Introduction
Primary care (PC) provides treatment for many patients living with the coexistence of two or more chronic health problems, i.e. multimorbi-dity [1, 2]. This is also true for patients with mental conditions and psychological problems [3].
The number of patients with multimorbidity is rising rapidly [4] and so is the burden it carries [5, 6]; this is even more pronounced in older people [4, 7], as life expectancy continues to increase. According to the United Nations, the growth rate of the global population aged 60 or above is estimated at 3% per year; the greatest percentage of older persons aged 60 or above dwell in Europe (25%) [8].
Prevalence of multimorbidity in old age can reach up to 98% [6]. In Portugal, 82.7% of primary care patients aged 65 or above reported having 2+ of 147 chronic health problems [1].
The presence of mental health problems in an individual increases with the number of simultaneous physical problems [9], people with multimorbidity being two to three times more likely to experience mental health problems, especially older people [10]. Depression and other mental health problems are more prevalent in patients with cardiovascular diseases, diabetes, chronic obstructive pulmonary disease, and chronic musculoskeletal disorders [11].
QoL is an extensive and subjective construct [12] that “broadly encompasses how an individual measures the ‘goodness’ of multiple aspects of their life” [13]. The importance of studying health-related QoL in distinct health problems is widely recognized in previously published articles in this journal [14–17]. In old age this concept is even more important since it is commonly accepted that a shorter life with quality is better than a longer one without it [12].
Mental-physical multimorbidity (MPM) is highly prevalent and increases total health care costs, but still needs a better understanding [18, 19], as does health-related quality of life (QoL) in older people [20]. Previous research shows that most QoL studies do not include mental health problems or that they were excluded from measures of QoL [21]. Given the number of patients with mental conditions who receive their care within a PC context, and the high prevalence of multimorbidity in PC (especially in older people), it is necessary to study MPM in this population and context.
The present study aims to identify the impact on health-related QoL of MPM in adults aged 60 years and older within primary care.
Material and methods
Data used for this secondary analysis were collected from phase II of the MM-PT project (Multi-morbidity in primary care in Portugal), a multicentre cross-sectional study conducted in the Centre Region of Portugal, which has been previously described elsewhere [22, 23]. In a few words, general practitioners (GPs) from 13 primary care centres were enrolled to collect information regarding demographic, clinical, and health-related QoL from 521 adult patients presenting for primary care consultations; written informed consent was always given. All patients were multimorbid, with at least 2 chronic health problems out of a list of 147 conditions [24], of which at least one was required to be hypertension, diabetes, asthma or osteoarthritis [23]. The institutional ethics committee approved the original study and it was performed in accordance with the ethical standards of the Declaration of Helsinki. Written consent was obtained from study participants.
The dataset was previously stripped of all identifying information and consequently did not generate identifiable data. The current analysis was performed in 251 individuals, 60 years and older. All adults aged under 60 years were excluded as the current analysis focused on older people with multimorbidity alone. No missing data were found for the included patients.
For the current study, the number of chronic health problems was obtained and categorized as 2–5 conditions and 6+ conditions. Health-related QoL was estimated for the entire sample using the Portuguese Short Form-12 Health Status Questionnaire (SF-12) [25]. The SF-12 is a generic measure of health status. SF-12 measures eight health aspects, namely physical functioning (PF), role limitations due to physical health problems (RP), bodily pain (BP), general health perceptions (GH), vitality (VT), social functioning (SF), role limitations due to emotional problems (RE), and mental health (psychological distress and psychological well-being) (MH). Two summary measures are derived from the SF-12: physical health (Physical Component Summary – PCS) and mental health (Mental Component Summary – MCS). Higher scores represent better health [25, 26].
The studied sample was divided into 2 groups of patients: (i) patients with 2+ chronic physical health problems but no mental health problems (physical-only multimorbidity, POM), and (ii) patients with 2+ chronic health problems including at least 1 physical and 1 mental (mental-physical multimorbidity – MPM).
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics for Windows, Version 21.0. Summary statistics were calculated according to variable type and distribution. Comparisons between categorical data were analysed using the χ2 test. Numerical variables were analysed using the Mann-Whitney U-test when the dependent variable was not normally distributed. Multiple linear regressions were performed for the two summary measures (PCS and MCS) using variables significant in the univariate analysis and a stepwise selection method (for MPM patients and POM patients). All tests considered a significance threshold of p < 0.05.
Results
Patient characteristics are presented in Table I. Mental-physical multimorbidity patients were mostly women (81%) and on average were younger than those with POM; 81% were less than 75 years old. The mean number of chronic health problems in MPM patients was higher than in those with POM (5.9 vs. 5.2; p = 0.006); the majority of MPM had 6+ conditions (60.3%; p = 0.003).
Table I
Characteristics of the 251 Portuguese primary care patients with multimorbidity aged 60 years and older (2014–2015)
| Parameter | Total (N = 251) | Multimorbidity | ||
|---|---|---|---|---|
| Physical-only (n = 193) | Mental-physical (n = 58) | P-value* | ||
| Sex, female, % (n)a | 57.8 (145) | 50.8 (98) | 81.0 (47) | < 0.001 |
| Age [years]: | ||||
| Meanb (SD; min.–max.) | 70.6 (7.7; 60–93) | 71.4 (7.8; 60–93) | 67.8 (6.8; 60–83) | 0.001 |
| 60–74 years, % (n)a | 69.7 (175) | 66.3 (128) | 81.0 (47) | 0.032 |
| 75+ years, % (n) | 30.3 (76) | 33.7 (65) | 11.0 (19) | |
| Living arrangements, % (n)a: | ||||
| Alone | 16.3 (41) | 12.4 (24) | 29.3 (17) | 0.002 |
| With someone | 83.7 (210) | 87.6 (169) | 70.7 (41) | |
| Education level, % (n)a: | ||||
| Low education (6 or less years) | 87.6 (220) | 88.6 (171) | 84.5 (49) | 0.403 |
| High education (more than 6 years) | 12.4 (31) | 11.4 (22) | 15.5 (9) | |
| Income level, % (n)a: | ||||
| Low income | 36.3 (91) | 35.2 (68) | 39.7 (23) | 0.539 |
| High income | 63.7 (160) | 64.8 (125) | 60.3 (35) | |
| Chronic health problems: | 0.006 | |||
| Meanb (SD; min.–max.) | 5.4 (2.3; 2–13) | 5.2 (2.4; 2–13) | 5.9 (1.8; 2–10) | |
| 2–5 conditionsa | 56.6 (142) | 61.7 (119) | 39.7 (23) | 0.003 |
| 6+ conditions | 43.3 (109) | 38.3 (74) | 60.3 (35) | |
Table II shows that MPM patients and those with POM had low mean SF-12 scores. These scores were even lower in MPM patients than those with POM. The scores that load heavily on mental health (SF and MH) were statistically significantly lower in the MPM group than in the POM group. The Mental Component Summary score was also significantly lower in the MPM group. However, regarding PCS no significant difference between the two groups of patients was evident.
Table II
SF-12 scores of individual scales by physical multimorbidity and mental-physical multimorbidity (2014–2015)
| Scores | Total (N = 251) | Multimorbidity | P-value* | |
|---|---|---|---|---|
| Physical-only (n = 193) | Mental-physical (n = 58) | |||
| SF-12 scale scores, mean (SD)a: | ||||
| Physical: | ||||
| Physical Functioning | 41.2 (12.5) | 42.0 (12.5) | 38.7 (12.2) | 0.076 |
| Role-Physical | 40.0 (13.5) | 40.3 (13.9) | 39.0 (12.2) | 0.500 |
| Bodily Pain | 38.3 (12.0) | 39.0 (11.8) | 36.0 (12.5) | 0.116 |
| General Health | 31.8 (9.6) | 32.2 (9.6) | 30.5 (9.8) | 0.203 |
| Mental: | ||||
| Vitality | 46.7 (11.3) | 47.4 (10.9) | 44.6 (12.2) | 0.117 |
| Social Functioning | 43.8 (14.2) | 44.9 (13.8) | 40.0 (14.7) | 0.018 |
| Role-Emotional | 43.0 (13.1) | 43.9 (12.5) | 39.8 (14.5) | 0.055 |
| Mental Health | 45.3 (13.1) | 47.2 (12.6) | 38.9 (12.8) | < 0.001 |
| SF-12 component scores, mean (SD)a: | ||||
| Summary: | ||||
| Physical Component Summary (PCS) | 36.8 (11.3) | 37.0 (11.5) | 36.4 (10.5) | 0.666 |
| Mental Component Summary (MCS) | 46.9 (12.2) | 48.4 (11.5) | 41.9 (13.4) | 0.001 |
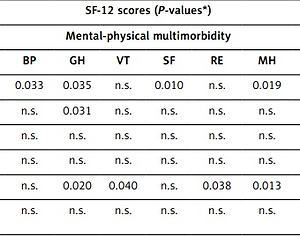
Table III shows that in MPM patients SF-12 scores were related to patients’ characteristics. Scores that load heavily on physical health were statistically related to sex, age, living arrangements and income. Scores that load heavily on mental health were statistically related to sex and living arrangements. SF-12 scores of MPM patients were not related to the number of chronic health problems. Contrarily, the number of chronic conditions was related to SF-12 scores in POM patients, particularly the PCS.
Table III
Association between SF-12 scores and patients’ characteristics (2014–2015)
| Characteristic | SF-12 scores (P-values*) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mental-physical multimorbidity | ||||||||||
| PF | RP | BP | GH | VT | SF | RE | MH | PCS | MCS | |
| Sex | 0.001 | n.s. | 0.033 | 0.035 | n.s. | 0.010 | n.s. | 0.019 | 0.012 | 0.031 |
| Age group | 0.016 | n.s. | n.s. | 0.031 | n.s. | n.s. | n.s. | n.s. | 0.006 | n.s. . |
| Living arrangements | 0.003 | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | 0.026 | n.s. |
| Education level | n.s | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. |
| Income level | 0.019 | 0.003 | n.s. | 0.020 | 0.040 | n.s. | 0.038 | 0.013 | 0.043 | 0.048 |
| Chronic health problems group | n.s | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. |
| Physical-only multimorbidity | ||||||||||
| PF | RP | BP | GH | VT | SF | RE | MH | PCS | MCS | |
| Sex | < 0.001 | n.s. | 0.001 | n.s. | n.s. | 0.024 | n.s. | < 0.001 | 0.012 | 0.014 |
| Age group | < 0.001 | 0.002 | n.s. | n.s. | 0.030 | 0.001 | n.s. | n.s. | 0.001 | n.s. |
| Living arrangements | 0.050 | 0.008 | n.s. | n.s. | n.s. | 0.002 | 0.038 | 0.026 | n.s. | 0.031 |
| Education level | n.s | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. |
| Income level | 0.031 | 0.032 | 0.002 | 0.005 | 0.028 | 0.003 | < 0.001 | 0.007 | 0.033 | < 0.001 |
| Chronic health problems group | 0.005 | < 0.001 | < 0.001 | n.s. | 0.041 | 0.029 | 0.020 | n.s. | <0.001 | n.s. |
Table IV shows that in MPM patients, female sex, 75+ years, and low income were associated with statistically significantly lower PCS score. Female sex was also associated with statistically significantly lower MCS score. Regarding POM patients, female sex, 75+ years, and 6+ chronic conditions were associated with statistically significantly lower PCS score. Female sex, living alone, and low income were associated with statistically significantly lower MCS score.
Table IV
Multiple linear regression for Physical Component Summary (PCS) and Mental Component Summary (MCS)
| Variable | Mental-physical multimorbidity | Physical-only multimorbidity | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PCS | MCS | PCS | MCS | |||||||||
| B | SEB | β | B | SEB | β | B | SEB | β | B | SEB | β | |
| Intercept | 30.94 | 6.41 | – | 30.54 | 5.43 | – | 45.41 | 3.77 | – | 23.56 | 5.33 | – |
| Sex | 6.43 | 3.18 | 0.24* | 9.51 | 4.33 | 0.28* | 3.98 | 1.54 | 0.17* | 3.34 | 1.57 | 0.15* |
| Age group | – 8.96 | 3.11 | –0.34* | – | – | – | –5.22 | 1.65 | –0.22* | – | – | – |
| Living arrangements | – | – | – | – | – | – | – | – | – | 5.17 | 2.38 | 0.15* |
| Income level | 5.26 | 2.53 | 0.25* | – | – | – | – | – | – | 6.18 | 1.64 | 0.26* |
| Chronic health problems group | – | – | – | – | – | – | –5.35 | 1.61 | –0.23* | – | – | – |
Discussion
The present study will be useful for better understanding of the complex impact of MPM on health-related QoL of older people in primary care. To the best of the authors’ knowledge, this is the first study of such nature in Portugal.
Even though the sample of patients with MPM in the present study was relatively small (n = 58), it made up a substantial proportion of all older people with 2+ chronic health problems (23.1%). This proportion is roughly in line with published prevalence rates amongst primary care patients [5]. Its epidemiologic characteristics (more common in women than men and in younger age groups) were like those encountered in other studies [5, 9], supporting the validity of the current study findings. This study also supports evidence from previous observations [27] where patients with mental conditions have more diseases, in a known bidirectional relationship [19, 28]. Nonetheless, because of the sample size, the results may not be generalisable. Further research is suggested on larger nationwide samples.
In general, MPM substantially and negatively affected health-related QoL of older people in primary care and was considerably worse compared with POM patients. These results match those observed in previous studies [29–31]. In reality, these findings of low health-related QoL can be even worse when we keep in mind that older people with health conditions often report QoL positively [12]. In a Canadian successful aging study, more than 80% of the 1821 participants of older age responded positively to the question “Do you think you have aged successfully?” [32]. Expectedly, in the current study, mental health (MCS score) was also significantly worse in the MPM group compared with the POM group. It can thus be suggested that older people with MPM suffer to a greater extent from maladaptive reaction to multimorbidity; the presence of some of the psychological problems may be a manifestation of the adjustment disorder [33], with a greater inability to feel calm and peaceful compared with POM patients. Older people with MPM also reported greater interference in their social activities (visiting friends, relatives, etc). Considering that a strong social network is associated with better QoL [34] and protects from multimorbidity [6], older people with MPM will probably need help for social support from the community, as seen in the present study; living with someone is a protective factor regarding mental health only for older people with POM.
The number of chronic conditions was related to SF-12 scores in POM patients, but not in MPM patients. More than the number of chronic health problems, the most probable explanation for this might be that the disease severity would be responsible for the decline in QoL, through the increase of psychological distress in older people with MPM [35]. Another explanation might be related to the presence of mental conditions which are known to have a larger effect on QoL than the severity of the physical illness [19]. Nonetheless, future research regarding MPM multimorbidity should consider the use of disease severity measures.
Some sociodemographic characteristics, commonly associated with worse health-related QoL in the context of multimorbidity [6, 23, 36], were also found in geriatric MPM patients: female sex, old age and low income (after the model was adjusted). These data suggest that MPM patients will most likely need care through medical and social services, as well as financial support [6, 23].
Limitations to the present study include the risks of secondary data analysis. Nonetheless, the authors were the ones who collected the original data, and as such, know perfectly the constructs measured and by what means they were measured, which was certainly an advantage [37]. Another advantage was that in the original sample, the 4 diseases collected are not only known to be associated with lower QoL but also with mental conditions.
In the future it would be beneficial to study whether, when the diagnosis of a mental health condition precedes the appearance of the physical health condition, that would affect the older persons’ quality of life. It would also be of interest to apply differential loads to medical conditions in future studies.
In conclusion, the present study contributes to the global knowledge of MPM in older people, illuminates health-related QoL differences among MPM patients and POM patients, and highlights the importance of non-modifiable characteristics associated with worse health-related QoL. Team collaboration between primary care physicians, psychiatrists (and other mental health providers), and social workers may be necessary to assess psychiatric and physical symptoms and provide for the care needs of older people with MPM.