Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
GENERAL SURGERY / RESEARCH PAPER
The use of prognostic scales in upper gastrointestinal tract bleeding.
1
2nd Department of General Surgery, Jagiellonian University Medical College, Poland
2
Jagiellonian University, Faculty of Medicine, Poland
Submission date: 2020-01-20
Final revision date: 2020-07-22
Acceptance date: 2020-08-27
Online publication date: 2021-04-29
Corresponding author
Czesław Osuch
2nd Department of General Surgery, Jagiellonian University Medical College, Jakubowksiego 2, 30-688, Kraków, Poland
2nd Department of General Surgery, Jagiellonian University Medical College, Jakubowksiego 2, 30-688, Kraków, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction:
In order to select high-risk patients, many prognostic scales have been invented. Among them, Rockall, Glasgow-Blatchford and AIMS 65 scales were considered the most useful.
Material and methods:
Patients with upper GI tract bleeding, treated between 2017 and 2018 were retrospectively enrolled to the study. Every patient had a Rockall, Glasgow-Blatchford and AIMS 65 score calculated retrospectively. Data on hospitalization as blood transfusions, length of hospital stay, rebleeding, intensive care unit (ICU) admission, mortality was included into data-base.
Results:
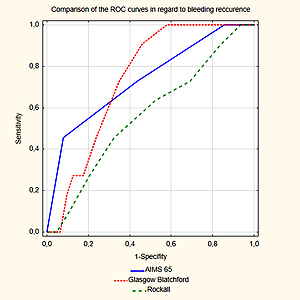
Univariate logistic regression revealed that only the AIMS65 scale was a prognostic factor for in-hospital mortality (OR 11.028; 95% CI: [2.271, 53.563], p=0.001). The AIMS 65 score >2 was the only factor predicting the need of >4 blood units transfusion during hospitalization (OR 3.977; 95% CI: [1.305, 12.122], p=0.015), whereas Glasgow-Blatchford scale >5 was the only risk factor for the need of fresh frozen plasma transfusion (OR 3.657; 95% CI: [1.010-13.242], p=0.048). The area under a curve (AUC) in the ROC analysis revealed that the AIMS 65 scale was the most accurate in mortality prediction (AUC=0.859, p=0.002), whereas Rockall score and Glasgow-Blatchford were not significant (AUC=0.614, p=0.093 and AUC=0.504, p=0.97, respectively).
Conclusions:
Based on our results, we recommend using AIMS 65 scoring system. It’s simple and requires few of parameters to be counted. Also, it proved to be the most efficient in predicting in-hospital mortality.
In order to select high-risk patients, many prognostic scales have been invented. Among them, Rockall, Glasgow-Blatchford and AIMS 65 scales were considered the most useful.
Material and methods:
Patients with upper GI tract bleeding, treated between 2017 and 2018 were retrospectively enrolled to the study. Every patient had a Rockall, Glasgow-Blatchford and AIMS 65 score calculated retrospectively. Data on hospitalization as blood transfusions, length of hospital stay, rebleeding, intensive care unit (ICU) admission, mortality was included into data-base.
Results:
Univariate logistic regression revealed that only the AIMS65 scale was a prognostic factor for in-hospital mortality (OR 11.028; 95% CI: [2.271, 53.563], p=0.001). The AIMS 65 score >2 was the only factor predicting the need of >4 blood units transfusion during hospitalization (OR 3.977; 95% CI: [1.305, 12.122], p=0.015), whereas Glasgow-Blatchford scale >5 was the only risk factor for the need of fresh frozen plasma transfusion (OR 3.657; 95% CI: [1.010-13.242], p=0.048). The area under a curve (AUC) in the ROC analysis revealed that the AIMS 65 scale was the most accurate in mortality prediction (AUC=0.859, p=0.002), whereas Rockall score and Glasgow-Blatchford were not significant (AUC=0.614, p=0.093 and AUC=0.504, p=0.97, respectively).
Conclusions:
Based on our results, we recommend using AIMS 65 scoring system. It’s simple and requires few of parameters to be counted. Also, it proved to be the most efficient in predicting in-hospital mortality.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.