Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CLINICAL RESEARCH
Symptom characteristics in self-observation and directional preference in patients with low back pain undergoing McKenzie therapy
1
Department of Physiotherapy, Faculty of Health Sciences, Wroclaw Medical University, Wroclaw, Poland
Submission date: 2023-11-30
Final revision date: 2024-02-12
Acceptance date: 2024-03-25
Online publication date: 2024-06-06
Corresponding author
Ewa Gieysztor
Department of Physiotherapy Faculty of Health Sciences Wroclaw Medical University Wroclaw, Poland
Department of Physiotherapy Faculty of Health Sciences Wroclaw Medical University Wroclaw, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction:
The McKenzie Method, also known as Mechanical Diagnosis and Therapy (MDT), is currently one of the most well-known methods for diagnosing and treating spinal and limb pain syndromes. The study aimed to analyze the self-observations of the symptom characteristics in comparison with directional preference (DP) in the therapeutic procedures.
Material and methods:
A study was conducted based on the therapeutic records of patients treated by MDT. The study was carried out on a group of 302 patients. The analysis of the symptoms in self-observations of the patient was conducted. The data were compared using various schemes: gender, age range, type of work, classification, positional preferences, and applied directional procedures.
Results:
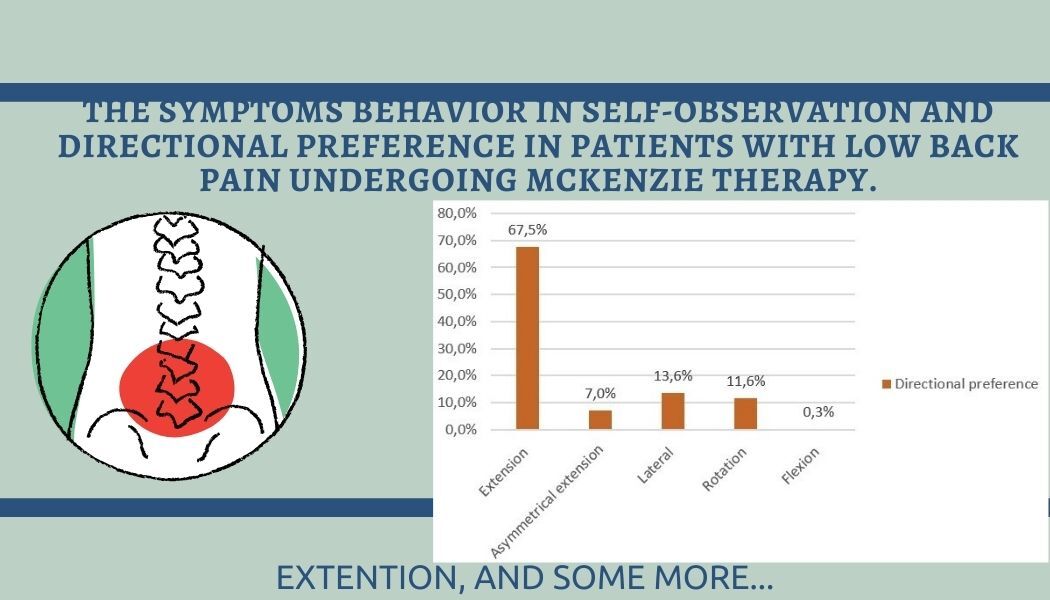
Patients more commonly indicate the movements that increase symptoms. The individuals treated with the extension DP reported an increase in pain symptoms during sitting, bending, and standing. The majority of patients were classified into the D3 group and treated with an extension-based approach. With increasing age, the number of individuals classified as D1 decreased, while those classified as D5 increased. In the oldest age group, the number of other than extensional therapeutic DP increased.
Conclusions:
Patients are not able to indicate the movements that decrease the symptoms while the movements that increase the symptoms are better recognized. Certified physiotherapists should educate about the centralization phenomenon and directional preference. While extension movements generally lead to a reduction in reported pain symptoms, they are not the only movements that can centralize symptoms and should not be applied without a thorough examination of the patient.
The McKenzie Method, also known as Mechanical Diagnosis and Therapy (MDT), is currently one of the most well-known methods for diagnosing and treating spinal and limb pain syndromes. The study aimed to analyze the self-observations of the symptom characteristics in comparison with directional preference (DP) in the therapeutic procedures.
Material and methods:
A study was conducted based on the therapeutic records of patients treated by MDT. The study was carried out on a group of 302 patients. The analysis of the symptoms in self-observations of the patient was conducted. The data were compared using various schemes: gender, age range, type of work, classification, positional preferences, and applied directional procedures.
Results:
Patients more commonly indicate the movements that increase symptoms. The individuals treated with the extension DP reported an increase in pain symptoms during sitting, bending, and standing. The majority of patients were classified into the D3 group and treated with an extension-based approach. With increasing age, the number of individuals classified as D1 decreased, while those classified as D5 increased. In the oldest age group, the number of other than extensional therapeutic DP increased.
Conclusions:
Patients are not able to indicate the movements that decrease the symptoms while the movements that increase the symptoms are better recognized. Certified physiotherapists should educate about the centralization phenomenon and directional preference. While extension movements generally lead to a reduction in reported pain symptoms, they are not the only movements that can centralize symptoms and should not be applied without a thorough examination of the patient.
REFERENCES (32)
1.
Ferreira ML, De Luca K, Haile LM, et al. Global, regional, and national burden of low back pain, 1990–2020, its attributable risk factors, and projections to 2050: a systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol 2023; 5: e316-29.
2.
Li Y, Zhang S, Shu P. Global burden of neck pain in 204 countries from 1990–2019. Arch Med Sci 2023; 19: 1811-21.
3.
Sirbu E, Onofrei RR, Szasz S, Susan M. Predictors of disability in patients with chronic low back pain. Arch Med Sci 2023; 19: 94-100.
4.
Long A, May S, Fung T. Specific directional exercises for patients with low back pain: a case series. Physiother Can 2008; 60: 307-17.
5.
Ali Ismail AM, Abd El-Azeim AS, El-Sayed Felaya ESE. Integrated neuromuscular inhibition technique versus spray and stretch technique in neck pain patients with upper trapezius trigger points: a randomized clinical trial. J Man Manip Ther 2024; 32: 141-9.
6.
Ismail AMA. ChatGPT: an expected excellent future technology in enhancing patient care education and physiotherapists’ continuous training. Eur J Physiother 2024; Available from: https://www.tandfonline.com/do....
7.
Edmond SL, Werneke MW, Grigsby D, Young M, Harris G. The association between self-efficacy on function and pain outcomes among patients with chronic low back pain managed using the McKenzie approach: a prospective cohort study. J Man Manip Ther 2023; 31: 38-45.
8.
Will JS, Bury DC, Miller JA. Mechanical low back pain. Am Fam Phys 2018; 98: 421-8.
9.
Edmond SL, Cutrone G, Werneke M, et al. Association between centralization and directional preference and functional and pain outcomes in patients with neck pain. J Orthop Sports Phys Ther 2014; 44: 68-75.
10.
May S, Runge N, Aina A. Centralization and directional preference: an updated systematic review with synthesis of previous evidence. Musculoskelet Sci Pract 2018; 38: 53-62.
11.
Truszczyńska A. Centralisation and peripheralisation of symptoms according to McKenzie Method among patients with chronic low back pain. Fizjoter Pol 2011; 11: 351-6.
12.
Werneke MW, Edmond S, Deutscher D, et al. Effect of adding McKenzie syndrome, centralization, directional preference, and psychosocial classification variables to a risk-adjusted Model predicting functional status outcomes for patients with lumbar impairments. J Orthop Sports Phys Ther 2016; 46: 726-41.
13.
Werneke M, Hart DL. Centralization phenomenon as a prognostic factor for chronic low back pain and disability. Spine 2001; 26: 758-65.
14.
May S. Classification by McKenzie mechanical syndromes: a survey of McKenzie-trained faculty. J Manipulative Physiol Ther 2006; 29: 637-42.
15.
May S, Rosedale R. An international survey of the comprehensiveness of the McKenzie classification system and the proportions of classifications and directional preferences in patients with spinal pain. Musculoskelet Sci Pract 2019; 39: 10-5.
16.
McKenzie R, May S. Lumbar Spine Mechanical Diagnosis and Therapy. Vol. 2. Wyd. Forum, Poznan 2011; 453-820.
17.
Halliday MH, Pappas E, Hancock MJ, et al. A randomized clinical trial comparing the McKenzie method and motor control exercises in people with chronic low back pain and a directional preference: 1-year follow-up. Physiotherapy 2019; 105: 442-5.
18.
Hefford C. McKenzie classification of mechanical spinal pain: Profile of syndromes and directions of preference. Man Ther 2008; 13: 75-81.
19.
Mbada EC, Ayanniyi PO, Ogunlade SO. Pattern of McKenzie syndromes and directional preference in patients with long-term mechanical low-back pain. Roman J Phys Ther 2013; 19: 62-8.
20.
Kondrat A, Huber J, Ziółkowska A, Lipiec J, Kulczyk A, Stengert T. Evaluation of treatment with McKenzie therapy using surface electromyography studies in patients with lumbosacral discopathy - pilot studies. Rehabil.
22.
Nowak K, Witkoś J, Michalik P, Budziosz J, Sieroń K. Assessing the extent of knowledge of patience suffering from low back pain about McKenzie treatment method. Emerg Room 2016; 9: 10-5.
23.
Werneke MW, Hart DL. Centralization: association between repeated end-range pain responses and behavioral signs in patients with acute non-specific low back pain. J Rehabil Med 2005; 37: 286-90.
24.
Mańko M, Zubrzycki J, Karpiński R. The impact of the artificial intervertebral disc on functioning the lumbar spine. J Technol Exp Mechan Engin 2015; 1: 33-58.
25.
Zawadka M, Fijewski A, Gawda P. Low back pain and degenerative changes. Geriatry 2017; 11: 56-65.
26.
Pramesti NP, Wibowo HK, Putri PM. Individual factors influence incidence of low back pain in batik craftsman. Jurnal Keterapian Fisik 2021; 6: 1-10.
27.
Celej-Szuster J, Turowski K, Przychodzka E, Lorencowicz R. Functional ability of patients with lumbar discopathy. Chapter V. Chair and Department of Neurological Nursing, Faculty of Health Sciences, Medical University of Lublin.
28.
Fiałkowski T, Bujok J, Szurmik T, Majerski P. Evaluation of treatment of patients with radicular pain in the lumbosacral part of the spine after periradicular, epidural steroid injection. J Educ Health Sport 2017; 7: 3-14.
29.
Leboeuf-Yde C, Kyvik KO. At what age does low back pain become a common problem? A study of 29,424 individuals aged 12-41 years. Spine 1998; 23: 228-34.
30.
Augustyniuk K, Leśniak A, Szkup M, Rogalska D, Jurczak A. The occurance of spinal pain in trade sector workers. Forum Med Rodz 2016; 10: 95-8.
31.
Klimaszewska K, Krajewska-Kułak E, Kondzior D, Kowalczuk K, Jankowiak B. Quality of life in patients with lumbar spine pain syndromes. Nurs Probl 2011; 19: 47-54.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.