Chronic obstructive pulmonary disease (COPD), including its main subtypes of emphysema and chronic bronchitis, significantly impacts patients’ quality of life and incurs substantial medical costs. In the United States nearly 25 million people are affected by asthma [1]. Recent studies, including a meta-analysis of 30 cohort studies, have indicated that lung diseases such as asthma and COPD markedly increase cardiovascular disease risk. Numerous epidemiological studies have explored the connection between lung disease (including asthma and COPD) and cardiovascular disease [2]. Recently, a meta-analysis of 30 cohort studies revealed that asthma significantly increases the risk of cardiovascular disease [3]. The American Heart Association’s “Life’s Simple 7” (LS7) metrics and its updated LE8 score, which includes sleep health, have been foundational in understanding these relationships. Although research using the LS7 score has revealed that ideal cardiovascular health (CVH) indicators significantly reduce the incidence of COPD [4], studies using the LE8 system are rare [5].
Furthermore, in discussing the complex relationship between lung diseases and cardiovascular health, a key factor that cannot be overlooked is depression. Depression, a prevalent mental health issue, affects hundreds of millions of people worldwide and has been proven to have significant connections with various physical health conditions, including lung diseases and cardiovascular diseases [6].
Given these considerations, we hypothesised that there may be an interconnection between lung disease, depression, and CVH. Although previous research has explored the relationships between lung disease and CVH and between depression and CVH, few studies have been conducted to simultaneously consider the interactions among these 3 variables, particularly the mediating role of depression between lung disease and CVH. Therefore, the aim of our study was to examine the mediating role of depression in this relationship by utilising National Health and Nutrition Examination Survey (NHANES) data and the LE8 score to offer insights into more integrated treatment approaches.
Methods
Using data from the National Health and Nutrition Examination Survey (NHANES) for 3 cycles between 2013 and 2018, our study analysed 2508 participants older than 20 years who had complete data on lung diseases, depression, and CVH scores. Lung diseases, including asthma, emphysema, chronic bronchitis, and COPD, were assessed using the NHANES Medical Conditions Questionnaire. Depression was evaluated via the Patient Health Questionnaire-9 (PHQ-9), with a score of 10 or more indicating depression. CVH scores, integrating body mass index, blood pressure, cholesterol, blood glucose, diet, physical activity, nicotine exposure, and sleep duration, were calculated according to the American Heart Association’s criteria. Covariates included age, sex, race/ethnicity, socioeconomic status, marital status, and alcohol consumption were based on interviews and biomarker assessments.
Statistical analysis
Continuous variables are described as the means ± SDs or medians with interquartile ranges based on their distribution, while categorical variables are expressed as frequencies and percentages. Differences were assessed using Student’s t-test or the Mann-Whitney U test for continuous data, and the χ2 test or Fisher’s exact test for categorical data. Initially, linear regression analysis was used to evaluate the overall association between lung disease and CVH scores without considering the impact of depression. Subsequently, linear regression and logistic regression analyses were used to assess the associations between lung disease and depression scores and between lung disease and depression severity. Two models were constructed for the analysis: Model 1 was an unadjusted crude model, and Model 2 was built upon Model 1 and further adjusted for confounding factors, including age, sex, race, family PIR, educational level, marital status, drinking status, waist circumference, alanine transaminase (ALT), aspartate transaminase (AST), uric acid, arthritis history, and liver disease history. Importantly, we employed bootstrap mediation analysis due to its robustness in handling nonnormal data, which is often encountered in studies with moderate sample sizes. This method effectively uses resampling techniques (5000 bootstrap samples) to estimate the distribution of indirect effects and to calculate precise confidence intervals without assuming a normal distribution. Our choice is further supported by rigorous model evaluations using R2 and the Akaike information criterion (AIC) and thorough assumptions checks, including the variance inflation factor (VIF), for multicollinearity and residual analysis for homoscedasticity and normality, ensuring that our models accurately represent the data and maintain statistical integrity.
All the statistical analyses were conducted using R Statistical Software (version 4.3.1; The R Foundation, http://www.R-project.org) and the Free Statistical analysis platform (version 1.9; Beijing, China). We employed a two-tailed test, and a result was considered statistically significant when the p-value was less than 0.05.
Results
According to the multivariate linear regression analysis shown in Table I, after accounting for potential confounding factors, we observed that participants with lung disease exhibited significantly lower CVH scores than did those without lung disease (β = –1.62, 95% CI: –2.68 to –-0.56). Notably, individuals with chronic bronchitis and COPD had even lower CVH scores (chronic bronchitis: β = –3.61, 95% CI: –5.33 to –1.88; COPD: β = –3.3, 95% CI = –5.45 to –1.15). These results reveal the severity of the impact of lung diseases on CVH.
Table I
Association between lung disease and CVH scores
Table II shows that individuals with lung diseases also had an increased risk of developing depression, with an adjusted odds ratio of 1.58 (95% CI: 1.14 to 2.2). The effect was particularly notable among individuals with asthma and chronic bronchitis (asthma: β = 1.49, 95% CI: 1.03 to 2.14; chronic bronchitis: β = 2.51, 95% CI: 1.62 to 3.9, all p < 0.05). These findings highlight the association between lung disease and depression.
Table II
Association between lung disease and depression status
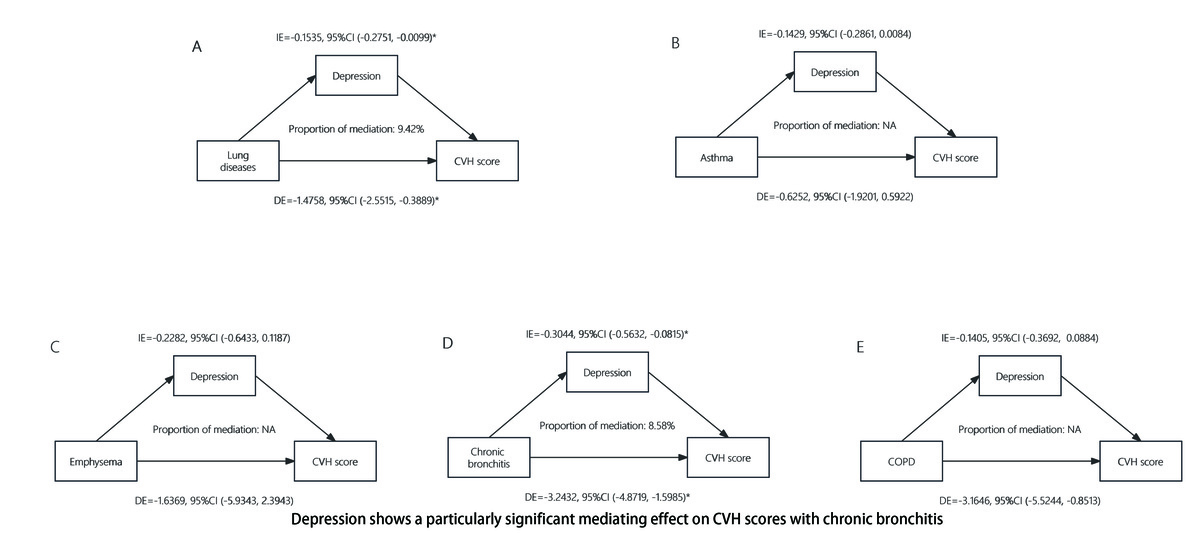
In our study, we used advanced statistical models to assess how lung diseases impact CVH scores. After adjusting for confounders, we identified a significant negative impact of lung disease on CVH scores (total effect: β = –1.6294, 95% CI = –2.6887 to –0.5081). This negative association persisted even after accounting for depression risk (direct effect: β = –1.4758, 95% CI: –2.5515 to –0.3889). Bootstrap methods confirmed depression’s significant mediating effect (β1 * β2 = –0.1535, 95% CI: –0.2751 to –0.0099), indicating that depression mediates 9.42% of the total effect between lung disease and CVH scores. Further analysis of the mediating role of depression among patients with asthma, emphysema, chronic bronchitis, and COPD revealed a particularly significant mediating effect among those with chronic bronchitis (Figure 1). Figure 1 provides a detailed illustration of how depression mediates the relationship between various types of lung disease and CVH scores among patients.
Figure 1
Depression as a mediator of the relationship between lung diseases and CVH scores. Mediation analysis by the bootstrap test: adjusted for age, sex, race, family PIR, educational level, marital status, drinking status, waist circumference, ALT, AST, uric acid, arthritis history, and liver disease history. Depression shows a particularly significant mediating effect on CVH scores with chronic bronchitis
IE – indirect effect, DE – direct effect, CVH – cardiovascular health, COPD – chronic obstructive pulmonary disease. *P < 0.05.
Discussion
To our knowledge, this study represents the first comprehensive examination utilising NHANES data to explore the interconnections among lung diseases, depression, and CVH. Our analysis revealed a significant association between lung disease and both depression and CVH scores. Importantly, we observed that depression mediated the relationship between lung disease and CVH scores, accounting for 9.42% of the effect. While this may appear to be a modest effect, it is significant in the context of chronic diseases where multiple factors contribute to outcomes.
A study involving 41,810 adults aged 18 and older from 6 low- and middle-income countries indicated that depression increases the incidence of asthma and chronic lung diseases [7]. Our study corroborates this finding by revealing a positive correlation between lung disease and depression and reinforcing the high prevalence of depressive symptoms among patients with lung conditions. The primary mechanisms driving depression in these patients may be related to common risk factors such as the need for long-term oxygen therapy, restricted activity, and increased feelings of social isolation. Additionally, the chronic pain and reduced mobility due to respiratory difficulties often faced by these patients could contribute to an increased risk of developing depression. These factors may collectively exacerbate the psychological burden on patients with lung diseases, thereby increasing their risk of developing depression [8].
In our study, lung disease also emerged as an independent risk factor for lower CVH scores. This finding aligns with recent research. For instance, a prospective cohort study involving 201 Spanish patients with chronic obstructive pulmonary disease (COPD) revealed a close association between chronic bronchial infections and cardiovascular events in COPD patients [9]. Szucs et al. highlighted the exacerbation of outcomes when COPD and CVD coexist due to factors such as oxygen deprivation, inflammation, and arterial rigidity [10]. Notably, our findings also show that depression mediates the relationship between lung disease and CVH. This mediation may involve mechanisms such as chronic inflammation and oxidative stress, which are characteristic of chronic obstructive pulmonary diseases. These factors contribute to systemic effects impacting brain function and mood, thereby increasing susceptibility to depression. Chronic hypoxia from lung disease can cause neuroinflammation and changes in the central nervous system, predisposing individuals to depression [11]. Additionally, depression may influence CVD through behavioural and biological pathways, including unhealthy lifestyles [12], sympathetic nervous system hyperactivity, and hypothalamic-pituitary-adrenal axis dysfunction [13], potentially leading to endothelial dysfunction, platelet activation [14], and increased inflammatory markers [15], which are all risk factors for CVD. In conclusion, depression plays a significant mediating role in the association between lung disease and cardiovascular health through these complex biological and behavioural mechanisms.
This study has certain limitations. First, many of the NHANES data rely on self-reports from participants, which could lead to inaccuracies due to recall bias, misunderstanding, or other reasons. Second, it is worth noting that the data on lung diseases in the NHANES only cover asthma, emphysema, chronic bronchitis, and COPD and do not include other types of lung conditions. This could limit our understanding of the association between depression and a broader range of lung diseases. Additionally, these results are based on the NHANES dataset from 2013–2018, which, while nationally representative of the United States, may not fully extend to other populations or healthcare systems due to differences in demographics, healthcare access, and treatment protocols. This specificity might limit the generalisability of our results to populations outside the United States or in different healthcare contexts. Despite these limitations, our study has significant strengths and contributes to the existing body of knowledge. This study is among the first to quantify the mediating role of depression in the relationship between lung diseases and CVH scores, providing valuable insights into the complex mechanisms that underlie these associations.
In conclusion, our findings revealed that depression mediated 9.42% of the association between lung disease and lower CVH scores, indicating a significant role of mental health in CVH among these patients. This underscores the need for integrated care strategies that include mental health support as part of the overall management plan for lung disease patients, potentially improving cardiovascular outcomes. The implementation of routine depression screenings and behavioural health interventions, such as cognitive-behavioural therapy, could help with the management of depression symptoms and enhance patient care.