Introduction
Cardiovascular disease (CVD) is still a leading cause of death in Poland and across Europe [1]. Diabetes mellitus (DM) is a main risk factor for coronary artery disease (CAD) [2], which is associated with a more complex multivessel CAD [3] and worse clinical prognosis [4]. Therefore patients with CAD and DM require optimal medical therapy and high rates of treatment goal attainment [5]. Despite recent progress in methods of invasive treatment of CAD and its better availability [6], the 1-year mortality rate following myocardial infarction is still relatively high – 10% [7, 8]. Several studies and registries suggest that more efforts should be made to improve secondary CVD prevention to achieve better control of risk factors and lifestyle modifications [9–12].
The European Society of Cardiology (ESC) published guidelines on CVD prevention in clinical practice in 2016 [5] promoting clinical recommendations and providing target treatment goals. The available data on the recent efficacy of secondary prevention in Poland are scarce and limited to single measures. Therefore, the aim of our study was to provide a comprehensive assessment of the attainment of main treatment goals in secondary prevention in coronary patients with or without DM.
Material and methods
POLASPIRE was a multicenter, cross-sectional study performed among Polish patients from 4 geographical areas (Krakow, Katowice, Bialystok, Warszawa) and 14 departments of cardiology representing various reference levels, including departments within medical universities and secondary care hospitals. The study had two parts performed independently in all departments (2017–2018): retrospective identification of patients (eligibility criteria) from hospital discharge lists of 14 departments and a prospective visit of study patients performed in leading centers of 4 geographical regions. All consecutive patients, men and women (≥ 18 years and < 80 years of age at the time of their index event or procedure) hospitalized more than 6 months earlier in one of the 14 departments for acute myocardial infarction, unstable angina, elective percutaneous coronary intervention (PCI) or coronary artery bypass surgery (CABG) were identified and invited for a study visit. The aim was to obtain prospective survey data on at least 200 patients in each geographical area using similar standardized methods and instruments according to the manufacturer’s manual in all centers. All parts of the study were performed by centrally trained research staff. Retrospective data regarding demographic information, clinical diagnoses, CV diseases and risk factors or laboratory tests were obtained from medical records. The study visit provided updated data on CV risk factors, attainment of treatment goals, medications and lifestyle. The visit included an interview with a patient using a detailed questionnaires of the European Action on Secondary Prevention through Intervention to Reduce Events (EUROASPIRE V) registry translated and validated for Poland. Additional available medical records were used for information on CV risk factors and current treatment. Moreover, the following measurements were performed during the visit: office blood pressure (mean value from two measurements), height and weight, waist circumference. Fasting venous blood was drawn for serum glycated hemoglobin (HbA1c), total cholesterol (TCH), high-density lipoprotein (HDL-C), triglycerides (TG) and low-density lipoprotein (LDL-C) was calculated according to Friedewald’s formula [13]. Definitions of risk factors and target treatment goals were based on the 2016 European Society of Cardiology guidelines on CVD prevention [5].
The diagnosis of dyslipidaemia was defined as abnormal plasma lipid levels (TCH > 190 mg/dl, LDL cholesterol > 115 mg/dl, TG > 150 mg/dl, HDL cholesterol < 40 mg/dl in men and < 50 mg/dl in women) or prior diagnosis and/or treatment [14]. Overweight was defined as a body mass index (BMI) ≥ 25 < 30 kg/m2 and obesity as a BMI ≥ 30 kg/m². Waist circumference (WC) was measured using a tape applied at the point midway in the mid-axillary line between the lowest rim of the rib cage and the superior iliac crest of the patient standing. Abdominal overweight was defined as a WC of ≥ 80 cm for women and ≥ 94 cm for men. Arterial hypertension was defined as systolic blood pressure (SBP) ≥ 140 mm Hg and/or diastolic blood pressure (DBP) ≥ 90 mm Hg. Smoking was defined at the time of interview and physical activity was estimated in an interview-based questionnaire. Chronic kidney disease was included in the patient’s characteristics based on a prior diagnosis and/or treatment on the retrospective discharge list from the index hospitalization [15]. Total cholesterol, HDL-C and TG were analyzed in serum, and HbA1c in whole blood. The main aim and the outcome measure of this analysis was the rate of patients with IHD and DM (known and treated since the index hospitalization) achieving the lifestyle, risk factors and therapeutic targets in comparison with individuals with IHD and not known DM. The study group was divided into two subgroups with (DM+) and without known DM (DM–) based on the retrospective medical records, including the discharge hospital documents (diagnosis and/or treatment).
The following goals were defined according to the 2016 guidelines [5]: controlled DM (HbA1c < 7.0%), lipid primary (LDL < 70 mg/dl) and secondary goal (non-HDL < 100 mg/dl), normal blood pressure (SBP < 140 and DBP < 90 mm Hg for all), normal BMI (20.0–25.0 kg/m), normal WC (women < 80 cm or men < 94 cm), smoking abstinence and regular physical activity with an equivalent of at least intensive activity for 20 min twice a week. The total number of attained goals was the sum of the above defined. An additional result for the attainment of BP target < 140/85 mm Hg was provided in the group with DM.
The coordinators of 4 geographical areas were responsible for obtaining Local Ethics Committees approvals and a written informed consent form was obtained from all the participants and stored in the patient’s file.
Statistical analysis
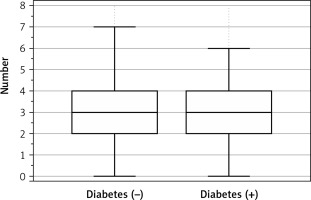
All results presented in the text, tables and figures are expressed as means ± standard deviation or number and percentage. Figure 1 is the exception and presents a box-and-whisker plot with medians, interquartile range and extreme values. The normality of distributions was analyzed using the Kolmogorov-Smirnov test. Baseline clinical parameters and the measures were compared between the subgroups using the t-tests for normally distributed continuous variables (Student’s t-test); in case of non-normal distribution, the Mann-Whitney U test was used. The Pearson χ2 test was applied to all categorical variables. A value p < 0.05 was considered statistically significant. Statistical analysis was undertaken using MedCalc software (version 19.0.5, Belgium).
Figure 1
Total number of the main therapeutic goals attained. Box-and-whisker plot showing median, interquartile range (1st and 3rd quartiles) and extreme values. Therapeutic goals: low-density lipoproteins cholesterol < 70 mg/dl; non-high-density lipoprotein < 100 mg/dl, smoking abstinence, blood pressure < 140/90 mm Hg, regular physical activity = at least 20 min twice a week of intensive activity, normal body mass index = 20.0–25.0 kg/m2, normal waist circumference – women < 80 cm or men < 94 cm
Results
Clinical characteristics in patients with and without diabetes mellitus
The study group included 1026 patients (65.5 ±9 years old, male/female: 72%/28%), who accepted the invitation for the interview and the examination > 6 months after the index hospitalization for acute myocardial infarction (39%), unstable angina (22%), elective percutaneous coronary intervention (35%) or coronary artery bypass surgery (4%). The study group represented a population of a very-high CV risk with several risk factors: dyslipidemia (100%), hypertension (81%), DM (32%), overweight (42.5%), obesity (43%) and active tobacco smoking (31%). Patients with known DM at the index hospitalization were included in the DM(+) group.
Patients DM(+) (n = 332; 32%) were slightly older compared to DM(–) individuals (67.2 ±7 vs. 64.6 ±9 years; p < 0.0001) with similar gender distribution (p = ns). Most patients with DM used oral antihyperglycemic medications (79%) with a minority treated with insulin (10%) or both (11%). The mean number of antihypertensive drugs was significantly increased in patients with DM (DM+ 2.93 ±0.66 vs. DM– 2.54 ±0.8; p < 0.0001). The clinical characteristics of the study group based on the retrospective hospital discharge list and medical records with the lipid-lowering treatment are presented in Table I.
Table I
Clinical characteristics of study patients with and without diabetes mellitus
There were 44 patients (6.3%) with undiagnosed DM (no DM or antihyperglycemic agents in medical records of the index event). Most of them (41) were diagnosed with DM in the outpatient clinics (oral glucose tolerance test or fasting plasma glucose) and were given oral antihyperglycemic drugs. Moreover, 246 patients (35%) in the DM(–) group had increased fasting plasma glucose at the prospective study visit suggestive of impaired fasting glucose.
Treatment goal attainment
The follow-up visit showed that patients with DM had significantly higher SBP, BMI, WC, TG and lower LDL-C and HDL-C compared to individuals without DM (Table II).
Table II
Clinical assessment on follow-up visit in patients with and without diabetes mellitus
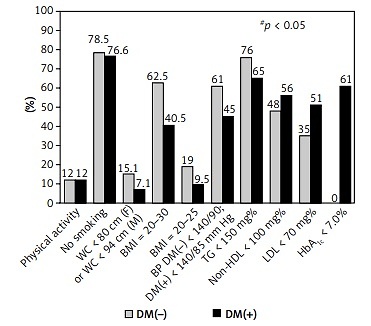
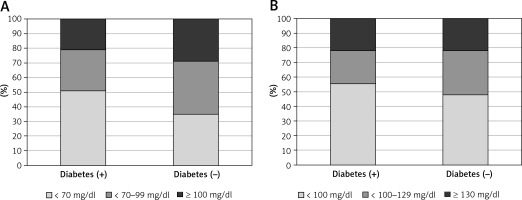
The attainment of particular treatment goals is shown in Figure 2. In brief, the glycemic goal was achieved in 196 patients (60%) (Figure 3). The rates of primary (LDL-C: 51% vs. 35%; p < 0.0001) and secondary (non-HDL-C: 56% vs. 48%; p < 0.02) lipid goal attainment were higher in DM(+) compared to DM(–) patients, but they had a smaller proportion of normal TG levels (65% vs. 76%; p < 0.001) (Figure 4). The rate of blood pressure < 140/90 mm Hg was lower in DM(+) than in normoglycemic patients (52% vs. 61%; p < 0.01). When the recommended target for patients with DM was used (< 140/85 mm Hg), the rate of target BP in the DM group was even lower (45%). As expected, goal achievement of normal weight (9.5% vs. 19%; p < 0.0001) and waist circumference (7% vs. 15%; p < 0.001) were lower in diabetic patients. The rate of individuals with regular physical activity was similar and low (DM(+): 12% vs. DM(–): 14%; p = ns). Finally, the proportions of active smokers were comparable but unacceptably high in both groups (DM(+): 23% vs.. DM(–): 22%; p = ns) (Figure 2).
Figure 3
Diabetes control: HbA1c in patients with diabetes mellitus with the relative frequency in the study group
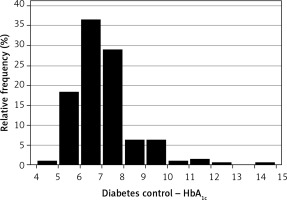
Figure 4
Proportion of patients with and without diabetes mellitus reaching different target goals of low-density lipoprotein cholesterol (A) and non-high-density lipoprotein cholesterol (B)
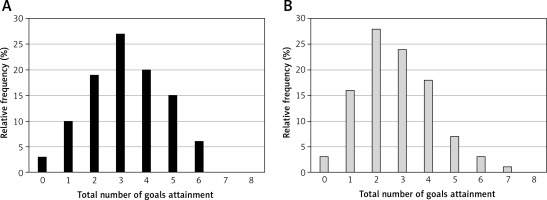
The total number of achieved goals was similar between both subgroups (DM(+): 2.56 ±1.3 vs. DM(–): 2.6 ±1.2; p = 0.6) (Figure 1). However, there was a small difference in total goal achievement among male patients (DM(+): 2.97 ±4.7 vs. DM(–): 2.77 ±1.4; p < 0.001) with no differences between female groups (DM(+) 2.55 ±3.2 vs. DM(–) 2.54 ±1.2; p = 0.9).
Figure 5 presents rates of patients of both groups reaching particular number of treatment goals.
Figure 5
Total number of therapeutic goals attained in patients with (A) and without (B) diabetes mellitus. Therapeutic goals: low-density lipoproteins cholesterol < 70 mg/dl; non-high-density lipoprotein < 100 mg/dl, smoking abstinence, blood pressure< 140/90 mm Hg, regular physical activity = at least 20 min twice a week of intensive activity, normal body mass index = 20.0–25.0 kg/m2, normal waist circumference – women < 80 cm or men < 94 cm and HbA1c < 7.0% for patients with diabetes mellitus
Most patients with DM reported having a regular glucose check-up (88%) and a regular BP measure (DM+: 91% vs. DM–: 81%; p < 0.05). Only one-third of patients reported following a specific lipid-lowering diet (DM+: 33% vs. DM–: 28%; p < 0.05). The particular lipid-lowering treatment is presented in Table I. The proportion of patients who were able to quit smoking just after the index event was higher in the DM(–) group (DM+: 28.5% vs. 36.6%; p < 0.05).
The proportion of patients who attempted to attain their weight was higher in DM patients (DM(+): 67.8% vs. DM(–): 60%; p = 0.01) and that of individuals who attempted to lose weight was similar in both groups (DM(+): 37.6% vs. DM(–): 33%; p = 0.15). The proportion of patients reporting engagement in physical activity aimed at weight loss was low and similar between both subgroups (DM(+): 21% vs. DM(–): 20.5%; p = 0.85).
Discussion
Our study of goal attainment in coronary patients with or without DM provided several important findings. First, despite a very high CV risk, the mean number of achieved goals was low in patients with and without DM. Second, diabetic or lipid goals revealed moderate rates of attainment in subjects with DM. Third, BMI, WC and physical activity revealed poor control, especially in DM patients. Fourth, about 6% (44 patients) of participants had previously undetected DM. Finally, drug therapies of dyslipidemia and DM are not optimal and need to be improved.
We present the most recent and comprehensive findings on the attainment of therapeutic goals in Polish patients since the ESC 2016 guidelines [5].
Our study sample was a relatively large group of patients with myocardial infarction or PCI as major index events. Patients with DM constituted one third of all individuals, with slightly higher mean age, similar gender distribution and significantly increased rates of obesity and CKD compared to non-DM patients. The great majority of patients with DM were treated with oral antihyperglycemic medication, but the target HbA1c was reached in only 60%. Twenty-nine percent of all participants in the recent EUROASPIRE-V registry (EAV) [9] had DM with a higher rate in insulin treatment (EAV: 32%) and slightly lower rate of patients with HbA1c target (54%).
There were 6.3% of patients with undetected DM during the index event hospitalization, which was mostly diagnosed in ambulatory outpatients. This screening failure was a cause of delay in diagnosis and more intensive treatment or lifestyle modifications. Moreover, one-third of patients in the DM(–) group had increased fasting plasma glucose at the prospective visit, suggesting a pre-diabetes state. This is even more interesting and important as those individuals would need intensive lifestyle modification to prevent or delay development of DM. Given that most patients in both groups had overweight or obesity and did not reach the recommended physical activity target, it is very probable that a considerable number of those patients will develop DM in the future. Undetected pre-diabetes or DM is quite common in patients with IHD [16] and it is associated with an unfavorable prognosis [17]. HbA1c is a test historically used for glycemic control, which helps to identify individuals with increased risk of microvascular complications [18].
The target BP was achieved in less than half of the patients with DM in spite of more intensive antihypertensive therapy. Additionally, the rates of CKD and obesity were significantly higher in patients with DM compared to non-DM patients. It suggests that hypertension is more advanced and difficult to control compared to normoglycemic patients [19, 20].
The rates of primary and secondary lipid goal attainment were significantly higher in patients with DM compared to non-DM subjects. Still, the LDL target was achieved only in one in two (DM+) or three (DM–) patients. There were no differences in statin use between the two groups. In spite of a very high CV risk of all patients, rosuvastatin was used only in one fifth of patients and atorvastatin was the most popular lipid-lowering drug. The prevalence of ezetimibe was very low in both subgroups and fibrates were used more frequently in DM. Finally, the rate of hypertriglyceridemia was higher in patients with DM. Only 1 in 3 patients used a specific lipid-lowering diet with a slightly better rate among diabetic patients. Those findings are consistent with previous reports on the mechanisms of dyslipidemia in DM [21]. Obesity and DM are associated mainly with harmful changes in the quality (not the quantity) of LDL particles and higher levels of triglycerides [22]. This may explain better rates of LDL-C and non-HDL-C goal attainment in patients with DM, while scheduled lipid-lowering therapy was similar between both subgroups. Another potential explanation could be better real compliance of individuals with DM to medical recommendations. In the EAV study, the rates of LDL goal achievement in all participants (29%) and patients with DM (39%) were even worse compared to our study groups [9]. Moreover, the results of the EA-IV [23] focused on patients with a previously known DM showed a similar attainment of BP target < 140/90 mm Hg (53%), HbA1c goal (53%) but significantly lower rate of LDL-C goal achievement (28%).
As expected, the rates of lifestyle goal attainment were alarming in both groups, especially in subjects with DM. An unhealthy lifestyle is a major risk factor for the development of DM [24]. Most patients reported making an attempt to maintain their weight target, but only one third of both subgroups reported aiming at weight loss. The number of patients reporting engagement in physical activity in order to lose weight was very small and similar in both subgroups. The rates of overweight and obesity in our study group with DM were higher compared to the overall rates in EAV (overweight 44%, obesity 38%) [9]. Although patients with an early stage of obesity without vascular or metabolic complications may have similar prognosis to non-obese individuals [25], obesity is the most important factor leading to DM.
Our study provided the most recent results on a real-life therapeutic effects in secondary prevention among Polish patients. The main strength of our multicenter study is that it was performed in cardiac centers of various reference levels using standardized interviews rather than retrospective medical records only. The survey was extensive and comparable with results of a large cross-sectional EAV study [9].
The final list of medical centers enrolling patients did not cover all the regions of Poland and therefore we cannot state that it was a nationwide epidemiologic study representative for Poland. All the participants were volunteers in a prospective visit and survey of their cardiovascular health. This is an obvious bias as the study group consisted of patients with an interest in CV prevention, suggesting that our results on therapeutic goal attainment in everyday practice might be even worse. Moreover, our invitation was limited only to patients hospitalized due to acute coronary syndrome or a revascularization procedure. Moreover, patients at higher risk who died within the first months after hospitalization might have presented even worse attainment of therapeutic goals. The retrospective data on study patients is based on medical records with all their imperfections, including the diagnosis of DM and the primary allocation to one of the subgroups. For the same reason we do not have patients’ HbA1c taken in the index hospitalization (not performed routinely), which would be used for a comparison with a prospective test. For logistic reasons, we did not perform OGTT at the prospective visit in all patients, which limits our knowledge on the current glucose state in the subgroup without DM.
In conclusion, this study provides the most recent and comprehensive results on secondary prevention among Polish coronary patients. A great majority of patients with DM in secondary prevention do not achieve treatment goals, particularly regarding lifestyles. Although lipid goal attainment is better in DM, the management of all risk factors needs to be improved. Routine screening for DM in coronary patients without known DM should become routine. Patients with DM need more intensive DM treatment as only 60% reached the diabetic goal. Smoking, obesity and low physical activity are the most important adverse lifestyles to be improved in both patients with and without DM.