Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
LIPID DISORDERS / CLINICAL RESEARCH
Success in achieving LDL-C target values in a high-risk population in Slovakia: the SlovakLipid retrospective study
1
SLOVACRIN & MEDIPARK, Faculty of Medicine, Pavol Jozef Safarik University, Košice, Slovakia
2
2nd Department of Cardiology, East Slovak Institute of Cardiovascular Diseases and Faculty of Medicine, Pavol Jozef Safarik University, Košice, Slovakia
Submission date: 2023-06-04
Final revision date: 2023-07-30
Acceptance date: 2023-08-11
Online publication date: 2023-09-06
Corresponding author
Stefan Toth
SLOVACRIN & MEDIPARK, Faculty of Medicine, Pavol Jozef Safarik University, Košice, Slovakia
SLOVACRIN & MEDIPARK, Faculty of Medicine, Pavol Jozef Safarik University, Košice, Slovakia
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Slovakia is among the countries with the highest cardiovascular mortality; nevertheless, extensive data on the effectiveness of dyslipidaemia management are lacking. The aim of this study was to assess the implementation of European guidelines in the very high-risk population in Slovakia.
Material and methods:
We retrospectively analysed anonymised low-density lipoprotein-cholesterol (LDL-C) values of patients at very high cardiovascular risk gathered between 2017 and 2019 from a collaborating laboratory with nationwide reach. Cardiovascular risk (CV) risk was based on the patient’s International Classification of Diseases (ICD) diagnosis. LDL-C target values were based on the 2016 ESC/EAS recommendations, as well as current recommendations from 2019. Patients diagnosed with acute coronary syndrome (ACS), stroke, or overall very high-risk cardiovascular disease (CVD) were selected.
Results:
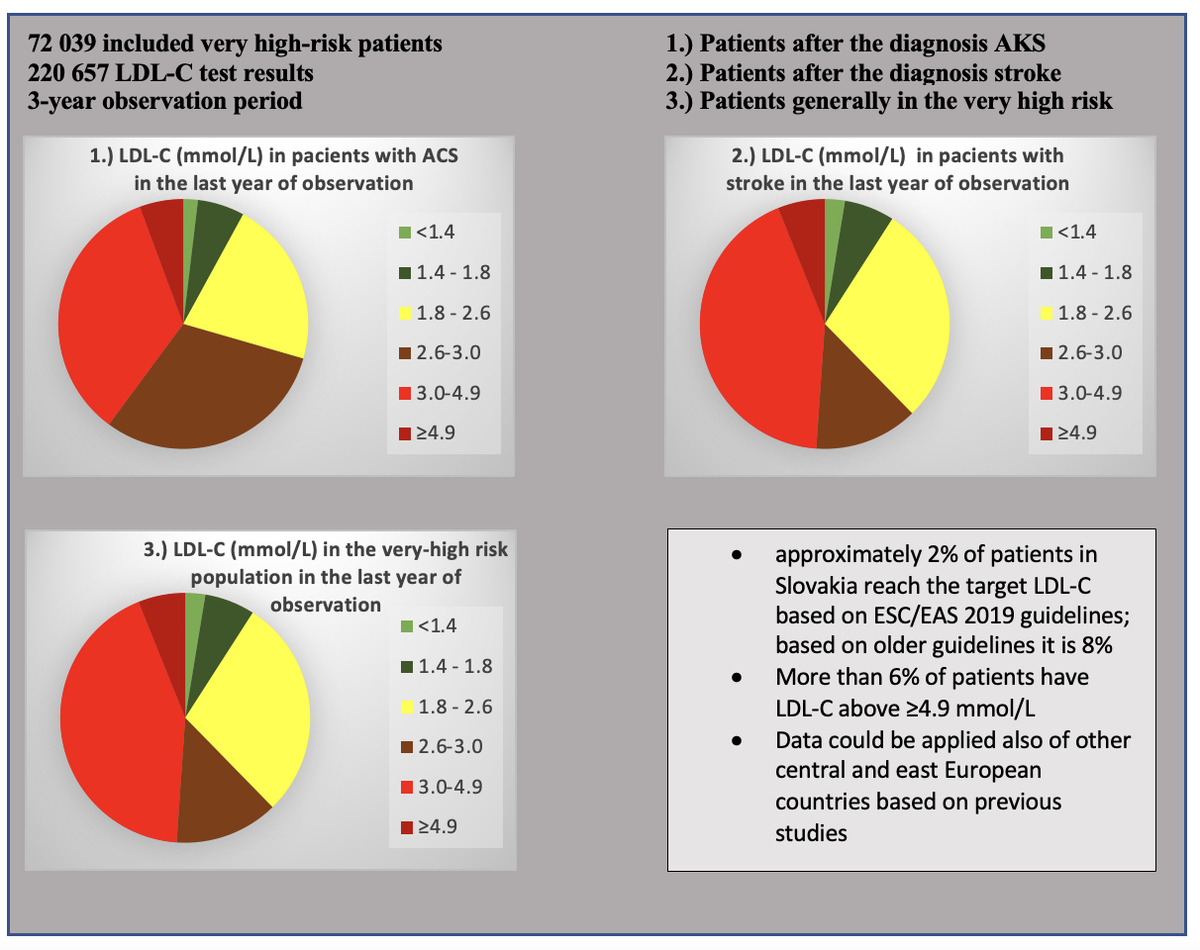
A total of 220 657 LDL-C test results from 72 039 patients were processed. Only 8–9% of patients with ACS attained target LDL-C in a follow-up test each year. 6–9% of patients had LDL-C levels ≥ 4.9 mmol/l. Only 9–10% of patients with stroke achieved target LDL-C levels, and 7–8% had levels ≥ 4.9 mmol/l. In the very high CV risk group, only 7% of patients achieved target levels, and 7–8% had extremely high LDL-C levels ≥ 4.9 mmol/l. With the ESC/EAS 2019 recommendations only 2–3% of patients in each group achieved target levels each year.
Conclusions:
Based on our results, we found that over 90% of patients with very high CVD risk do not achieve target LDL-C levels. This percentage is even higher when implementing the 2019 guidelines. These patients remain at high risk of subsequent CVD events and would benefit significantly from intensified hypolipaemic therapy.
Slovakia is among the countries with the highest cardiovascular mortality; nevertheless, extensive data on the effectiveness of dyslipidaemia management are lacking. The aim of this study was to assess the implementation of European guidelines in the very high-risk population in Slovakia.
Material and methods:
We retrospectively analysed anonymised low-density lipoprotein-cholesterol (LDL-C) values of patients at very high cardiovascular risk gathered between 2017 and 2019 from a collaborating laboratory with nationwide reach. Cardiovascular risk (CV) risk was based on the patient’s International Classification of Diseases (ICD) diagnosis. LDL-C target values were based on the 2016 ESC/EAS recommendations, as well as current recommendations from 2019. Patients diagnosed with acute coronary syndrome (ACS), stroke, or overall very high-risk cardiovascular disease (CVD) were selected.
Results:
A total of 220 657 LDL-C test results from 72 039 patients were processed. Only 8–9% of patients with ACS attained target LDL-C in a follow-up test each year. 6–9% of patients had LDL-C levels ≥ 4.9 mmol/l. Only 9–10% of patients with stroke achieved target LDL-C levels, and 7–8% had levels ≥ 4.9 mmol/l. In the very high CV risk group, only 7% of patients achieved target levels, and 7–8% had extremely high LDL-C levels ≥ 4.9 mmol/l. With the ESC/EAS 2019 recommendations only 2–3% of patients in each group achieved target levels each year.
Conclusions:
Based on our results, we found that over 90% of patients with very high CVD risk do not achieve target LDL-C levels. This percentage is even higher when implementing the 2019 guidelines. These patients remain at high risk of subsequent CVD events and would benefit significantly from intensified hypolipaemic therapy.
REFERENCES (37)
1.
Gitt AK, Lautsch D, Ferrieres J, et al. Cholesterol target value attainment and lipid-lowering therapy in patients with stable or acute coronary heart disease: results from the Dyslipidemia International Study II. Atherosclerosis 2017; 266: 158-66.
2.
Studencan M, Pella D, Bramlage P, Kaszasova E. Clinical characteristics and management of hyperlipoproteinemia in patients with chronic coronary heart disease in Slovakia. Arch Med Sci DOI: https://doi.org/10.5114/aoms/1....
4.
Banach M, Shekoohi N, Mikhailidis DP, Lip GY, Hernandez AV, Mazidi M. Relationship between low-density lipoprotein cholesterol, lipid-lowering agents and risk of stroke: a meta-analysis of observational studies (n = 355,591) and randomized controlled trials (n = 165,988). Arch Med Sci 2022; 18: 912-29.
5.
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J 2020; 41: 111-88.
6.
Ballantyne CM, Raichlen JS, Nicholls SJ, et al. Effect of rosuvastatin therapy on coronary artery stenoses assessed by quantitative coronary angiography: a study to evaluate the effect of rosuvastatin on intravascular ultrasound-derived coronary artery atheroma burden. Circulation 2008; 117: 2458-66.
7.
Nicholls SJ, Puri R, Anderson T, et al. Effect of evolocumab on progression of coronary disease in statin-treated patients: the GLAGOV randomized clinical trial. JAMA 2016; 316: 2373-84.
8.
Kováčová M, Hubáček Mrózová L, Hroncová D. LDL-C cholesterol in patients with dyslipidemia: retrospective analysis of local LDL-C data obtained for 2017-2019, Bratislava: InovaHealth s. r. o., 2021.
9.
Cholesterol Treatment Trialists’ Collaboration, 2015. Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials. Lancet 2015; 385: 1397-405.
10.
Collins R, Reith C, Emberson J, et al. Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet 2016; 388: 2532-61.
11.
Banach M, López-Sendon JL, Averna M, et al. Treatment adherence and effect of concurrent statin intensity on the efficacy and safety of alirocumab in a real-life setting: results from ODYSSEY APPRISE. Arch Med Sci 2022; 18: 285-92.
12.
Banach M, Burchardt P, Chlebus K, et al. PoLA/CFPiP/PCS/PSLD/PSD/PSH guidelines on diagnosis and therapy of lipid disorders in Poland 2021. Arch Med Sci 2021; 17: 1447-547.
13.
Dyrbus K, Gasior M, Desperak P, Nowak J, Osadnik T, Banach M. Characteristics of lipid profile and effectiveness of management of dyslipidaemia in patients with acute coronary syndromes–data from the TERCET registry with 19,287 patients. Pharmacol Res 2019; 139: 460-6.
14.
Silverio A, Benvenga RM, Piscione F, et al. Prevalence and predictors of out-of-target LDL cholesterol 1 to 3 years after myocardial infarction. A subanalysis from the EYESHOT Post-MI Registry. J Cardiovasc Pharmacol Ther 2021; 26: 149-57.
15.
Kotseva K, Wood D, De Backer G, De Bacquer D, Pyörälä K, Keil U; EUROASPIRE Study Group. Cardiovascular prevention guidelines in daily practice: a comparison of EUROASPIRE I, II, and III surveys in eight European countries. Lancet 2009; 373: 929-40.
16.
Kotseva K, Wood D, De Bacquer D, et al. EUROASPIRE IV: A European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur J Prev Cardiol 2016; 23: 636-48.
17.
Gitt AK, Drexel H, Feely J, et al. Persistent lipid abnormalities in statin-treated patients and predictors of LDL-cholesterol goal achievement in clinical practice in Europe and Canada. Eur J Prev Cardiol 2012; 19: 221-30.
18.
Gitt AK, Ferrieres J, de Ferrari G, et al. 0186: Are coronary patients on lipid-lowering therapy in Europe achieving the recommended LDL-C target? Results from the Dyslipidemia International Study (DYSIS) II Europe. Arch Cardiovasc Dis Suppl 2016; 8: 5.
19.
De Backer G, Jankowski P, Kotseva K, et al. Management of dyslipidaemia in patients with coronary heart disease: results from the ESC-EORP EUROASPIRE V survey in 27 countries. Atherosclerosis 2019; 285: 135-46.
20.
Mert GÖ, Başaran Ö, Mert KU, et al. The reasons of poor lipid target attainment for secondary prevention in real life practice: results from EPHESUS. Int J Clin Practice 2019; 73: 1-9.
21.
März W, Dippel FW, Theobald K, Gorcyca K, Iorga ŞR, Ansell D. Utilization of lipid-modifying therapy and low-density lipoprotein cholesterol goal attainment in patients at high and very-high cardiovascular risk: real-world evidence from Germany. Atherosclerosis 2018; 268: 99-107.
22.
Perez de Isla L, Alonso R, Watts GF, et al. Attainment of LDL-cholesterol treatment goals in patients with familial hypercholesterolemia: 5-year SAFEHEART registry follow-up. J Am Coll Cardiol 2016; 67: 1278-85.
23.
Ray KK, Molemans B, Schoonen WM, et al. EU-Wide cross-sectional observation al study of lipid-modifying therapy use in secondary and primary care: the DA VINCI study. Eur J Prev Cardiol 2021; 28: 1279-89.
24.
Bruthans J, Cífková R, Lánská V, et al. Explaining the decline in coronary heart disease mortality in the Czech Republic between 1985 and 2007. Eur J Prev Cardiol 2014; 21: 829-39.
25.
Bandosz P, O’Flaherty M, Drygas W, et al. Decline in mortality from coronary heart disease in Poland after socioeconomic transformation: a modelling study. BMJ 2012; 344: d8136.
26.
Joensen AM, Joergensen T, Lundbye-Christensen S, et al. Explaining trends in coronary heart disease mortality in different socioeconomic groups in Denmark 1991-2007 using the IMPACTSEC model. PLoS One 2018; 13: e0194793.
27.
Psota M, Bandosz P, Goncalvesova E, et al. Explaining the decline in coronary heart disease mortality rates in the Slovak Republic between 1993-2008. PLoS One 2018; 13: e0190090.
28.
Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J 2016; 37: 2999-3058.
29.
Pella D, Pecen L, Műllerová J, et al. Are we successful in achieving target values for LDL cholesterol in statin-treated patients? Results from the DYSIS I survey – Slovak Republic. Int Med 2015.
30.
Cannon CP, Blazing MA, Giugliano RP, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med 2015; 372: 2387-97.
31.
Caprnda M, Hencel J, Farkasovsky J, Encinger PS, Tlčimuka MO. Achieving LDL cholesterol targets with an effective dose of atorvastatin 30 mg in general practitioner practice. Via Pract 2015; 12: 213-6.
32.
Vrablik M, Seifert B, Parkhomenko A, et al. Lipid-lowering therapy use in primary and secondary care in Central and Eastern Europe: DA VINCI observational study. Atherosclerosis 2021; 334: 66-75.
33.
Ray KK, Haq I, Bilitou A, et al. Treatment gaps in the implementation of LDL cholesterol control among high-and very high-risk patients in Europe between 2020 and 2021: the multinational observational SANTORINI study. Lancet Reg Health Eur 2023; 29: 100624.
34.
Banach M, Reiner Z, Cicero AF, et al. 2022: the year in cardiovascular disease–the year of upfront lipid lowering combination therapy. Arch Med Sci 2022; 18: 1429-34.
35.
Lewek J, Niedziela J, Desperak P, et al. Intensive statin therapy versus upfront combination therapy of statin and ezetimibe in acute coronary syndrome patients. A propensity score matching analysis based on the PL-ACS Registry data. A Propensity Score Matching Analysis Based on the PL-ACS Registry Data. J Am heart Assoc 2023; 12: e030414.
36.
Banach M, Penson PE, Vrablik M, et al. Optimal use of lipid-lowering therapy after acute coronary syndromes: A Position Paper endorsed by the International Lipid Expert Panel (ILEP). Pharmacol Res 2021; 166: 105499.
37.
Kim BK, Hong SJ, Lee YJ, et al. Long-term efficacy and safety of moderate-intensity statin with ezetimibe combination therapy versus high-intensity statin monotherapy in patients with atherosclerotic cardiovascular disease (RACING): a randomised, open-label, non-inferiority trial. Lancet 2022; 400: 380-90.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.