Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
PUBLIC HEALTH / CLINICAL RESEARCH
Wellbeing of parents raising children with autism spectrum disorder and the role of psychologists
1
SDU University, Kaskelen, Kazakhstan
2
Asfendiyarov Kazakh National Medical University, Almaty, Kazakhstan
3
Al-Farabi Kazakh National University, Almaty, Kazakhstan
4
Lithuanian University of Health Sciences, Kaunas, Lithuania
Submission date: 2024-03-25
Final revision date: 2024-06-26
Acceptance date: 2024-07-03
Online publication date: 2024-07-28
Corresponding author
KEYWORDS
TOPICS
ABSTRACT
Introduction:
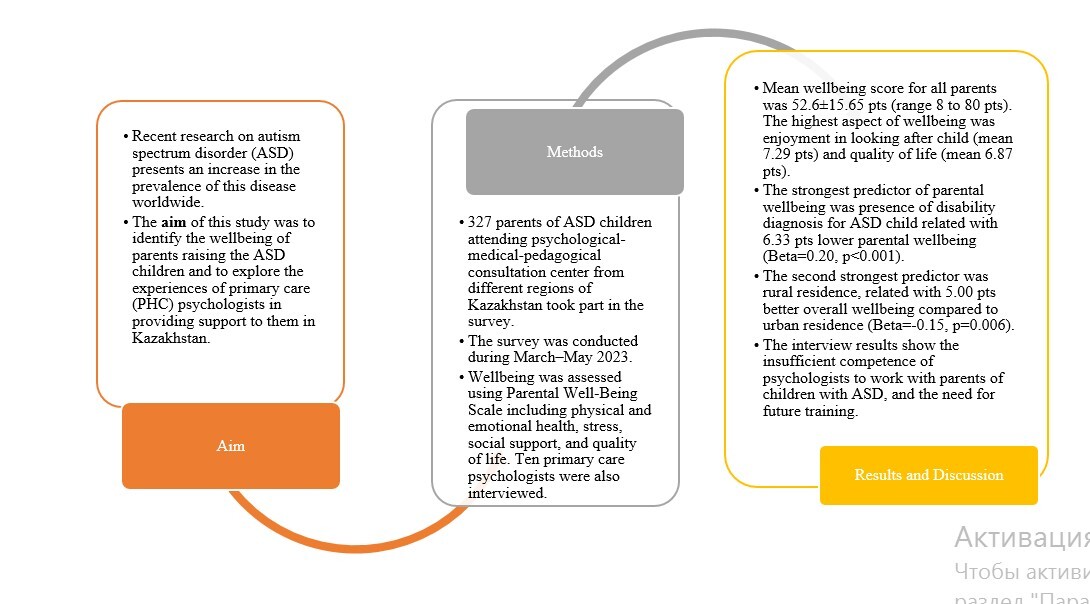
Recent research has shown a rise in the prevalence of autism spectrum disorder (ASD) worldwide. At the same time, care for ASD children was found to affect the psychological health of parents or guardians of ASD children. The aim of the study was to identify the wellbeing of parents raising ASD children and to explore the experiences of primary health care (PHC) psychologists in providing support to them.
Material and methods:
We conducted a cross-sectional study. Parents of ASD children took part in the survey. Wellbeing was assessed using the Parental Well-Being Scale including physical and emotional health, stress, social support, and quality of life. Ten primary care psychologists were also interviewed.
Results:
Three hundred and twenty-seven parents of ASD children participated in our study. The mean wellbeing score for all parents was 52.6 ±15.65 points. The highest scoring aspects of wellbeing were enjoyment in looking after the child (mean 7.29 points) and quality of life (mean 6.87 points). The strongest predictor of parental wellbeing was presence of a disability diagnosis for the ASD child (6.33 points), with lower parental wellbeing ( = 0.20, p < 0.001). The interview results show the insufficient competence of psychologists to work with parents of children with ASD.
Conclusions:
On the Parental Well-Being Scale, the highest scores were observed for enjoyment in looking after the child and quality of life. Insufficient work is carried out by PHC psychologists with parents of children with ASD. There is a need for future training of psychologists in the management of children with ASD and their parents.
Recent research has shown a rise in the prevalence of autism spectrum disorder (ASD) worldwide. At the same time, care for ASD children was found to affect the psychological health of parents or guardians of ASD children. The aim of the study was to identify the wellbeing of parents raising ASD children and to explore the experiences of primary health care (PHC) psychologists in providing support to them.
Material and methods:
We conducted a cross-sectional study. Parents of ASD children took part in the survey. Wellbeing was assessed using the Parental Well-Being Scale including physical and emotional health, stress, social support, and quality of life. Ten primary care psychologists were also interviewed.
Results:
Three hundred and twenty-seven parents of ASD children participated in our study. The mean wellbeing score for all parents was 52.6 ±15.65 points. The highest scoring aspects of wellbeing were enjoyment in looking after the child (mean 7.29 points) and quality of life (mean 6.87 points). The strongest predictor of parental wellbeing was presence of a disability diagnosis for the ASD child (6.33 points), with lower parental wellbeing ( = 0.20, p < 0.001). The interview results show the insufficient competence of psychologists to work with parents of children with ASD.
Conclusions:
On the Parental Well-Being Scale, the highest scores were observed for enjoyment in looking after the child and quality of life. Insufficient work is carried out by PHC psychologists with parents of children with ASD. There is a need for future training of psychologists in the management of children with ASD and their parents.
REFERENCES (42)
1.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: American Psychiatric Publishing 2013.
2.
Salari N, Rasoulpoor S, Rasoulpoor S, et al. The global prevalence of autism spectrum disorder: a comprehensive systematic review and meta-analysis. Ital J Pediatr 2022; 48: 112.
3.
Zeidan J, Fombonne E, Scorah J, et al. Global prevalence of autism: a systematic review update. Autism Res 2022; 15: 778-90.
4.
Schnabel A, Youssef GJ, Hallford DJ, et al. Psychopathology in parents of children with autism spectrum disorder: a systematic review and meta-analysis of prevalence. Autism 2020; 24: 26-40.
5.
McStay RL, Trembath D, Dissanayake C. Maternal stress and family quality of life in response to raising a child with autism: from preschool to adolescence. Res Dev Disabil 2014; 35: 3119-30.
6.
McConkey R. A brief measure of parental wellbeing for use in evaluations of family-centred interventions for children with developmental disabilities. Children (Basel) 2020; 7: 120.
7.
Rivard M, Terroux A, Parent-Boursier C, Mercier C. Determinants of stress in parents of children with autism spectrum disorders. J Autism Dev Disord 2014; 44: 1609-20.
8.
Sim A, Vaz S, Cordier R, et al. Factors associated with stress in families of children with autism spectrum disorder. Develop Neurorehabil 2018; 21: 155-65.
9.
Lee J, Barger B. Factors predicting poor mental and physical health in parents of children with autism spectrum disorder: results from 2016 to 2019 National Survey of Children’s Health. J Autism Dev Disord 2024; 54: 915-30.
10.
Li F, Tang Y, Li F, et al. Psychological distress in parents of children with autism spectrum disorder: a cross-sectional study based on 683 mother-father dyads. J Pediatr Nurs 2022; 65: e49-55.
11.
Zhang X, Kern ZG, Yun J. Physical activity and mental health of parents of children with autism spectrum disorder. Adapt Phys Activ Q 2023; 40: 649-63.
12.
Lai WW, Goh TJ, Oei TP, Sung M. Coping and well-being in parents of children with autism spectrum disorders (ASD). J Autism Dev Disord 2015; 45: 2582-93.
13.
Samadi SA, McConkey R, Bunting B. Parental wellbeing of Iranian families with children who have developmental disabilities. Res Dev Disabil 2014; 35: 1639-47.
14.
Somerton M, Stolyarova V, Khanin S. Autism and the knowledge and beliefs of specialists in Kazakhstan. J Autism Dev Disord 2022; 52: 1156-68.
15.
Order of the Minister of Health of the Republic of Kazakhstan dated October 23, 2020 No. KR DSM-149/2020. On approval of the rules for organizing the provision of medical care to persons with chronic diseases, frequency and duration of observation, mandatory minimum and frequency of diagnostic studies https://adilet.zan.kz/rus/docs... (Kazakh or Russian languages).
16.
Smith J, Sulek R, Abdullahi I, et al. Comparison of mental health, well-being and parenting sense of competency among Australian and South-East Asian parents of autistic children accessing early intervention in Australia. Autism 2021; 25: 1784-96.
17.
Samadi SA, McConkey R. Autism in developing countries: lessons from iran. Autism Res Treat 2011; 2011: 145359.
18.
Peiris H, Wickramarachchi DC, Samarasinghe P, et al. Diagnosing autism in low-income countries: clinical record-based analysis in Sri Lanka. Autism Res 2022; 15: 1358-67.
20.
Padden C, James JE. Stress among parents of children with and without autism spectrum disorder: a comparison involving physiological indicators and parent self-reports. J Dev Phys Disabil 2017; 29: 567-86.
21.
Alibekova R, Kai Chan C, Crape B, et al. Stress, anxiety and depression in parents of children with autism spectrum disorders in Kazakhstan: prevalence and associated factors. Glob Ment Health (Camb) 2022; 9: 472-82.
22.
Greenlee JL, Hickey E, Stelter CR, Huynh T, Hartley SL. Profiles of the parenting experience in families of autistic children. Autism 2023; 27: 1919-32.
23.
Dyches TT, Christensen R, Harper JM, Mandleco B, Roper SO. Respite care for single mothers of children with autism spectrum disorders. J Autism Dev Disord 2016; 46: 812-24.
24.
Nunnally AD, Factor RS, Sturm A, et al. Examining indicators of psychosocial risk and resilience in parents of autistic children. Front Behav Neurosci 2023; 17: 1102516.
25.
Di Renzo M, Guerriero V, Zavattini GC, Petrillo M, Racinaro L, Bianchi di Castelbianco F. Parental attunement, insightfulness, and acceptance of child diagnosis in parents of children with autism: clinical implications. Front Psychol 2020; 11: 1849.
26.
Losada-Puente L, Baña M, Asorey MJF. Family quality of life and autism spectrum disorder: comparative diagnosis of needs and impact on family life. Res Dev Disabil 2022; 124: 104211.
27.
Gowin E, Avonts D, Horst-Sikorska W, Dytfeld J, Michalak M. Stimulating preventive procedures in primary care. Effect of PIUPOZ program on the delivery of preventive procedures. Arch Med Sci 2012; 8: 704-10.
28.
Bispo-Torres AC, Lucena R, Tavares-Rodrigues IC, et al. Psychopathological symptoms in parents and siblings of people on the autism spectrum: a systematic review and meta-analysis. Psychiatry Res 2023; 323: 115145.
29.
Astana Times (2023). Kazakh Family Survey Explores Gender Roles, Institution of Fatherhood and Women’s Role in Preventing Corruption. https://astanatimes.com/2023/0....
30.
Bartholmae MM, Karpov MV, Dod RD, Dodani S. SilverCloud mental health feasibility study: who will it benefit the most? Arch Med Sci 2023; 19: 1576-80.
31.
Karst JS, Van Hecke AV. Parent and family impact of autism spectrum disorders: a review and proposed model for intervention evaluation. Clin Child Fam Psychol Rev 2012; 15: 247-77.
32.
Maughan AL, Lunsky Y, Lake J, et al. Parent, child, and family outcomes following acceptance and commitment therapy for parents of autistic children: a randomized controlled trial. Autism 2024; 28: 367-80.
33.
Croen LA, Qian Y, Ashwood P, et al. Family history of immune conditions and autism spectrum and developmental disorders: findings from the study to explore early development. Autism Res 2019; 12: 123-35.
34.
Sankey C, Derguy C, Clément C, Ilg J, Cappe É. Supporting parents of a child with autism spectrum disorder: the french awakening. J Autism Dev Disord 2019; 49: 1142-53.
35.
Clark M, Adams D. Listening to parents to understand their priorities for autism research. PLoS One 2020; 15: e0237376.
36.
State Healthcare Development Program “Densaulyk” for 2016 – 2019 Government of the Republic of Kazakhstan. Approved Government Decree No. 634, October 15, 2018.
37.
Turnage D, Conner N. Quality of life of parents of children with autism spectrum disorder: an integrative literature review. J Spec Pediatr Nurs 2022; 27: e12391.
38.
Khazhymurat A, Paiyzkhan M, Khriyenko S, et al. Health education competence: an investigation of the health education knowledge, skills and attitudes of nurses in Kazakhstan. Nurse Educ Pract 2023; 68: 103586.
39.
Riklefs V, Abakassova G, Bukeyeva A, et al. Transforming medical education in Kazakhstan: successful case of internationalization from Karaganda State Medical University. Med Teach 2018; 40: 481-7.
40.
Alshaigi K, Albraheem R, Alsaleem K, Zakaria M, Jobeir A, Aldhalaan H. Stigmatization among parents of autism spectrum disorder children in Riyadh, Saudi Arabia. Int J Pediatr Adolesc Med 2020; 7: 140-6.
41.
Kozhageldiyeva L, Kosherbayeva L, Sabyrdilda Z, Kaukenova A, Kurmanalina S. Perceptions regarding autism spectrum disorders among population of Kazakhstan. J Clin Med Kaz 2024; 21: 41-7.
42.
Gaziel-Guttman M, Anaki D, Mashal N. Social anxiety and shame among young adults with autism spectrum disorder compared to typical adults. J Autism Dev Disord 2023; 53: 2490-8.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.