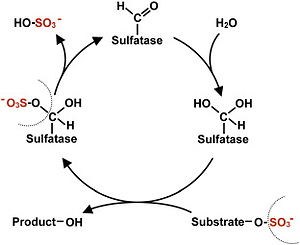
Multiple sulfatase deficiency is a rare human inherited disorder caused by pathogenic variants in the SUMF1 gene encoding the formylglycine-generating enzyme (FGE) that activates all known sulfatases [1, 2]. This protein is essential in the posttranslational modification of all sulfatase enzymes in the endoplasmic reticulum. Deficiency of FGE results in accumulation of multiple sulfated substrates in multiple tissues. A complex, progressive neurodegenerative disorder of early childhood, multiple sulfatase deficiency (MSD) manifests as systematic psychomotor retardation followed by loss of motor skills, speech, hearing, and vision [1, 3]. Although all MSD patients present these neurologic impairments, a wide range of other personalized clinical manifestations, such as facial features, hydrocephalus, chondrodysplasia punctata, ichthyosis, cardiac and pulmonary defects, hepatosplenomegaly, hydrops fetalis, recurrent ear infections, and eye problems, including corneal clouding and retinitis pigmentosa, can be variable for different patients in the first few years of life [4]. Sleep disturbance, feeding difficulties, constipation, spasticity, and hip dislocation are other frequent symptoms [5]. Brain magnetic resonance imaging (MRI) findings can also be variable with demyelination resembling metachromatic leukodystrophy (MLD), brain atrophy, corpus callosum hypoplasia, subcerebellar cysts, and hydrocephalus [6]. Diagnosis of MSD is commonly based on SUMF1 genetic testing; nonetheless, biochemical and genetic confirmation risk false-negative results. MSD could be missed on panels measuring limited sulfatases; therefore, identifying low activity levels of at least two sulfatase enzymes is recommended to confirm the MSD [7]. A consensus statement on the complex care and management of MSD patients was introduced at the first International Conference on MSD in 2017, providing the first clinical guidelines for MSD [8]. There is no curative therapy yet for MSD, and patients often face multiple health problems due to the complexity of the disease. Consequently, any therapeutic intervention with potential benefits to MCD patients is urgent.
Trehalose is a naturally occurring disaccharide composed of two glucose molecules. The sugar is found in various plants, bacteria, fungi, and insects, functioning in these organisms as a cryoprotectant against environmental and oxidative stress, as an energy source, and key structural component of bacterial cell walls [9]. Not only does basic and experimental research support trehalose in several models of disease [10–13], but several clinical trials have reported the efficacy and/or safety of trehalose in healthy individuals and diseased populations [14–16]. Trehalose is a safe compound, and no adverse effect has been reported at doses up to (50 g/a day); however, some trehalose-deficient patients have shown gastrointestinal side effects. The Joint FAO/WHO Expert Committee on Food Additives (JECFA), U.S. Food and Drug Administration (FDA), and the European Union recognized and approved trehalose as a safe additive for human consumption in 2000–2001 [9].
Evidence for IV trehalose was provided in patients with genetic lysosomal storage disease (LSD). Trehalose has many potential mechanisms of neuroprotective activities such as anti-aggregation, anti-inflammatory, antioxidant properties, and autophagy induction in both cell cultures and in vivo animal models [9–11]. Several lines of evidence suggest the chaperone-like activity of trehalose in neurodegenerative diseases (NDs) to prevent protein misfolding or aggregation and contribute to the clearance of accumulated proteins by promoting autophagy. As such, trehalose is emerging as a novel therapeutic avenue to repress oxidative stress and inflammation by decreasing the production of reactive oxygen species (ROS) and proinflammatory cytokines, such as interleukin-1β (IL-1β) and tumor necrosis factor-α (TNF-α), respectively [17]. The FGE defect causes sulfatase enzyme family deficiency, leading to increased sulfated lipids and mucopolysaccharides [1, 18]. Therefore, trehalose might be effective in attenuating adverse outcomes in MSD patients by reducing lipid accumulation, inflammation, and oxidative damage. Trehalose can be supplemented orally or administered intravenously; however, its absorption is decreased to 0.5% in the oral route due to enzymatic metabolization with trehalase appearing in the intestinal brush border, and IV trehalose administration is more efficient for clinical trials [9]. Nevertheless, oral administration of trehalose in both preclinical and clinical studies of oculopharyngeal muscular dystrophy (OPMD) and Machado-Joseph disease (MJD) can stabilize neurological impairment and improve the severity of clinical disease scores [15, 19].
There have been no published randomized controlled trials on trehalose efficacy in patients with MSD. Accordingly, we report on a case study investigating the efficacy of IV trehalose (15 g) once a week for 90 min during 3 months in a patient with MSD. In the current study, we present a girl with MSD who received trehalose for 12 weeks.
Methods
In the current study, the effects of IV trehalose were investigated in a female aged 9.5 years (weight 21.5 kg and height 120.6 cm) who was diagnosed with MSD by genetic testing and clinical observations. She was born from a consanguineous family, and the genotype analysis result was homozygous (Variant: Homozygous NM: 182760: exon4: c.G529C: p.A177P; ATM class 2- likely pathogenic) (Table I). Her parents signed an informed consent form, and the study protocol has been approved by the Ethics Committee of Mashhad University of Medical Sciences (ID: IRCT20130829014521N17), Mashhad, Iran. For 3 months, the subject received a pharmaceutical grade of trehalose as a 15% solution in 100 ml sterile sealed vials manufactured by Dr. Rajabi Pharmaceutical Company, Khorasan Razavi, Iran. A fasted blood sample was taken from the subject at W0 and W12 to evaluate safety.
Table I
Summarized demographic information of the participant
| Age | Gender | Variance region | Gene | Diagnosis | |
|---|---|---|---|---|---|
| Patient | 9.5 | F | Homozygous NM: 182760: exon4: c.G529C: p. A177P | SUMF1 | MSD |
Quality of life assessment
The TAPQOL (TNO-AZL Preschool children Quality of Life) index was used to assess the physical, social, emotional, and cognitive function of the patient. TAPQOL is a multidimensional questionnaire-parent form with 43 items comprising 12 scales to measure health-related quality of life (HRQoL) in preschool children (aged 2–48 months). The questionnaire is designed so that each phrase examines the existence of a specific problem in the past month. The answers are in the form of a Likert scale with five options: always (0), often (1), sometimes (2), very little (3), and never (4). The score obtained for each subscale will be between 0 and 100. Each phrase is scored as follows: always, 0; often, 25; sometimes, 50; very low, 75; and never, 100. A score less than 25 indicates a low quality of life, a score between 25 and 75 indicates an average quality of life, and a score above 75 indicates a high quality of life [20].
Imaging detection
Hepatosplenomegaly is a clinical feature and diagnosis in MSD patients; therefore, we measured spleen and liver size using ultrasonography and volumetric analysis at baseline and the end of the study. Brain MRIs were also performed at W0 and W12.
Serum biomarkers
To evaluate liver function, serum levels of alanine aminotransferase (ALT) and aspartate transaminase (AST) were measured using a colorimetric assay kit to evaluate liver function. Moreover, the antioxidant activity of trehalose was assessed by analyzing parameters related to oxidant/antioxidant status, including serum malondialdehyde (MDA) levels and superoxide dismutase (SOD) activity, before and after the intervention.
Intravenous trehalose did not have any adverse effects and was well tolerated. Although initially some nausea and constipation were experienced by the patient, these events decreased and she gained some weight. The TAPQOL score increased from 67 at W0 to 80 at W12, suggesting an improved health-related quality of life. The patient’s nausea and constipation recovered, and gross motor problems such as difficulties with walking, running, and balance improved. Also, she gained a little weight after 3 months of trehalose treatment. Abdominal ultrasonography was normal without hepatosplenomegaly at W0, and the spleen size was found to have decreased from 88 mm to 80 mm by W12. MRI images revealed symmetrical periventricular white matter signal abnormalities. Oxidative stress (MDA levels) decreased from 8.4 to 6.1 (nmol/ml) and SOD activity increased from 1.8 to 2.3 (U) by W12; similarly, ALT and AST levels increased mildly by W12 (Table II).
Discussion
Multiple sulfatase deficiency is an autosomal recessive lysosomal storage disorder. MSD is due to a formylglycine-generating enzyme (FGE) deficiency encoded by the sulfatase modifying factor 1 (SUMF1) gene which causes increased sulfated lipids and mucopolysaccharides. Accumulation of glycosaminoglycans (GAGs) and sulfatides is a common feature of the MSD phenotype, as seen in mucopolysaccharidoses (MPS). This abnormal storage leads to several pathological consequences that can trigger a high level of apoptosis by activating pro-apoptotic genes and proteins [21]. Currently, no effective treatment is available for MSD patients [18].
Previously, there had been no research on trehalose effects in a patient with MSD. This study investigated the potential efficacy of IV trehalose (at a dose of 15 g/week) in a patient with MSD. The dose of 15 g/week was selected based on evidence from our previous research showing the safety and efficacy of the dose in patients with Niemann-Pick disease [14] as well as from another clinical study conducted in patients with Machado-Joseph disease (MJD) [15]. Our results suggested that trehalose could improve quality of life during 12 weeks of intervention without any significant adverse effects. The patient’s nausea and constipation recovered, and she gained a little weight. We hypothesize that trehalose could slow disease progression and improve neuropathologic features by decreasing the accumulation of multiple sulfated substrates and sphingolipid deposition after 3 months of treatment. Furthermore, the development of gross motor skills, such as difficulties with walking, running, and balance, was observed.
Owing to the well-documented role of impaired autophagy in the pathogenesis of LSDs, induction of the autophagy-lysosomal pathway (ALP) has been actively sought as a potentially efficient approach to enhance the clearance of accumulated toxic metabolites [22]. In this respect, trehalose is a potential candidate given its capacity to activate transcription factor EB (TFEB) and stimulate the ALP in several cellular and experimental models. Furthermore, trehalose has been shown to stimulate autophagy via an mTOR-independent pathway [23–25]. The present findings corroborate those of our earlier study in patients with Niemann-Pick A/B disease, in whom a significant improvement in the quality of life (assessed using TAPQOL score) was observed following an identical IV trehalose protocol over 12 weeks as followed in the current study [14].
Hepatosplenomegaly accompanied by liver failure is a typical sign in MSD patients. We observed a slight decrease in the spleen dimensions after 12 weeks of treatment, although neither ALT nor AST was affected. Since oxidative and endoplasmic reticulum stresses are common mediators of apoptosis in LSDs, decreasing oxidative stress might help mitigate some clinical progression of MSD [26]. Preclinical studies demonstrated that trehalose upregulated antioxidant gene expression of antioxidant enzymes such as SOD through the promotion of nuclear translocation of Nrf2 and remarkably reduced the production of ROS in a dose-dependent manner [27, 28]. In line with these studies, we examined serum MDA levels and SOD activity after trehalose treatment to evaluate whether the sugar affected the oxidative stress in the MSD patient. Increased SOD activity accompanied by a decrease in MDA confirmed the improved oxidative stress in this patient. Finally, radiologic findings in our patients were similar to previously reported cases, with the most common MRI finding being periventricular white matter abnormalities [29].
In conclusion, treating MSD patients with 15 g/week of trehalose may be effective in improving disease symptoms caused by lipid accumulation; however, the length of treatment in our research is also not long enough to evaluate trehalose’s effects on behavioral problems. Finally, future dose-ranging studies are needed to indicate the optimal therapeutic dose of trehalose and determine whether trehalose has clinical efficacy in patients with MSD.
Trial registration: IRCT20130829014521N17.