Pyroptosis is a programmed form of inflammatory cell death mediated by inflammasomes, characterized by the rupture of the cell membrane and the release of intracellular contents, which elicits a robust inflammatory response. This process frequently involves the activation of specific Gasdermin proteins (such as GSDMA, GSDMB, GSDMC, GSDMD, GSDME, PJVK), which possess distinct N-terminal and C-terminal domains [1]. Gasdermins trigger pyroptosis by forming pores upon activation, resulting in the release of cellular contents, amplification of local inflammatory responses, and modulation of immune responses within the microenvironment [2]. The characteristics of the tumor immune microenvironment significantly influence tumor growth and metastasis, and are closely associated with patient prognosis. Gasdermins may function as potential regulatory factors within this microenvironment, providing novel targets and strategies for cancer immunotherapy [3, 4]. Prostate cancer is the most common malignant tumor in men globally. The emergence of immune checkpoint inhibitors has revolutionized cancer immunotherapy, reshaping the treatment landscape. Prostate cancer is often classified as a “cold” tumor, which typically shows limited response to immunotherapy. However, pyroptosis can transform “cold” tumors into “hot” tumors by modulating the immune microenvironment, thereby enhancing their responsiveness to immunotherapy [5, 6].
Methods
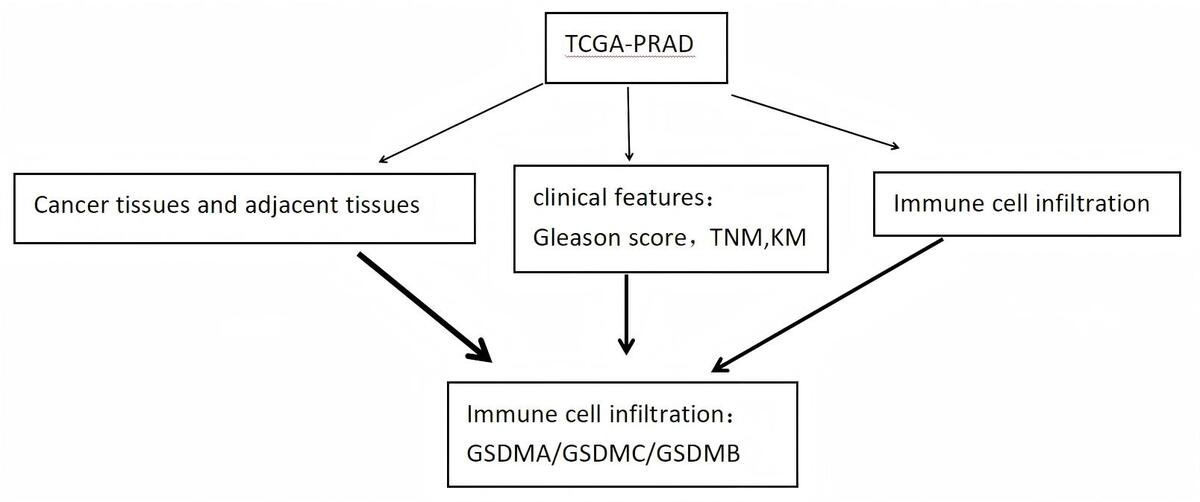
In this study, we conducted a comprehensive analysis to investigate the differential expression of Gasdermins in prostate cancer tissues compared to adjacent non-cancerous tissues using data from the TCGA-PRAD database.
Results
Our results revealed that, except for GSDMC, which showed no significant differential expression between cancerous and non-cancerous tissues, the other five Gasdermins exhibited marked differences in expression levels. To further elucidate these findings, we examined the correlations between the differential expression of Gasdermins and various clinical features, including tumor grade, stage, and patient survival time. Detailed results are provided in Supplementary Table SI. Notably, the expression levels of GSDMA and GSDMC varied significantly across different Gleason scores, while GSDMB expression demonstrated significant variability across clinical stages, underscoring the potential implications of these findings for understanding the role of Gasdermins in prostate cancer progression.
We assessed the association between Gasdermin expression and immune cell infiltration in the tumor microenvironment using CIBERSORT, TIMER, and other advanced computational algorithms. Our results demonstrated a positive correlation between Gasdermin expression and both immune cell infiltration (Figure 1 A) and immune score (Figure 1 B). Patients were stratified into high-expression and low-expression groups based on Gasdermin levels, and survival analysis was performed to evaluate the impact on patient prognosis (Figure 1 C). The findings indicated that prostate cancer patients in the disease-free progression phase exhibited significant differences in GSDMB and PJVK expression levels, while no significant differences were observed for other Gasdermins. These preliminary studies elucidate the multifaceted roles of Gasdermins in prostate cancer and provide a comprehensive evaluation of the relationship between Gasdermin expression and immune cell infiltration (Figure 1 D). This enhances our understanding of the immune landscape associated with varying Gasdermin levels and establishes a Cox regression prognostic model for differential proteins, suggesting the potential of Gasdermins as prognostic biomarkers in prostate cancer.
Figure 1
A – The relationship between GSDMs and immune cell infiltration; B – Correlation between GSDMs and matrix immune score; C – GSDMs relationship with survival curve, correlation between risk factors of D.C.OX prognostic model and GSDMs, D – Risk factor scores were correlated with major immune cells

Discussion
Through the aforementioned analysis, it is evident that GSDMA, GSDMC, and GSDMB play crucial roles in the biology of prostate cancer and patient prognosis. Notably, GSDMA’s involvement in pyroptosis has been extensively documented across various cancers, with its expression levels correlating with tumor invasiveness and patient survival outcomes [7, 8]. Our findings demonstrate that elevated GSDMA expression is significantly associated with advanced tumor stages and poorer prognosis, indicating that GSDMA may serve as a promising biomarker for disease progression and a potential target for therapeutic intervention. Recent studies have revealed that GSDMC can modulate the tumor microenvironment by influencing immune cell infiltration [9]. In our analysis, we observed a significant correlation between GSDMC expression levels and the presence of specific immune cell types in the tumor microenvironment, suggesting that GSDMC may play a role in immune evasion mechanisms observed in prostate cancer. This finding underscores the potential of GSDMC not only as a prognostic marker but also as a mediator of immune interactions within the tumor microenvironment. Furthermore, emerging evidence indicates that GSDMB is involved in regulating apoptosis and necrosis, contributing to cancer cell survival and proliferation [10, 11]. Our survival analysis revealed that patients with high GSDMB expression experienced a significant survival disadvantage, independent of other clinical factors. This underscores the critical role of GSDMB in prostate cancer prognosis and indicates its potential as a valuable therapeutic target for enhancing treatment efficacy. In summary, the differential expression of Gasdermins, particularly GSDMA, GSDMC, and GSDMB, in prostate cancer highlights their potential as biomarkers and therapeutic targets. Further investigation into their mechanisms and interactions within the tumor microenvironment is essential to fully understand their contributions to prostate cancer progression and patient outcomes.
This study acknowledges several important limitations that should be considered in the context of our findings. Firstly, the reliance on data from the TCGA database may introduce inherent biases, such as variations in sample collection protocols and processing methods, which could compromise the generalizability of our results to broader populations. Secondly, while we utilized sophisticated algorithms like CIBERSORT and TIMER to assess immune cell infiltration within the tumor microenvironment, it is essential to recognize that these computational methods have limitations in terms of accuracy and may not fully capture the complex nuances of the tumor microenvironment. Thirdly, the retrospective nature of our analysis restricts our ability to establish definitive causal relationships between Gasdermin expression levels and clinical outcomes, a critical consideration for interpreting the implications of our research. Finally, although we performed a comprehensive Cox regression analysis to evaluate the independent prognostic value of Gasdermins, potential confounding effects from unmeasured clinical variables cannot be entirely excluded, which may affect the overall robustness and reliability of our conclusions.
In conclusion, our analysis of Gasdermin expression in prostate cancer and adjacent tissues using data from the TCGA database reveals significant differential expression patterns that correlate with various clinical characteristics, including tumor grade, stage, and patient survival. The application of computational algorithms such as CIBERSORT and TIMER has further clarified the relationship between Gasdermin expression and immune cell infiltration within the tumor microenvironment. By stratifying patients into high- and low-expression groups based on Gasdermin levels, we performed survival analyses that highlight the prognostic significance of GSDMA, GSDMC, GSDMB, and PJVK. Subsequent multivariate Cox regression analysis, adjusting for other clinical variables, reinforces the potential of these Gasdermins as biomarkers for predicting patient prognosis in prostate cancer. These findings not only deepen our understanding of the role of Gasdermins in tumor biology but also suggest promising directions for future research focused on therapeutic targeting and personalized treatment strategies.