Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CLINICAL RESEARCH
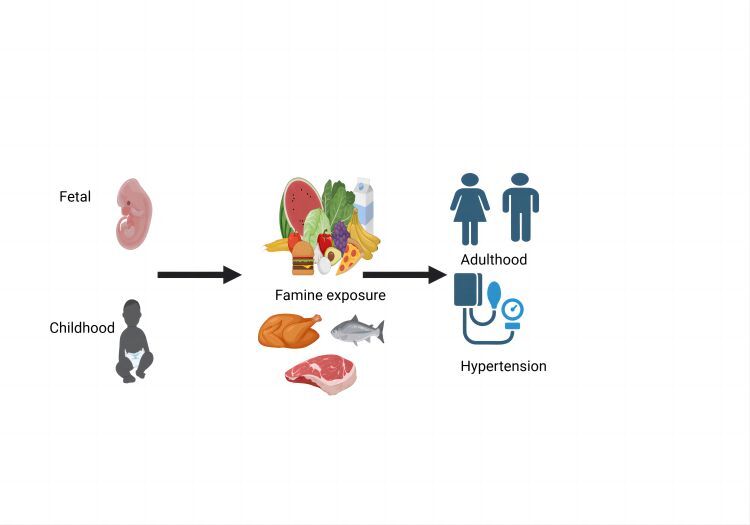
The effects of exposure to the Great Chinese Famine during the fetal stage and childhood on prevalence of hypertension in adulthood
1
Department of Geriatrics, National Key Clinic Specialty, Guangzhou First People’s Hospital, South China University of Technology, Guangzhou, China
2
Department of Cardiology, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Southern Medical University, Guangzhou, China
Submission date: 2024-02-04
Final revision date: 2024-03-09
Acceptance date: 2024-03-21
Online publication date: 2024-12-16
Corresponding author
Yu-qing Huang
Department of Cardiology, Guangdong Provincial People's Hospital, Guangdong Academy of Medical Sciences, Guangzhou 510080, China
Department of Cardiology, Guangdong Provincial People's Hospital, Guangdong Academy of Medical Sciences, Guangzhou 510080, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Many studies have found that famine exposure in early life was associated with higher prevalence of hypertension, but the results remain controversial. The aim was to examine the association of early life exposure to famine with hypertension in adulthood.
Material and methods:
The cross-sectional study enrolled about 100,000 adults from Guangdong province, China, who were born between 1 October 1952 and 30 September 1964. Participants were classified as non-exposed, fetal exposed, early-childhood exposed, mid-childhood exposed, and late-childhood exposed group according to birth data. Multivariable logistic regression, subgroup analysis, and sensitivity analysis were used to estimate the odds ratios (ORs) and confidence intervals (CIs) for the association between famine exposure and hypertension.
Results:
Among the 28,804 participants, the prevalence of hypertension in non-exposed, fetal, early-childhood, mid-childhood, and late-childhood exposed groups were 2686 (41.2%), 1777 (44.5%), 2998 (49.0%), 3196 (51.1%), 3192 (53.9%), respectively. Compared with the non-exposed group, the fully adjusted ORs of subjects exposed to the famine in the fetal, early-childhood, mid-childhood and late-childhood exposed groups were 1.10 (95% CI: 0.97–1.24, p = 0.143), 1.23 (95% CI: 1.10–1.37, p < 0.001), 1.39 (95% CI: 1.24–1.55, p < 0.001), and 1.55 (95% CI: 1.38–1.73, p < 0.001), respectively (p for trend < 0.001), and for the age-balanced group it was 1.37 (95% CI: 1.13–1.59, p < 0.001). Subgroup analyses showed that the effect of famine on hypertension was more pronounced in women and in the rural and overweight population.
Conclusions:
Exposure to famine at any stage in childhood, but not in the fetal stage, was significantly associated with higher prevalence of hypertension in adults, especially in women and in the rural and overweight population.
Many studies have found that famine exposure in early life was associated with higher prevalence of hypertension, but the results remain controversial. The aim was to examine the association of early life exposure to famine with hypertension in adulthood.
Material and methods:
The cross-sectional study enrolled about 100,000 adults from Guangdong province, China, who were born between 1 October 1952 and 30 September 1964. Participants were classified as non-exposed, fetal exposed, early-childhood exposed, mid-childhood exposed, and late-childhood exposed group according to birth data. Multivariable logistic regression, subgroup analysis, and sensitivity analysis were used to estimate the odds ratios (ORs) and confidence intervals (CIs) for the association between famine exposure and hypertension.
Results:
Among the 28,804 participants, the prevalence of hypertension in non-exposed, fetal, early-childhood, mid-childhood, and late-childhood exposed groups were 2686 (41.2%), 1777 (44.5%), 2998 (49.0%), 3196 (51.1%), 3192 (53.9%), respectively. Compared with the non-exposed group, the fully adjusted ORs of subjects exposed to the famine in the fetal, early-childhood, mid-childhood and late-childhood exposed groups were 1.10 (95% CI: 0.97–1.24, p = 0.143), 1.23 (95% CI: 1.10–1.37, p < 0.001), 1.39 (95% CI: 1.24–1.55, p < 0.001), and 1.55 (95% CI: 1.38–1.73, p < 0.001), respectively (p for trend < 0.001), and for the age-balanced group it was 1.37 (95% CI: 1.13–1.59, p < 0.001). Subgroup analyses showed that the effect of famine on hypertension was more pronounced in women and in the rural and overweight population.
Conclusions:
Exposure to famine at any stage in childhood, but not in the fetal stage, was significantly associated with higher prevalence of hypertension in adults, especially in women and in the rural and overweight population.
REFERENCES (52)
1.
Al-Makki A, DiPette D, Whelton PK, et al. Hypertension pharmacological treatment in adults: a world health organization guideline executive summary. Hypertension 2022; 79: 293-301.
2.
Lu J, Lu Y, Wang X, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet 2017; 390: 2549-58.
3.
Natsis M, Antza C, Doundoulakis I, et al. Hypertension in obesity: novel insights. Curr Hypertens Rev 2020; 16: 30-6.
4.
Liu MY, Li N, Li WA, Khan H. Association between psychosocial stress and hypertension: a systematic review and meta-analysis. Neurol Res 2017; 39: 573-80.
5.
Jarrin DC, Alvaro PK, Bouchard MA, et al. Insomnia and hypertension: a systematic review. Sleep Med Rev 2018; 41: 3-38.
6.
Gloria-Bottini F, Banci M, Neri A, Magrini A, Bottini E. Smoking and hypertension: effect of adenosine deaminase polymorphism. Clin Exp Hypertens 2019; 41: 548-51.
7.
Mannucci PM, Ancona C. Noise and air pollution as triggers of hypertension. Eur Heart J 2021; 42: 2085-7.
8.
Vallianou NG, Geladari E, Kounatidis D. Microbiome and hypertension: where are we now? J Cardiovasc Med (Hagerstown) 2020; 21: 83-8.
9.
Appel LJ. The effects of dietary factors on blood pressure. Cardiol Clin 2017; 35: 197-212.
10.
Azupogo F, Abizari AR, Aurino E, et al. Malnutrition, hypertension risk, and correlates: an analysis of the 2014 ghana demographic and health survey data for 15-19 years adolescent boys and girls. Nutrients 2020; 12: 2737.
11.
Du R, Zheng R, Xu Y, et al. Early-life famine exposure and risk of cardiovascular diseases in later life: findings from the REACTION Study. J Am Heart Assoc 2020; 9: e14175.
12.
Grey K, Gonzales GB, Abera M, et al. Severe malnutrition or famine exposure in childhood and cardiometabolic non-communicable disease later in life: a systematic review. BMJ Glob Health 2021; 6: e003161.
13.
van Abeelen A, de Rooij SR, Osmond C, et al. The sex-specific effects of famine on the association between placental size and later hypertension. Placenta 2011; 32: 694-8.
14.
Hult M, Tornhammar P, Ueda P, et al. Hypertension, diabetes and overweight: looming legacies of the Biafran famine. PLoS One 2010; 5: e13582.
15.
Liu L, Xu X, Zeng H, et al. Increase in the prevalence of hypertension among adults exposed to the Great Chinese Famine during early life. Environ Health Prev Med 2017; 22: 64.
16.
Yu C, Wang J, Li Y, et al. Exposure to the Chinese famine in early life and hypertension prevalence risk in adults. J Hypertens 2017; 35: 63-8.
17.
Zhang L, Yang L, Wang C, et al. Combined effect of famine exposure and obesity parameters on hypertension in the midaged and older adult: a population-based cross-sectional study. Biomed Res Int 2021; 2021: 5594718.
18.
Wang Y, Jin J, Peng Y, Chen Y. Exposure to Chinese famine in the early life, adulthood obesity patterns, and the incidence of hypertension: a 22-year cohort study. Ann Nutr Metab 2021; 77: 109-15.
19.
Lu J, Xuan S, Downing NS, et al. Protocol for the China PEACE (Patient-centered Evaluative Assessment of Cardiac Events) Million Persons Project pilot. Bmj Open 2016; 6: e10200.
20.
Linderman GC, Lu J, Lu Y, et al. Association of body mass index with blood pressure among 1.7 million chinese adults. JAMA Netw Open 2018; 1: e181271.
21.
Li C, Lumey LH. Exposure to the Chinese famine of 1959-61 in early life and long-term health conditions: a systematic review and meta-analysis. Int J Epidemiol 2017; 46: 1157-70.
22.
Huang YQ, Liu L, Yu YL, et al. The relationship between famine exposure during early life and carotid plaque in adulthood. Eur J Clin Nutr 2021; 75: 546-54.
23.
Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013; 34: 2159-219.
24.
Janssen I, Heymsfield SB, Allison DB, Kotler DP, Ross R. Body mass index and waist circumference independently contribute to the prediction of nonabdominal, abdominal subcutaneous, and visceral fat. Am J Clin Nutr 2002; 75: 683-8.
25.
Meng R, Lv J, Yu C, et al. Prenatal famine exposure, adulthood obesity patterns and risk of type 2 diabetes. Int J Epidemiol 2018; 47: 399-408.
26.
Wang Z, Zou Z, Yang Z, et al. The association between fetal-stage exposure to the China famine and risk of diabetes mellitus in adulthood: results from the China health and retirement longitudinal study. Bmc Public Health 2018; 18: 1205.
27.
Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289: 2560-72.
28.
Stein AD, Zybert PA, van der Pal-de BK, Lumey LH. Exposure to famine during gestation, size at birth, and blood pressure at age 59 y: evidence from the Dutch Famine. Eur J Epidemiol 2006; 21: 759-65.
29.
Roseboom TJ, van der Meulen JH, Ravelli AC, et al. Blood pressure in adults after prenatal exposure to famine. J Hypertens 1999; 17: 325-30.
30.
Stanner SA, Bulmer K, Andres C, et al. Does malnutrition in utero determine diabetes and coronary heart disease in adulthood? Results from the Leningrad siege study, a cross sectional study. BMJ 1997; 315: 1342-8.
31.
Wang Z, Li C, Yang Z, Zou Z, Ma J. Infant exposure to Chinese famine increased the risk of hypertension in adulthood: results from the China Health and Retirement Longitudinal Study. BMC Public Health 2016; 16: 435.
32.
Zhang L, Yang L, Wang C, et al. Individual and combined association analysis of famine exposure and serum uric acid with hypertension in the mid-aged and older adult: a population-based cross-sectional study. BMC Cardiovasc Disord 2021; 21: 420.
33.
Chen H, Nembhard WN, Stockwell HG. Sex-specific effects of fetal exposure to the 1959-1961 Chinese famine on risk of adult hypertension. Matern Child Health J 2014; 18: 527-33.
34.
Guo HJ, Ding X, Jiang W, et al. [Association analysis of famine exposure during early life and risk of hypertension in adulthood]. Zhonghua Yu Fang Yi Xue Za Zhi 2021; 55: 732-6.
35.
Zambrano E, Martinez-Samayoa PM, Bautista CJ, et al. Sex differences in transgenerational alterations of growth and metabolism in progeny (F2) of female offspring (F1) of rats fed a low protein diet during pregnancy and lactation. J Physiol 2005; 566: 225-36.
36.
Wu YT, Niubo AS, Daskalopoulou C, et al. Sex differences in mortality: results from a population-based study of 12 longitudinal cohorts. CMAJ 2021; 193: E361-70.
37.
Edwards MJ. Genetic selection of embryos that later develop the metabolic syndrome. Med Hypotheses 2012; 78: 621-5.
38.
Li Y, Jaddoe VW, Qi L, et al. Exposure to the Chinese famine in early life and the risk of hypertension in adulthood. J Hypertens 2011; 29: 1085-92.
40.
Jiang X, Ma H, Wang Y, Liu Y. Early life factors and type 2 diabetes mellitus. J Diabetes Res 2013; 2013: 485082.
41.
Heijmans BT, Tobi EW, Stein AD, et al. Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proc Natl Acad Sci USA 2008; 105: 17046-9.
42.
Vaiserman A, Lushchak O. Prenatal famine exposure and adult health outcomes: an epigenetic link. Environ Epigenet 2021; 7: dvab013.
43.
Ferreira VR, Jardim TV, Povoa TR, et al. Birth weight and its association with blood pressure and nutritional status in adolescents. J Pediatr (Rio J) 2018; 94: 184-91.
44.
Syme C, Shin J, Richer L, et al. Epigenetic loci of blood pressure. Circ Genom Precis Med 2019; 12: e2341.
45.
Wang Y, Weng P, Wan H, et al. Economic status moderates the association between early-life famine exposure and hyperuricemia in adulthood. J Clin Endocrinol Metab 2020; 105: dgaa523.
46.
Song C, Wang M, Chen Z, et al. Fetal exposure to chinese famine increases obesity risk in adulthood. Int J Environ Res Public Health 2020; 17: 3649.
47.
Abate KH, Abdulahi M, Abdulhay F, et al. Consequences of exposure to prenatal famine on estimated glomerular filtration rate and risk of chronic kidney disease among survivors of the great Ethiopian famine (1983-85): a historical cohort study. Nutr J 2021; 20: 19.
48.
Yu MA, Sanchez-Lozada LG, Johnson RJ, Kang DH. Oxidative stress with an activation of the renin-angiotensin system in human vascular endothelial cells as a novel mechanism of uric acid-induced endothelial dysfunction. J Hypertens 2010; 28: 1234-42.
49.
Iantorno M, Campia U, Di Daniele N, et al. Obesity, inflammation and endothelial dysfunction. J Biol Regul Homeost Agents 2014; 28: 169-76.
50.
Saxena T, Ali AO, Saxena M. Pathophysiology of essential hypertension: an update. Expert Rev Cardiovasc Ther 2018; 16: 879-87.
51.
Li C, Tobi EW, Heijmans BT, Lumey LH. The effect of the Chinese Famine on type 2 diabetes mellitus epidemics. Nat Rev Endocrinol 2019; 15: 313-4.
52.
Li J, Yang Q, An R, et al. Famine and trajectories of body mass index, waist circumference, and blood pressure in two generations: results from the CHNS From 1993-2015. Hypertension 2022; 79: 518-31.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.