Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
GASTROENTEROLOGY / CLINICAL RESEARCH
Treatment of Barrett’s esophagus with radiofrequency ablation
1
Department of Gastroenterology and Hepatology, University Clinical-Hospital Centre Zemun-Belgrade, Belgrade, Serbi
2
Clinic for Gastroenterology and Hepatology, Faculty of Medicine, University of Belgrade, Clinical Centre of Serbia, Belgrade, Serbia
3
Clinic for Surgery, Faculty of Medicine, University of Belgrade, Clinical Centre of Serbia, Belgrade, Serbia
4
Department of Radiobiology and Molecular Genetics, VINČA Institute of Nuclear Sciences – National Institute of the Republic of Serbia, University of Belgrade, Belgrade, Serbia
Submission date: 2022-11-14
Final revision date: 2023-01-09
Acceptance date: 2023-01-14
Online publication date: 2023-01-27
Corresponding author
Esma R. Isenovic
Department of Radiobiology and Molecular Genetics, VINČA Institute of Nuclear Sciences - National Institute of the Republic of Serbia, University of Belgrade, P.O.Box 522, 11001, Belgrade, Serbia
Department of Radiobiology and Molecular Genetics, VINČA Institute of Nuclear Sciences - National Institute of the Republic of Serbia, University of Belgrade, P.O.Box 522, 11001, Belgrade, Serbia
KEYWORDS
TOPICS
ABSTRACT
Introduction:
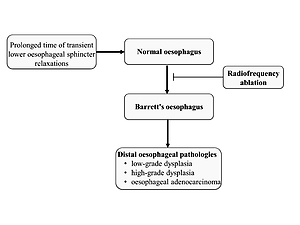
Barrett’s esophagus (BE) represents the distal esophageal epithelium changes that carry a high risk of developing esophageal adenocarcinoma. One of the most challenging aspects of diagnosing BE by endoscopy is precisely discerning between normal epithelium and BE changes, which is essential for therapy success. The objectives of this study were to compare the success of radio-frequency ablation (RFA) therapy to conservative treatment with proton pump inhibitor (PPI) drugs between the clinical presentation and endoscopy findings of BE at 2, 6, 12, and 24 months after administered therapy.
Material and methods:
Seventy-five subjects were divided into two groups (RFA and PPI) based on the BE treatment regimen in this case-control study to compare the quality of treatments applied over a 24-month follow-up. Subjects who received RFA therapy were further divided into groups: those who received focal HALO 90 and those who received circumferential HALO 360, based primarily on EGDS findings or endoscopist experience.
Results:
The results show that using the RFA therapeutic modality in the treatment of BE is more effective (by 94.2% in the second month of follow-up, i.e., by 99% at the final visit after 24 months) than using PPI therapy alone. Re-RFA therapy was given to 15% of the subjects, mostly applied in the same therapeutic modality (HALO 90).
Conclusions:
Our findings show that RFA and re-RFA therapy have a high efficacy and safety profile, with no registered worsening of histology findings, the occurrence of esophageal adenocarcinoma, or adverse effects of the therapy.
Barrett’s esophagus (BE) represents the distal esophageal epithelium changes that carry a high risk of developing esophageal adenocarcinoma. One of the most challenging aspects of diagnosing BE by endoscopy is precisely discerning between normal epithelium and BE changes, which is essential for therapy success. The objectives of this study were to compare the success of radio-frequency ablation (RFA) therapy to conservative treatment with proton pump inhibitor (PPI) drugs between the clinical presentation and endoscopy findings of BE at 2, 6, 12, and 24 months after administered therapy.
Material and methods:
Seventy-five subjects were divided into two groups (RFA and PPI) based on the BE treatment regimen in this case-control study to compare the quality of treatments applied over a 24-month follow-up. Subjects who received RFA therapy were further divided into groups: those who received focal HALO 90 and those who received circumferential HALO 360, based primarily on EGDS findings or endoscopist experience.
Results:
The results show that using the RFA therapeutic modality in the treatment of BE is more effective (by 94.2% in the second month of follow-up, i.e., by 99% at the final visit after 24 months) than using PPI therapy alone. Re-RFA therapy was given to 15% of the subjects, mostly applied in the same therapeutic modality (HALO 90).
Conclusions:
Our findings show that RFA and re-RFA therapy have a high efficacy and safety profile, with no registered worsening of histology findings, the occurrence of esophageal adenocarcinoma, or adverse effects of the therapy.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.