Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
GASTROENTEROLOGY / RESEARCH PAPER
The outcomes of multivisceral resection for primary T4b colorectal cancer in a tertiary referral centre: a propensity score matching analysis
1
Medical University of Lodz, Poland
2
Department of Surgery, Middlemore Hospital, University of Auckland, New Zealand
Submission date: 2020-11-22
Final revision date: 2020-12-09
Acceptance date: 2020-12-26
Online publication date: 2021-03-25
KEYWORDS
TOPICS
ABSTRACT
Introduction:
A multivisceral resection (MVR) is often necessary for patients with colorectal cancer (CRC) because the tumour must be removed en bloc with the infiltrated tissues. The outcomes of MVR are variably presented in the literature. This study aimed to analyse mortality and morbidity of MVR in patients with CRC.
Material and methods:
This retrospective study was performed using the Department of General and Colorectal Surgery database of 2204 patients operated on for CRC. Patients with MVR due to stage pT4b primary CRC were the study group. Patients with no sign of intraoperative infiltration into contiguous structures who had undergone a traditional resection qualified for the control group. Mortality and morbidity for both groups were compared using a propensity score matching analysis.
Results:
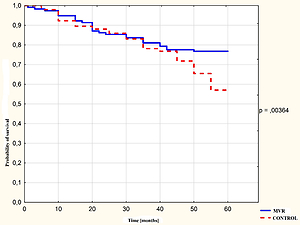
Patients with no sign of intraoperative infiltration into contiguous structures, who had undergone a traditional resection, qualified for the control group, while 117 patients with MVR due to stage pT4b primary CRC were included in the study group. Early post-operative mortality was not significantly increased in the MVR group (3.4% vs. 1.4%; p = 0.284). The mean operative time was significantly longer in the MVR group (p < 0.001). The 5-year absolute survival rate was significantly higher in the MVR group (76.7%) than in the control group (57.0%; p = 0.004).
Conclusions:
MVR in pT4 CRC is not linked to a higher risk of significant post-operative complications compared to standard resections. Patients with CRC with involvement of contiguous structures, who undergo an MVR, do not appear to have worse long-time outcome than those who do not have involvement of contiguous structures.
A multivisceral resection (MVR) is often necessary for patients with colorectal cancer (CRC) because the tumour must be removed en bloc with the infiltrated tissues. The outcomes of MVR are variably presented in the literature. This study aimed to analyse mortality and morbidity of MVR in patients with CRC.
Material and methods:
This retrospective study was performed using the Department of General and Colorectal Surgery database of 2204 patients operated on for CRC. Patients with MVR due to stage pT4b primary CRC were the study group. Patients with no sign of intraoperative infiltration into contiguous structures who had undergone a traditional resection qualified for the control group. Mortality and morbidity for both groups were compared using a propensity score matching analysis.
Results:
Patients with no sign of intraoperative infiltration into contiguous structures, who had undergone a traditional resection, qualified for the control group, while 117 patients with MVR due to stage pT4b primary CRC were included in the study group. Early post-operative mortality was not significantly increased in the MVR group (3.4% vs. 1.4%; p = 0.284). The mean operative time was significantly longer in the MVR group (p < 0.001). The 5-year absolute survival rate was significantly higher in the MVR group (76.7%) than in the control group (57.0%; p = 0.004).
Conclusions:
MVR in pT4 CRC is not linked to a higher risk of significant post-operative complications compared to standard resections. Patients with CRC with involvement of contiguous structures, who undergo an MVR, do not appear to have worse long-time outcome than those who do not have involvement of contiguous structures.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.