Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
Editor's Choice
METABOLIC DISORDERS / RESEARCH PAPER
Telomere length across the spectrum of metabolic health – an analysis from the LIPIDOGEN2015 study
1
Faculty of Medicine, the John Paul II Catholic University of Lublin, Lublin, Poland
2
Medical University of Lodz, Department of Preventive Cardiology and Lipidology, Poland
3
Medical University of Silesia, Department of Pharmacology, Faculty of Medical Sciences in Zabrze, Poland
4
University of Opole, Department of Biology and Genetics, Institute of Medical Sciences, Poland
5
Medical University of Silesia, Department of Medical and Molecular Biology, Faculty of Medical Sciences in Zabrze, Poland
6
University of Opole, Department of Cardiology, Institute of Medical Sciences, Poland
7
Polish Mother’s Memorial Hospital Research Institute, Department of Genetics, Poland
8
University of Opole, Department of Family Medicine and Public Health, Institute of Medical Sciences, Poland
These authors had equal contribution to this work
Submission date: 2024-08-17
Final revision date: 2024-09-29
Acceptance date: 2024-10-31
Online publication date: 2024-10-31
Corresponding author
Martyna Fronczek
Medical University of Silesia, Department of Pharmacology, Faculty of Medical Sciences in Zabrze, Katowice, Poland
Medical University of Silesia, Department of Pharmacology, Faculty of Medical Sciences in Zabrze, Katowice, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Telomere length is a cellular aging marker and correlates with various cardiovascular disease (CVD) risk factors. The current study assessed the association between obesity, metabolic syndrome (MetS), and telomere length.
Material and methods:
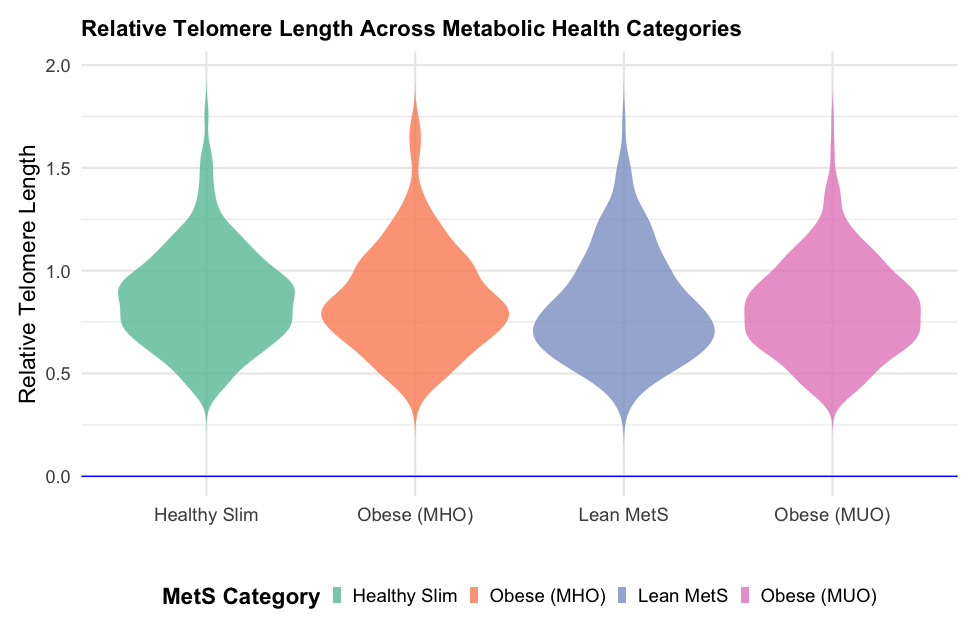
The LIPIDOGRAM&LIPIDOGEN2015 study was conducted in primary care in 2015-2016. Recruited patients to the LIPIDOGEN2015 cohort (n=1788) were a random subset of patients of the LIPIDOGRAM2015 (n=13,724) study. For the aims of this analysis, the recruited patients were divided into four groups based on the presence of MetS: healthy slim (HS), metabolically healthy obese (MHO), non-obese with MetS (NOMS), and metabolically unhealthy obese (MUO). Relative telomere length (RTL) was measured using quantitative polymerase chain reaction (qPCR).
Results:
1516 patients (85%; females - 59.7%, mean age- 50.3 years) were included for final analyses. An increase in body mass index (BMI), waist circumference, prevalence of diabetes mellitus, hypertension, dyslipidemia, and history of myocardial infarction moving from HS to MUO were observed. MUO group exhibited the highest triglycerides and lowest high-density lipoprotein (HDL-C) levels. Univariable regression analyses indicated that NOMS (p=0.038) and MUO (p=0.003) were associated with significantly decreased RTL. After adjustment for age, gender, education, smoking, place of residence, and myocardial infarction, the association was no longer statistically significant.
Conclusions:
Despite the lack of statistical significance in the multivariate analysis, the univariate results suggest that both MUO and NOMS phenotypes contribute to the shortening of telomere length. These results may also indicate that MetS, irrespectively on obesity occurrence, is responsible for the shortened lifespan.
Telomere length is a cellular aging marker and correlates with various cardiovascular disease (CVD) risk factors. The current study assessed the association between obesity, metabolic syndrome (MetS), and telomere length.
Material and methods:
The LIPIDOGRAM&LIPIDOGEN2015 study was conducted in primary care in 2015-2016. Recruited patients to the LIPIDOGEN2015 cohort (n=1788) were a random subset of patients of the LIPIDOGRAM2015 (n=13,724) study. For the aims of this analysis, the recruited patients were divided into four groups based on the presence of MetS: healthy slim (HS), metabolically healthy obese (MHO), non-obese with MetS (NOMS), and metabolically unhealthy obese (MUO). Relative telomere length (RTL) was measured using quantitative polymerase chain reaction (qPCR).
Results:
1516 patients (85%; females - 59.7%, mean age- 50.3 years) were included for final analyses. An increase in body mass index (BMI), waist circumference, prevalence of diabetes mellitus, hypertension, dyslipidemia, and history of myocardial infarction moving from HS to MUO were observed. MUO group exhibited the highest triglycerides and lowest high-density lipoprotein (HDL-C) levels. Univariable regression analyses indicated that NOMS (p=0.038) and MUO (p=0.003) were associated with significantly decreased RTL. After adjustment for age, gender, education, smoking, place of residence, and myocardial infarction, the association was no longer statistically significant.
Conclusions:
Despite the lack of statistical significance in the multivariate analysis, the univariate results suggest that both MUO and NOMS phenotypes contribute to the shortening of telomere length. These results may also indicate that MetS, irrespectively on obesity occurrence, is responsible for the shortened lifespan.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.