Introduction
Iodine is a crucial trace element that the human body needs and a crucial component in the production of thyroid hormones, which participate in the body’s material and energy metabolism and promote growth and development [1]. Thus, the physiological function of iodine is mainly manifested by the action of thyroid hormones, and insufficient iodine intake results in inadequate levels of thyroid hormone synthesis, which causes a range of diseases that are collectively referred to as iodine deficiency diseases [2]. International organizations such as the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) have prioritized iodine insufficiency diseases, vitamin A insufficiency disease, and iron insufficiency anemia as the top three micronutrient deficiency diseases for worldwide prevention, control and elimination [3–7]. The need to pay more attention to preventing iodine deficiency diseases, especially in children, is underscored by the fact that they are the only known and preventable diseases that cause mental developmental disorders and brain damage [3, 8].
However, iodine deficiency is still common in low- and middle-income countries (LIMCs). Over 50% of preschool-aged children in 13 countries suffer from iodine shortage, while more than 40% of African children suffer from iron-deficiency anemia [6, 9]. Moreover, severe iodine deficiency in Ethiopian women during pregnancy is known to cause approximately 50,000 stillbirths each year [10, 11].
No comparable assessments of the burden of iodine deficiency have been conducted at the worldwide, regional and national levels. Therefore, in this study, we comprehensively assessed the incidence of iodine deficiency at the global, regional and national levels using data gathered from 204 nations and territories during the Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019.
Material and methods
Overview
Utilizing the most recent epidemiological data sources and enhanced standardization techniques, the Global Burden of Disease Study 2019 (GBD 2019) assessed the occurrence, popularization, death rate, years of life lost (YLLs), years lived with disability (YLDs), and disability-adjusted life-years (DALYs) associated with 369 diseases and injuries for both genders and 204 nations and territories [11, 12]. The information is available via the GHDx query tool (http://ghdx.healthdata.org/gbd-results-tool) for the Global Health Data Exchange. This study is publicly available and does not require ethical approval.
Data sources
The primary sources of the initial data assessed by the GBD 2019 for iodine deficiency were household surveys, civil registration and vital statistics, disease registries, health service usage, air pollution monitors, satellite imaging, sickness notifications, and censuses [12]. Iodine deficiency was determined by the 10th revision of the International Classification of Diseases and Injuries (ICD-10) codes E00–E02.
Estimation of incidence and DALYs
To estimate the incidence of significant iodine insufficiency and the changes in DALYs, age-standardized rates and EAPC were computed for these two metrics. Following age standardization, the age-standardized DALYs rates represent the sum of YLLs and years lived with a disability per 100,000 people. The ASI rates represent the number of cases per 100,000 people. The calculation of DALYs involved adding up years lost as a result of disability and YLLs, which included both the fatal and the non-fatal burden.
Statistical analysis
The age-standardized rates trend is indicated by the EAPC [13]. The following formula is utilized: y = a + bx + ε, where x = calendar year and y = ln (age-standardized rates). Additionally, EAPC = 100 × (exp (β) –1), where β is the slope b’s predicted value. The 95% confidence interval (CI), where the standard error is derived from the fitted regression line, is then computed once again using the aforementioned procedure. When both the estimated EAPC and its 95% confidence interval’s lower bound were greater than zero, the age-standardized rates were deemed to be increasing. In contrast, age-standardized rates were deemed to be declining if both the estimate of EAPC and its upper 95% confidence interval (CI) were less than 0. If not, the age-standardized rates were considered to have remained steady throughout time.
Results
Change in the incidence of iodine deficiency in different regions
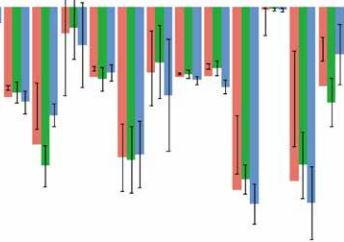
As shown in Table I and Figure 1 A, compared to locations with other SDI levels in 2019, the ASI rate of iodine deficiency was significantly greater in low- and low-middle-SDI values. In 2019, Low-spatial SDI regions had the greatest ASI rates of iodine insufficiency (205.01 per 100,000 people; 95% UI: 167.11 to 248.21), followed by Low-middle SDI regions (146.76 per 100,000 population; 95% UI:, 114.94 to 184.41). In contrast, the Low-middle SDI zones, where the EAPC was highest, saw the greatest drop in the ASI rate of iodine insufficiency (–1.55; 95% CI: –1.86 to –1.24), followed by that in Low SDI zones (EAPC = –0.83; 95% CI: –0.98 to –0.69). The ASI rate and its EAPC (ρ = –0.294, p < 0.0010, Supplementary Figure S3 A and the SDI (ρ = –0.164, p = 0.019, Supplementary Figure S3 B) showed negative associations. Additionally, it was discovered that locations with greater SDI in 1990 and 2019 had higher proportions of incident instances of iodine insufficiency in the 50–69 and 70+ year old groups, and that a region’s proportion of incident cases of iodine deficiency in young people decreased with increasing SDI (Supplementary Figure S4 A, B). The annual percentages of iodine deficiency incidence in all age groups remained stable year after year (Supplementary Figure S5 A). The incidence of iodine deficiency in people aged 15–49 years was much higher than that in other people in all SDI zones (Supplementary Figure S4 A, B). Globally, the iodine deficiency incidence rate peaked at 20–24 years globally and in all other regions (Supplementary Figure S7).
Table I
Age-standardized incidence rate of iodine deficiency in 1990 and 2019 and its temporal trends
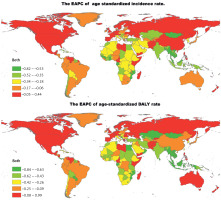
Prevalence of iodine deficiency in different geographical areas
Central sub-Saharan Africa had the highest area-level ASI rates of iodine insufficiency in 2019 (458.95 per 100,000 population; 95% UI: 371.55 to 555.75), South Asia (211.47 per 100,000 population; 95% UI: 164.69 to 266.20) and Eastern sub-Saharan Africa (185.56 per 100,000 population; 95% UI: 148.21 to 228.82), whereas the lowest ASI rate of iodine deficiency in 2019 was in Oceania (4.31 per 100,000 population; 95% UI: 3.28 to 5.62; Table I, Supplementary Table SII). From 1990 to 2019, the ASI rate of iodine deficiency increased the most in East Asia (EAPC = 0.17; 95% CI: –0.28 to 0.62), and decreased the most in Central Asia (EAPC = –2.16; 95% CI: –2.57 to –1.75) and in Southeast Asia (EAPC = –1.94; 95% CI: –2.16 to –1.72; Table I, Figure 1 A, Supplementary Table SII).
Somalia had the highest ASI rate of iodine deficiency nationally in 2019 (725.15 per 100,000 population; 95% UI: 591.27 to 869.53), followed by the Democratic Republic of the Congo (549.20 per 100,000 population; 95% UI: 443.41 to 665.68) and Djibouti (476.63 per 100,000 population; 95% UI: 379.22 to 582.48), whereas the lowest ASI rates of iodine deficiency were in Samoa (2.65 per 100,000 population; 95% UI: 1.90 to 3.50), American Samoa (2.79 per 100,000 population; 95% UI: 2.02 to 3.69) and Guam (2.88 per 100,000 population; 95% UI: 2.11 to 3.80) (Supplementary Tables SI and SIII). The Philippines saw the most noticeable rise in the ASI rate of iodine deficiency (EAPC = 1.32; 95% CI: 0.30 to 2.34), followed by Pakistan (EAPC = 0.64; 95% CI: 0.56 to 0.71) and Nepal (EAPC = 0.48; 95% CI: –0.31 to 1.09) (Supplementary Tables SI, SIII and Figure 2 A). The ASI rate of iodine deficiency increased most in females in the Philippines (EAPC = 1.58; 95% CI: 0.49 to 2.69), Nepal (EAPC = 1.10; 95% CI: 0.28 to 1.94) and Pakistan (EAPC = 0.85; 95% CI: 0.76 to 0.94), whereas it increased most in males in the Philippines (EAPC = 0.96; 95% CI: 0.06 to 1.88), Somalia (EAPC = 0.40; 95% CI: 0.28 to 0.52), Romania (EAPC = 0.39; 95% CI; 0.10 to 0.69) and the Republic of Moldova (EAPC = 0.39; 95% CI: –0.21 to 1.00) (Supplementary Tables SI and SIII). The incidence rate (per 100,000) of iodine insufficiency by age in various nations in 2019 is displayed in Supplementary Table SV.
Global changes in DALYs due to iodine deficiency
The total worldwide DALYs due to iodine deficiency in 1990 were 2,499,955.19 (95% UI: 1,534,317.54 to 4,033,662.53) in 1990, and decreased to 2,438,598.59 (95% UI: 1,372,657.05 to 4,238,613.26) in 2019. Between 1990 and 2019, the age-standardized DALY rate of iodine insufficiency dropped to 1.35 EAPC (95% CI: –1.45 to –1.25; Table II, Figure 1B, Supplementary Figure S1 D). Between 1990 and 2019, the age-standardized DALY rate for iodine insufficiency fell for both genders (males: EAPC = –1.76; 95% CI: –1.91 to –1.61; females: EAPC = –1.08; 95% CI: –1.15 to –1.01) (Table II, Figure 1 B, Supplementary Figures S1 E, F, 2). However, males experienced a lower age-standardized DALY rate of iodine insufficiency from 1990 to 2019 than did females (Table II).
Table II
Age-standardized DALY rate of iodine deficiency in 1990 and 2019 and its temporal trends
The Low SDI quintile had the most age-standardized DALYs from iodine deficiency in 2019 (78.06 per 100,000 population; 95% UI: 45.66 to 133.80), followed by that of the Low-middle SDI quintile (50.55 per 100,000 population; 95% UI: 29.32 to 86.65) (Table II). All SDI regions saw a drop in the age-standardized DALYs caused by iodine deficiency, with the Low-middle SDI regions experiencing the biggest decline (–2.37; 95% CI: –2.52 to –2.22; Table II, Figure 1 B).
Furthermore, there was a negative correlation between the age-standardized DALY rate and the EAPC of the iodine deficiency-related DALY rate (ρ = –0.185, p = 0.008, Supplementary Figure S3 C) and the SDI (ρ = –0.192, p = 0.006, Supplementary Figure S3 D). The age-standardized DALY of iodine insufficiency in people aged 15–49 years was much higher than that in other people in all SDI zones (Supplementary Figures S4 C, D). The annual percentages of iodine deficiency age-standardized DALY in all age groups remained stable every year (Supplementary Figure S5 B). Globally, the iodine deficiency DALY rate increased with age globally, and in all other regions (Supplementary Figure S8). The male-to-female rate of DALYs from iodine deficiency peaked in the 90–94 age range across all age groups globally (Supplementary Figure S6 A), peaked in the age range of 95 and over in High SDI areas; in the age range of 15 and 19 in High-middle SDI regions; in the age range of 90 and 94 in Middle SDI regions and Low-middle SDI regions; and in the age range of 95 and over in Low SDI regions (Supplementary Figures S6 B–F).
Change in DALYs due to iodine deficiency in different geographical areas
Central sub-Saharan Africa had the greatest age-standardized DALYs from iodine deficiency in 2019 (158.75 per 100,000 population; 95% UI: 81.96 to 291.75), South Asia (72.78 per 100,000 population; 95% UI: 42.19 to 125.52) and Eastern sub-Saharan Africa (60.38 per 100,000 population; 95% UI: 33.17 to 107.57). Andean Latin America has the lowest age-standardized DALYs from iodine deficiency (1.02 per 100,000 population; 95% UI: 0.51 to 1.89), Tropical Latin America (1.12 per 100,000 population; 95% UI: 0.50 to 2.15) and Southern Latin America (1.49 per 100,000 population; 95% UI, 0.67 to 2.83; Table II and Supplementary Table SII). Iodine deficiency-related age-standardized DALYs declined across all geographic areas. The Southeast Asian area had the largest drop in age-standardized DALYs associated with iodine deficiency (EAPC = –4.30; 95% CI: –5.12 to –3.47), followed by Central Asia (EAPC = –2.92; 95% CI: –3.52 to –2.32) and North Africa and Middle East (EAPC = –2.66; 95% CI: –2.90 to –2.42; Table II, Figure 1 B and Supplementary Table SII).
The nations with the greatest age-standardized DALY rates of iodine deficiency in 2019 were Somalia (274.38, 95% UI: 152.68 to 481.43), the Democratic Republic of the Congo (193.06, 95% UI: 100.63 to 358.72) and Djibouti (151.77, 95% UI: 74.28 to 284.42). In 2019, Samoa had the lowest age-standardized DALY rates of iodine deficiency among all nations (0.43, 95% UI: 0.19 to 0.85), followed by American Samoa (0.45, 95% UI: 0.19 to 0.89) and Guam (0.47, 95% UI: 0.21 to 0.93) (Supplementary Tables SI and SIV). The age-standardized DALY rate of iodine deficiency declined most in Equatorial Guinea (EAPC = –8.10; 95% CI: –9.05 to –7.14) and increased the most in Nepal (EAPC = 0.55, 95% CI: –0.08 to 1.18) (Supplementary Tables SI, SIV and Figure 2 B). Females saw the largest drop in the age-standardized DALY rate (EAPC = –7.87; 95% CI: –8.79 to –6.93) in Equatorial Guinea and it increased most in females (EAPC = 1.18; 95% CI: 0.34 to 2.02) in Nepal. Males had the largest declines in the age-standardized DALY rate (EAPC = –8.20; 95% CI: –9.28 to –7.11) in Equatorial Guinea and it increased most in males (EAPC = 0.52; 95% CI: 0.19 to 0.85) in Romania (Supplementary Tables SI and SIV). Supplementary Table SVI displays the age distributions of the mortality rates (per 100,000) due to iodine deficiency in various nations in 2019.
Discussion
Our comprehensive assessment of the worldwide, regional, and national impact of iodine deficiency revealed a decline in the ASI and disability-adjusted life year (DALY) rates between 1990 and 2019. This is likely due to countries worldwide taking steps to eliminate iodine deficiency by improving the iodine nutritional situation of their people via advocating diversity of diet and fortifying bread, milk, water and table salt with iodine. Due to the effectiveness, safety, simplicity and low cost of salt iodization, prevention and control measures based on this method are currently most commonly used [14, 15].
The implementation of salt iodization programs such as universal salt iodization (USI) have led to decreases in the iodine deficiency rate worldwide, such that the current global iodine nutritional status has significantly improved compared to before such efforts were instigated [9, 16–18]. USI is hailed as a public health success story, as 75% of the world’s population was estimated in 2016 to use iodized salt in a total of 130 countries. The iodine intake is insufficient in 15 countries, sufficient in 102 and excessive in 10. Among the 15 countries with insufficient intake, only two are classified as moderately deficient and 13 as mildly deficient [15, 19]. In South Africa, mandatory iodization of table salt, at a level of 40–60 ppm, replaced voluntary iodization in December 1995, using potassium iodate as the fortifier because of its stability in warm climates, rather than potassium iodide that is used in North America and Europe; the level of fortification was subsequently revised in 2007 to allow a wider range, namely 35–65 ppm [20]. The iodization program has effectively addressed iodine deficiency in the country. Salt iodization is recommended by organizations such as the WHO, because salt is widely consumed by virtually all population groups in all countries, with little seasonal variation in consumption; salt production is generally limited to a few centers, facilitating quality control; technology for salt iodization is well established and relatively easy to transfer to less developed countries; iodization does not affect the organoleptic properties of salt, and therefore, consumer acceptability is high; iodization is very inexpensive [21].
However, although almost all countries have eliminated severe iodine deficiency, residents of many countries still face the risk of a mild to moderate iodine shortage [22, 23] because their iodine intake remains insufficient. This is a serious public health problem and has been addressed by recommendations and guidelines on iodine fortification and supplementation published by the WHO, UNICEF and the Iodine Global Network [16, 24–26].
In 2019, regions with low and low-middle SDI values had a significantly higher ASI rate of iodine insufficiency than did regions with other SDI values. The percentage of households utilizing table salt that has been sufficiently iodized is the current USI performance measure. However, as the world’s intake of processed foods and sauces rises, the percentage of table salt in dietary salt is decreasing [27]. Throughout the past several decades, there has been a notable increase in the consumption of processed foods and condiments, particularly in LMICs, due to factors such as rising incomes, urbanization, the increased participation of women in the labor force and changes in lifestyles and choices [28, 29]. For instance, studies conducted in Bangladesh, Nepal, India, Indonesia, and Vietnam have demonstrated that industrially produced food – that is, processed food with both high and low value added – accounts for about three-quarters of household food purchases in urban areas and more than half in rural areas [27]. In addition, in Eastern and Southern Africa, one third of the food market comprises highly processed foods [30, 31]. In rural and urban areas, the relative proportion of this market share increases with income; that is, as incomes rise, dietary trends shift away from the consumption of staples, such as grains, toward the consumption of fruits, vegetables, animal protein, dairy, processed products and ready-made meals [32].
We found that the incidence of global iodine deficiency was greatest in populations aged 20–24, in both sexes. Iodine deficiency is also common in children and adolescents, and the WHO estimates that 285 million school-age children in nations with chronic iodine shortage are vulnerable to iodine-related problems [33]. Studies have suggested that although iodine deficiency can cause growth retardation and brain damage in humans, it is an independent cause that is easily preventable [34]. Compared to other micronutrient deficiencies, deficiencies in iodine, iron, zinc, and vitamin A remain major public health problems. Deficiencies of iron, zinc and vitamin A often coexist, possibly because of similar causal factors, such as (1) inadequate dietary intake and/or absorption from predominantly plant-based diets; (2) sub-optimal breast feeding practices; (3) diseases that either induce excessive losses or impair use of the micronutrients; and (4) physiological states that increase requirements, such as periods of rapid growth during childhood and pregnancy. Unlike the micronutrient deficiencies mentioned above, iodine deficiency mainly occurs in regions of low soil iodine content [35]. Most iodine is found in the oceans as iodide, and regions of glaciations, heavy rainfall and floods tend to have low iodine soil content, which leads to iodine deficiency in plants and animals grown on these soils. Consequently, populations in such areas that depend on locally grown foods are at risk of developing iodine deficiency. USI is the main strategy proposed by the WHO, and thus, the addition of an appropriate amount of iodine to people’s daily intake of table salt has become the most economical and effective measure to prevent iodine deficiency diseases [17]. Nevertheless, more attention must be paid to groups at high risk of iodine deficiency, and an iodine deficiency disease monitoring project should be established to carry out urinary iodine monitoring, screen high-risk groups and implement preventive measures [36].
Between 1990 and 2019, the East Asian area saw the largest increase in the ASI rate of iodine deficiency, with increasing prevalence in countries such as Nepal, Pakistan, and the Philippines. The Philippines is addressing iodine deficiency in its population through a government policy of adding iodine to all salt intended for animal and human consumption [23]. However, in Pakistan, the consumption of iodized salt is even lower than that in some low-income African countries [26], which is ultimately due to a lack of proper planning and political will and oversight. We believe that legislation on salt iodization, especially mandatory legislation under the National Food Law, will help to popularize the use of iodized salt in Pakistan [25].
At present, USI is the most simple, economical, effective and internationally recognized measure to control iodine deficiency. The WHO recommends an iodine intake of 150 µg/day for adults [32]. Therefore, to reduce iodine deficiencies, effective measures and appropriate monitoring indicators must be employed to monitor the iodine nutritional status of iodine-supplemented populations and normal populations. Care must also be taken to survey for the negative effects of both insufficient and excessive supplementation [7, 22, 37]. Thus, iodine supplementation measures should be tailored to the iodine levels in the drinking water and diet of people in a given region. In regions with low levels of iodine in food and/or drinking water that humans consume, iodized salt supplementation should be actively promoted, whereas in regions where drinking water and/or people’s diets have high iodine content, iodized salt supplementation should be stopped or iodized salt with a lower iodine content should be provided. Such active monitoring of iodine nutrition can both effectively control iodine deficiency and prevent the consequences of excessive iodine intake [38].
Based on the current situation, East Asian countries should conduct a comprehensive survey and assessment of the iodine nutritional status of their population. This should involve an examination of their populations’ iodine nutritional status, dietary conditions and iodized salt intake, as well as the determination of the iodine concentrations in the external environment (e.g., soil and drinking water).
This was the first research to cover the global burden of iodine deficiency in such a thorough and complete manner. Crucially, we also classified high-risk groups according to age and sex. Our research will be helpful in determining priorities and allocating resources at the national, regional, and international levels. This study has a limitation. That is, the GBD 2019 included bias adjustments to account for survey procedures, low-quality sampling, and other methodological flaws in data sources, but the quality and volume of data entered into the models ultimately determine how accurate the estimates for iodine shortage are. Future work should involve more rigorous surveys of population-wide iodine intake, with a particular focus on the above-mentioned high-risk regions.
In conclusion, we discovered that despite the global ASI and DALY rates of iodine deficiency decreasing between 1990 and 2019, East Asia, the Philippines, Pakistan and Nepal continue to suffer from a substantial burden of iodine deficiency. These regions should thus be targeted for intervention.