Introduction
Ankle and foot injuries are the most common pediatric athlete injuries [1] with a prevalence of 2.15 per 1000 [2]. It was also reported that the prevalence was 0.7% and 0.4% for mild and severe chronic ankle instabilities (CAI) among males and 0.3% and 0.4% among females, respectively, whereas males had a 2.33-fold greater incidence of mild CAI than females [3]. Ankle sprains (AS) are the most frequent sports-related injuries among athletes and physically active individuals [2]. Individuals with a history of AS are more susceptible to chronic ankle instability [4]. The CAI can be presented as functional instability perceived as giving way, or as mechanical instability that results from ligamentous and pericapsular laxity [5]. Ankle instability (AI), limited mobility of the ankle joint, muscle weakness, and proprioceptor damage in the ankle ligaments are the most common risk factors reported. The injury results from overstretching the ligaments that support the ankle joint beyond their physiological limits, leading to damage of the ligaments fibrous integrity [6]. Incomplete healing of injuries in lateral ligaments of the ankle can lead to an increase in the accessory movements causing an enlargement of the neutral zone and an abnormal pattern of joint movement [7]. The injury does not solely affect the ligamentous integrity, but extends to include related joint structures. Recent ultrasonic evaluations reported the cross sectional area of the peroneus longus to be reduced in patients with lateral AS [8].
Functional ankle instability results in altered activation patterns of the lower limb proximal muscles reflected as significant differences in amplitude of proximal muscle activity with distal muscle activity during perturbation [9].
According to McKeon, lateral AS and CAI lead to muscle injury and peripheral neural structures, central neural inhibition and sensory reorganization, and neuromotor impairment providing impaired postural control and balance [10].
In addition, deficits in postural control resulting from impaired neuro-motor control and proprioception are commonly found in patients with CAI [11], whereas various balance-training programs were reported to improve postural control in patients with CAI [12].
Several treatment protocols were reported to improve ankle stability including proprioceptive [13], coordination [14], balance [15], strength, and virtual reality training [16].
Virtual reality (VR) gaming is a new technology, enhancing and providing multiple innovative interventions that require attention and active participation from patients [17]. It gives a chance to have interaction in multisensory activities that are almost like existence including hand skills, activities of daily living, manipulation, mobility, balance, and cognition [18]. The Nintendo Wii Fit Plus is a common designed VR used to improve balance and fitness while providing entertainment. It has a great impact on the improvement of functional performance by enhancing flexibility, balance, strength, and coordination training [19].
On the other hand, the Biodex balance training (BBT) system can improve the functional abilities of the neuro-musculoskeletal system by decreasing the malalignment of posture and improving spinal kinematics and balance control [20]. To date, several studies have been reported comparing VR and BBT in cases of AS, but to our knowledge, none has addressed adolescent athletes. Therefore, the purpose of this study was to compare the effect of virtual reality training (VRT) in the form of Wii Fit Plus games and BBT for ankle instability in adolescent athletes. It was hypothesized that there is a significant difference between the efficacy of VRT and BBT in rehabilitation of ankle instability in adolescent athletes.
Material and methods
Study design
A randomized controlled study was conducted in an outpatient private clinic, during the period from August 2018 to August 2020. An informed consent form was signed by the parent of each participant. Verbal assent was obtained from each participant in the presence of the parent or legal guardian. Procedures of our study had approval No. P.T.REC/012/002877 from the Institutional Ethical Committee Clearance of the Faculty of Physical Therapy, Cairo University, and had registration number NCT04592900 that was registered at Clinicaltrial.gov.
Confidentiality
All research procedures from the orientation to the actual application of the study were conducted in a closed room in the private outpatient clinic. We ensured that no one other than the investigators was present in the room during the study.
Declaration of interests
No interest other than the information gained and data obtained from participants for the research study.
Access to data
The participants’ personal data and information were saved in an Excel spreadsheet that was only accessible to the research investigators. The sheet was on the primary investigator’s computer that is secured by a password.
Ancillary and post-trial care
The study does not involve any physical, psychological or social risks. The study could be stopped if any unexpected symptoms were reported by the patients during treatment.
Dissemination policy
Reports and results were sent by email to each participant parent/guardian individually.
Participants
Ninety male football players who were diagnosed with AI based on a careful clinical evaluation were referred by qualified physicians of at least 10 years of experience and confirmed by an experienced physiotherapist of at least 10 years of experience as well.
The study inclusion was restricted to males who sustained a lateral ankle sprain of grade II, in the age range of 12–16 years (15.23 ±1.21), with a history of [21]:
At least one significant ankle sprain where:
A history of the previously injured ankle joint “giving way”, and/or recurrent sprain, and/or “feelings of instability”.
Participant also had to obtain a score of 24 or less according to the Cumberland Ankle Instability Tool (CAIT), and had a stable medical and psychological status as reported by the team physician. The authors excluded from the current study participants with grades I and III ankle sprain, ankle or foot deformity, back problems, or any musculoskeletal disorders; a history of previous surgery on the musculoskeletal structures (i.e., bones, joint structures, nerves) in either lower extremity, acute injury to musculoskeletal structures of other joints of the lower extremity in the previous 3 months that impacted joint integrity and function resulting in at least 1 interrupted day of desired physical activity, any disorder affecting balance, still receiving ankle physical therapy treatment, or did not have any previous exposure to exergaming (the activity of playing video games that involve physical exertion and are thought of as a form of exercise) [22]. Participants who did not commit to two successive sessions were also considered for exclusion.
Randomization
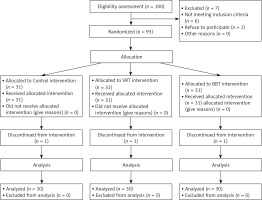
One hundred athletic adolescents with CAI were assessed for eligibility. Six did not meet our selected criteria, one did not agree to enroll, and three dropped out from post-assessment. Ninety children were assigned randomly to three groups of equal numbers. Randomization was limited to different sizes of permuted blocks to ensure the allocation of equal numbers in each group. Each random permuted block was stored in a drawer locked until required in the form of sealed consecutive sequence, numbered, opaque envelopes. After the formal inclusion of each participant in the trial and in the presence of the patient’s parent, the next envelope was opened by the researcher in sequence. All participants were blinded to the study hypothesis. A randomization diagram of participants is shown in Figure 1.
Outcome measures
Primary: CAIT
It is a self-reporting scale that assesses the degree of AI. It consists of 30 points of a total of nine items. Recording at least a 28-point score is defined as a subject having a normal ankle, while those with a point score of 24 or less are defined as subjects having functional ankle instability (FAI). A higher score indicates greater ankle stability [23].
CAIT is reported as a simple, valid, and reliable tool to assess the severity of functional ankle instability. The CAIT score threshold was reported as 27.5 (Youden index, 68.1) with sensitivity of 82.9% and specificity of 74.7%. Test-retest reliability was excellent; ICC(2,1) = 0.96 [24].
All measurements were collected at the baseline and after 3 months of treatment.
Secondary: Postural stability
The Biodex Balance System (BBS) SD (Model 950-441) is an important therapeutic tool used for the assessment and training of patients with deficits in balance [25]. The BBS is a reliable and valid device used to evaluate the participant’s ability to maintain static and dynamic balance stability on the unstable tilting platform; clinicians can evaluate postural control by measuring the ability to maintain dynamic unilateral and bilateral posture stability on the unstable surface. During the posture stability test, we evaluate the variance from the center by measuring the ability of the participant to control the platform’s angle of tilt [26]. A dynamic balance test was performed on stability level eight according to a prior pilot study. The outcome measures were: the overall stability index (OASI), which refers to the ability of the participant to maintain his balance in all directions; the antero-posterior stability index (APSI), which refers to the participant’s ability to maintain his balance from forward to backward direction; and the medio-lateral stability index (MLSI), which refers to the ability of the participant to maintain his balance from side-to-side directions. High values indicate that the participant had difficulty.
The Biodex stability system is actually a movable platform with variable degrees of instability (static, from 1 to 12). The platform can be tilted up to twenty degrees of surface tilt from horizontal in all directions. It has a foot grid for determination of foot position before testing. It has 12 stability levels. Stability level 12 is the most stable platform surface, whereas stability level 1 is the most unstable platform surface [27].
Intervention
Intervention was provided individually in a face-to-face mode of delivery by a therapist with at least 15 years of clinical experience in ankle and foot rehabilitation.
The Biodex was chosen based on being the most widely used in our region as well as based on its validity, reliability and ease of use. Meanwhile, the Wii Fit was chosen since active video gaming has become an emerging trend in fitness, education and health sectors [22]. It was also reported as a safe and feasible adjunct to physiotherapy [28], increasing activity levels, vitality and well-being while being fun [29].
In addition, it can be used independently at home, especially during a pandemic [30].
Proprioceptive training was based on the participant’s ability to maintain a single-limb stance while performing various tasks. The exercise sequence was (1) hop to stabilization, (2) hop to stabilization and reach, (3) hop-to-stabilization box drill, (4) progressive single-limb stance activities with eyes open, and (5) progressive single-limb stance activities with eyes closed. Each participant progressed to the next level only after completing the previous level without faults. Faults were considered when touching down with the contralateral limb, trunk bending more than 30° to either side, removing the hands from the hip level during hands-on-hips exercises, bracing the non-weight-bearing extremity against the weight-bearing one, or missing the target.
Thera Band resistance was also used to strengthen plantar flexors, dorsiflexors, invertors, and evertor muscles. Additional balance exercises were performed by perturbation on a slide board, Airex Balance Pad, trampoline, and donut hall [32].
– The VR group received 30 min of the same guideline protocol in addition to 30 min VR. Nintendo Wii Fit Plus is one of the most common home-based interactive video games (IVG), consisting of a wireless handheld pointing device, the detection of movement and acceleration being in three dimensions by a motion sensor attached to a television. The virtual image is seen on the television screen that mimics the participant’s movements. These games encourage the interaction of participants to play repetitively [33]. The strength and balance exercises were carefully selected by physical therapists to provide an optimum effect.
– The guideline of the VRT protocol was timed and calculated by the program and displayed on the screen. The program included: lunge, single leg extension, sideways leg lift, single leg twist, and rowing squat as strength exercises; and soccer heading, tight rope walks, ski slalom, table tilt, and snowboard slalom as balance exercises [16].
– The BBT group received 30 min of the same guideline protocol of assessment of balance on the BBS [34].
– All participants received treatment three times/week for 3 consecutive months.
Sample size
To determine the required number of subjects needed in this study, estimates of mean and standard deviation were collected from a pilot study consisting of 10 patients who received the same program between June 1, 2018 and July 30, 2018. The mean differences and standard deviation of the CAIT score were estimated as 0.52 and 3.4, respectively, from this pilot study. These findings are consistent with Wright et al. [35], who identified the minimal detectable change (MDC) and minimal clinically important difference (MCID) as 3.08 and > 3 respectively. According to these figures, at least 25 participants per group, given a significance level of 5% and statistical power of 80%, were needed in the current study. To account for possible participant drop-outs, the sample size was increased by 20%. Calculations were performed using the ps power and sample size calculation computer program available online from the Vanderbilt Medical Center (www.mc.vander-bilt.edu). The sample size was based on the expected difference in the primary outcome variable between the groups at post-test only.
Statistical analysis
The data were screened before the final analysis to test the normality assumption by using the Shapiro-Wilk test, which reflects normal distribution (p > 0.05). Additionally, Levene’s test was used to testing the homogeneity of variance, which revealed no significant difference (p > 0.05). Since data were normally distributed, parametric analysis was used. The SPSS package program version 25 for Windows (SPSS, Inc., Armonk, NY: IBM Corp) was used. All data were expressed as mean and standard deviation for demographic data, balance measurement, and ankle instability measurement. A mixed design 3 x 2 MANOVA-test was used to compare the tested variables in different groups and measuring periods. The first independent variable (between-subject factors) was the tested group with 3 levels (control group, VR group, and BBT group). The second independent variable (within-subject factor) was the testing time before and after treatment. The four dependent variables were the OASI, APSI, MLSI, and CAIT. The Bonferroni correction test was used to compare between pairs of groups for post-treatment of the tested variables whose F-value was significant in the MANOVA test. The significance level was set at p ≤ 0.05.
Results
Ninety patients participated in this study and were distributed randomly as 30 patients in each group. No significant differences in age, weight, height, and BMI were found among the three groups (Table I).
Table I
Comparison of mean values of demographic data among three groups
Multivariate tests by 3 x 2 mixed design MANOVA for outcome measures presented statistically significant (p < 0.05) effects due to main effects of tested groups (F17.487; p = 0.0001; partial η2 = 0.290), measurement time (F = 225.796; p = 0.0001; partial η2 = 0.841), and group x time interaction (F = 342.00; p = 0.0001; partial η2 = 0.245).
The statistical analysis within each group (Table II) revealed a significant (p < 0.05) decrease in OASI, APSI, and MLSI at post-treatment compared to pre-treatment within the control, VR, and BBT groups. Measurement of the ankle instability (CAIT) significantly (p < 0.05) increased at post-treatment compared to pre-treatment within the control group, VR group, and BBT group. Both the VR group and the BBT group revealed more improvement in postural balance and CAIT than the control group.
Table II
Comparison by MANOVA test for all measured dependent variables within and among three groups
| Variables | Groups (mean ± SD) | P-value | ||
|---|---|---|---|---|
| Control group (n = 30) | VR group (n = 30) | BBT group (n = 30) | ||
| OASI: | ||||
| Pre-treatment | 2.41 ±0.31 | 2.35 ±0.28 | 2.30 ±0.37 | 0.405 |
| Post-treatment | 2.01 ±0.42 | 1.22 ±0.19 | 1.16 ±0.26 | 0.0001* |
| Mean difference | 0.40 | 1.13 | 1.14 | |
| Improvement % | 16.60 | 48.09 | 49.57 | |
| P-value | 0.0001* | 0.0001* | 0.0001* | |
| APSI: | ||||
| Pre-treatment | 1.61 ±0.19 | 1.55 ±0.16 | 1.60 ±0.28 | 0.469 |
| Post-treatment | 1.24 ±0.27 | 0.77 ±0.13 | 0.78 ±0.18 | 0.0001* |
| Mean difference | 0.37 | 0.78 | 0.82 | |
| Improvement % | 22.98 | 50.32 | 51.25 | |
| P-value | 0.0001* | 0.0001* | 0.0001* | |
| MLSI: | ||||
| Pre-treatment | 1.45 ±0.36 | 1.41 ±0.31 | 1.39 ±0.39 | 0.850 |
| Post-treatment | 1.29 ±0.63 | 1.08 ±0.50 | 1.10 ±0.50 | 0.027* |
| Mean difference | 0.16 | 0.33 | 0.29 | |
| Improvement % | 11.03 | 23.40 | 20.90 | |
| P-value | 0.024 | 0.004* | 0.014* | |
| CAIT: | ||||
| Pre-treatment | 18.50 ±1.49 | 18.28 ±1.10 | 18.31 ±2.50 | 0.871 |
| Post-treatment | 19.89 ±1.54 | 22.55 ±1.36 | 22.93 ±3.13 | 0.0001* |
| Mean difference | 1.39 | 3.97 | 4.62 | |
| Improvement % | 7.51% | 21.72% | 25.23% | |
| P-value | 0.001* | 0.0001* | 0.0001* | |
The statistical analysis between the 3 groups (Table II) showed no significant differences (p > 0.05) in mean values of pre-treatment OASI, APSI, MLSI, and CAIT. However, there were significant differences (p < 0.05) in the mean values of post-treatment OASI, APSI, MLSI, and CAIT between the three groups.
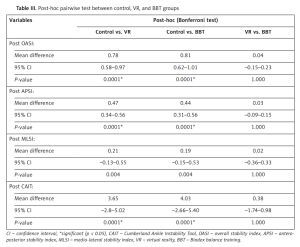
From post-hoc test comparisons (Table III), there was a significant difference (p < 0.05) between the control and VR groups, control, and BBT groups, whereas no significant differences were found (p > 0.05) between VR and BBT groups for measurements of balance and CAIT.
Table III
Post-hoc pairwise test between control, VR, and BBT groups
| Variables | Post-hoc (Bonferroni test) | ||
|---|---|---|---|
| Control vs. VR | Control vs. BBT | VR vs. BBT | |
| Post OASI: | |||
| Mean difference | 0.78 | 0.81 | 0.04 |
| 95% CI | 0.58–0.97 | 0.62–1.01 | –0.15–0.23 |
| P-value | 0.0001* | 0.0001* | 1.000 |
| Post APSI: | |||
| Mean difference | 0.47 | 0.44 | 0.03 |
| 95% CI | 0.34–0.56 | 0.31–0.56 | –0.09–0.15 |
| P-value | 0.0001* | 0.0001* | 1.000 |
| Post MLSI: | |||
| Mean difference | 0.21 | 0.19 | 0.02 |
| 95% CI | –0.13–0.55 | –0.15–0.53 | –0.36–0.33 |
| P-value | 0.004 | 0.004 | 1.000 |
| Post CAIT: | |||
| Mean difference | 3.65 | 4.03 | 0.38 |
| 95% CI | –2.8–5.02 | –2.66–5.40 | –1.74–0.98 |
| P-value | 0.0001* | 0.0001* | 1.000 |
Discussion
The current trial aimed to compare the efficacy of VR and BBT in the treatment of CAI in adolescent athletes. The results of the trial showed a significant decrease in OASI, APSI, and MLSI as well as a significant increase in CAIT within both groups. However, there was no significant difference between the VR and BBT groups with regards to the outcomes of the rehabilitation for athletic adolescents with CAI.
As reported earlier, ankle sprains are common in young athletes, representing up to 30% of all sports injures [36]. This is supported by the previous finding that adolescents were at greater risk of AS than adults [37]. Consequently, CAI could affect the performance of young athletes in daily life activities.
The current findings revealed significant improvement in stability indices. This is in agreement with previous research reporting balance deficits due to impairments in proprioception and neuromuscular control [5, 38, 39]. Decreased balance in the pre-treatment assessment of all participants was directly related to the diagnosis of AS; this supports the fact that AS leads to deficits in proprioception and affects balance by increasing body sway [40]. In addition, a deficit in ROM of ankle dorsiflexion secondary to (AS) could potentially affect dynamic balance in individuals with CAI [10].
Since the balancing process requires coordination of multiple motor, sensory, and biomechanical components [41], it is considered an essential component of precise and functional interaction with the surrounding environment.
This explains the within-group improvements following both balance training [32, 42, 43] and conventional physiotherapy [12, 44, 45].
Additionally, this study utilized the CAIT as a reliable tool that has been widely used to assess FAI [46]. The results of the current study showed that there was a significant increase of CAIT score in the post-assessment mean values as compared to pre-assessment mean values in all groups. These results are similar to the findings of O’Driscoll et al., indicating significant improvement in CAIT score after 6 weeks of VR training in functional ankle instability; thus, increasing the CAIT score via intervention may have considerable significance to reduce FAI [47].
The results of the current study also showed a significant decrease in post-treatment mean values of OASI, APSI, and MLSI in the control group that received a traditional program. This is attributed to the reported positive impact of conventional physiotherapy (proprioceptive training) on the improvement of balance in patients with functional AI reducing recurrent ankle sprains [48].
Regarding virtual training, VR games such as Nintendo Wii Fit Plus have a low cost and could be available in the department of physiotherapy in many developing countries. It has great benefits in the rehabilitation process in areas with limited resources. The Interactive Rehabilitation Exercise System is an expensive and inaccessible VR system for the majority of the population. Therefore, it is becoming popular to use mainstream game consoles for treatment [49].
The current findings revealed a significant improvement in the VR group mainly in APSI. This reflects an increased dorsiflexion and plantar flexion (DF/PF) strength ratio [50].
According to Coughlan, & Caulfield, VR in the form of Wii Fit Plus training is considered neuromuscular training involving balanced exercises and closed chain exercises which has a positive impact on balance in athletic patients [11]. It was concluded that Wii exercises had a great impact on improving muscle strength and balance (i.e., static, and dynamic balance) in patients with functional AI [11, 16, 32].
Similarly, improvement in means values of the stability indices OASI, APSI, and MLSI in the BBT group may be attributed considering BBT as a form of closed kinetic chain exercises that can stimulate muscle and joint mechanoreceptors and facilitate agonists and antagonists’ co-contraction that help to regain balance, postural control and produce better functional joint stability [42, 51].
Comparison of mean values of the stability index between conventional therapy and VR training showed significant improvement of all stability indices – OASI, APSI, and MLSI – in favor of VR, similar to previous findings revealing significant improvement of static and dynamic balance in subjects with functional ankle instability [16].
Comparison of mean values of the stability index between conventional therapy and BBT training showed significant improvement of all stability indices – OASI, APSI, and MLSI – in favor of BBT. Similar findings were also reported by Rozzi et al., who concluded that BBT is an effective way to improve proprioception of joint and ability of subjects with AI to stand on a single leg [27].
The present study showed that there was no significant difference in the post-treatment mean values of the stability index between the VR group and BBT group. Our findings are in agreement with Khalil et al., who reported that there was no significant difference between the VR group and BBT group after 4 weeks of training in normal adults [50].
The current findings did not agree with Punt et al., who found no significant difference between the Wii Fit Plus exercise as a form of VR and conventional physical therapy programs in patients with an ankle sprain [52]. Also, Vernadakis et al. concluded that there was no significant difference in all stability index variables between VR and conventional therapy [53]. We believe the disagreement in the findings may be due to the difference in the population age as well as the duration of applying the intervention.
This study was conducted only on male participants; thus it did not consider the effect of gender.
Further studies are required to evaluate the efficacy of application for longer durations and allowing a follow-up period to ensure our statistical findings over time. We also recommend repeating the study on adolescent female athletes to reveal any possible gender differences in the relevant outcomes.
In conclusion, the findings of our study showed that both VR and BBT have an evident therapeutic effect on improving the degree of balance in cases of CAI in adolescent athletes but with no significant difference observed between VR and BBT during the rehabilitation of athletic adolescents with CAI.