Introduction
Pulmonary hypertension (PH) is a progressive disease characterized by elevated pulmonary vascular resistance, which leads to an increased workload in the right ventricle, symptoms of heart failure, and death if not properly treated. The routine clinical evaluation of PH basically comprises an exercise capacity assessment, biomarkers, echocardiography, and right heart catheterization (RHC) [1]. Because of the invasive nature of RHC, it cannot be frequently repeated; thus, non-invasive tests for monitoring disease severity and proper therapeutic decision-making are continuously sought. Recently, biomarkers, such as N-terminal prohormone B-type natriuretic peptide (NT-proBNP) and troponin-T (TnT), have emerged as attractive non-invasive tools for monitoring patients with PH [2–6]. However, given the complexity of PH, it is unlikely that a single biomarker will be appropriate for the assessment of disease severity and patient outcomes. Therefore, searching for new biomarkers has serious clinical significance. The soluble ST2 (sST2) protein is an interleukin (IL)-1 receptor family member that occurs in two isoforms: transmembrane ST2 ligand (ST2L) and soluble ST2 (sST2) [7–9]. Soluble ST2 is a blood-soluble truncated receptor that can be detected in serum. Interleukin 33 is a member of the IL-1 receptor ligand family and the dedicated ligand of ST2L receptor [7–10]. Soluble ST2 is supposed to work as a “decoy” receptor for IL-33, inhibiting the IL-33/ST2L signaling pathway. Interleukin 33 has been shown to exert an anti-hypertrophic effect through binding to ST2L receptors in cardiomyocytes [7–9]. The soluble ST2 protein is released predominantly in response to myocardial stress or strain [11], but it is also known for its involvement in type 2 immune responses [12]. In the last years, sST2 has been used as a novel biomarker of myocardial strain and remodeling mainly among patients with left heart failure. Based on available research, a prognostic value for mortality in chronic and acute heart failure has been revealed [13–15]. Moreover, assessed in settings of acute myocardial infarction, sST2 levels correlate with post-infarct cardiac remodeling [16] and can be predictive of 30-day mortality [17]. The relation of sST2 concentration with right heart failure has not been investigated extensively yet. Previous studies revealed the potential role of sST2 in pulmonary vascular remodeling in patients with idiopathic pulmonary arterial hypertension (iPAH), correlations of sST2 levels with right ventricular dysfunction, as well as prognostic value in cohorts of patients with pulmonary arterial hypertension (PAH) and chronic thromboembolic pulmonary hypertension (CTEPH) [18–20]. The aim of this study was to assess the role of sST2, an emerging biomarker of heart failure, in a variety of patients with right ventricular overload due to PH of different etiologies.
Material and methods
The study was performed at the European Health Centre in the Department of Pulmonary Circulation, Thromboembolic Disease and Cardiology, Centre of Postgraduate Education Medical in Otwock, Poland, in association with the 1st Chair and Department of Cardiology, Medical University of Warsaw, Poland.
Between September 2016 and August 2017, 100 patients with iPAH or CTEPH were prospectively enrolled in the study. The diagnosis of iPAH or CTEPH was established according to the European Society of Cardiology (ESC) Guidelines [1]. Patients with at least one of the following criteria were excluded: PH of a type other than iPAH or CTEPH, left heart diseases, connective tissue diseases, chronic respiratory diseases, diabetes mellitus, and other diseases caused by inflammatory processes. Relevant left heart disease was ruled out by echocardiography, which was performed in the screening phase. In addition, patients with exacerbated PH were excluded and all participants were stable. Subpopulation of patients with exacerbated disease were defined by clinical features such as sudden deterioration in functional parameters to worse World Health Organization functional class (WHO-FC), signs of right heart failure decompensation, such as ascites or peripheral edema, requiring escalation of diuretic treatment and/or the use of catecholamines as well as any changes in targeted medical therapy of PH within the last 4 weeks. Additionally, in patient with CTEPH treated with balloon pulmonary angioplasty, we did not perform sST2 concentration assessment during the perioperative period, defined as 2 weeks after each session. As stable we defined patients without any deterioration of exercise tolerance, with no need to escalate diuretic treatment or to change targeted therapy of PH in the last 4 weeks. The patients were admitted for routine hospitalization and were evaluated for WHO FC, 6-minute walking test (6MWT), NT-proBNP, and TnT. All patients underwent RHC according to current guidelines [21]. A Swan-Ganz catheter was used to measure the right atrial pressure (RAP), right ventricular pressure (RVP), pulmonary artery pressure (PAP), pulmonary capillary wedge pressure (PCWP), cardiac output (CO) assessed with thermodilution, cardiac index (CI), stroke volume (SV), pulmonary vascular resistance (PVR), and systemic vascular resistance (SVR). The heart rate (HR), systolic arterial pressure (SAP), diastolic arterial pressure (DAP), O2 saturation of mixed venous blood (MVSatO2) samples and O2 saturation of arterial blood (AoSatO2) were also assessed during the RHC procedure. All the laboratory tests, including NT-proBNP and TnT assessment, as well as blood collection for sST2 assessment, were performed on the same day. Other procedures, such as RHC and 6MWT, were performed the next day after laboratory tests had been performed. The blood samples for sST2 evaluation were obtained directly from the peripheral vein. EDTA anticoagulated blood samples were collected and plasma aliquots were frozen at –80°C until further analysis. All the sST2 concentration measurements were performed after 2 months from the date of blood collection. The sST2 concentration was measured in frozen samples using the ASPECT-PLUS sST2 test (Critical Diagnostics, San Diego, CA, USA), a rapid lateral flow immunoassay for the quantitative measurement of sST2 in human plasma using the ASPECT reader. The ASPECT-PLUS ST2 test cassette consists of murine mouse monoclonal antibodies against human sST2, goat polyclonal antibodies against murine IgG, and a fluorescent dye. The ASPECT Reader measures the fluorescence signal, and quantitative sST2 values are given as nanograms per milliliter. The plasma sST2 concentration was assessed in accordance with the manufacturer’s manual. Based on the measurement limits of the ASPECT Reader, an sST2 plasma concentration < 12.5 ng/ml or > 250 ng/ml was reported as being below or above the limit values, respectively. According to the manufacturer’s manual, the analysis procedure meets the permissible criteria for analytical parameters, with an average coefficient of variation (CV) of 10.4% for the variation within the assay and 13.6% for the variation among assays.
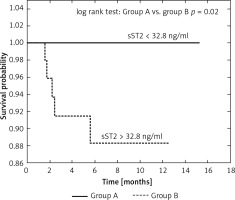
The whole population underwent the follow-up. During the follow-up period (median: 7.67 months, IQR: 3.3–10.77) patients were under the care of our center. The endpoint was all-cause death. The population was divided into two subpopulations: one characterized by a sST2 plasma concentration below the median (group A) and the second by a sST2 plasma concentration above the median (group B). The cumulative survival was compared between the two subpopulations.
According to current guidelines [1] all patients with iPAH received the targeted therapy with: sildenafil, endothelin receptor antagonist (ERA) or prostanoids, during the follow-up period. Eight (19%) patients received dual-targeted therapy. There were no changes in the targeted treatment therapy during the follow-up. 36 (63%) patients diagnosed with CTEPH received targeted therapy (sildenafil of riociguat). Additionally 29 (51%) patients were treated with balloon pulmonary angioplasty (BPA) during the follow-up. No pulmonary endarterectomy was performed within the CTEPH study population.
Statistical analysis
Nominal variables are presented as numbers and percentages. Continuous variables with normal distribution are presented as means and standard derivations (SDs). Variables with distribution different from a normal distribution are presented as medians with 25th and 75th percentile values, i.e., IQR. Groups were compared by paired Student’s t test or the paired Wilcoxon test when appropriate. Spearman correlation was used to test for an association between sST2 and hemodynamic, biochemical, and functional variables. The proportion of patients surviving was estimated by the Kaplan-Meier method with the date of the sST2 blood concentration measurement as the starting point. The survival difference between groups A and B was compared using log-rank. A p-value <0.05 was considered significant. All statistical analyses were performed using Statistica 13.1 (STATSOFT, Tulsa, OK, USA).
Results
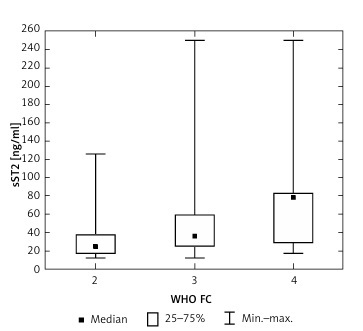
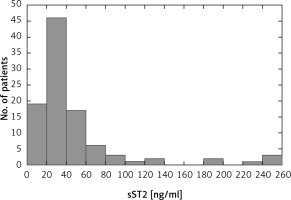
One hundred patients were included in the study (65 females, 35 males, median age: 59.7 ±18.0 years). Thirty-three (33%) patients presented with symptoms of WHO FC II, 59 (59%) patients WHO FC III, and 8 (8%) WHO FC IV. CTEPH was diagnosed in 57 (57%) patients, and 43 (43%) patients suffered from iPAH. The baseline characteristics of the study population are summarized in Table I. The hemodynamic assessment revealed increased mean pulmonary artery pressure (mPAP) (43.0 ±12.3 mm Hg) and increased PVR (6.95 ±3.87 Wood units), normal CI (2.70 ±0.69 l/min × m2), and border values of RAP (6.0 ±4.4 mm Hg). The mean 6MWT distance was decreased (365 ±103 m). The NT-proBNP concentration was increased (median 529 pg/ml [IQR: 234–1889 pg/ml]). In the study population, the median sST2 concentration was 32.8 ng/ml [IQR: 21.6–48.5 ng/ml]. Figure 1 is a histogram of sST2 concentration in the general study population.
Table I
Baseline characteristics of the study population
[i] PH – pulmonary hypertension, iPAH – idiopathic pulmonary arterial hypertension, CTEPH – chronic thromboembolic pulmonary hypertension, WHO FC – World Health Organization functional class, mRAP – mean right atrial pressure, mPAP – mean pulmonary artery pressure, PCWP – pulmonary capillary wedge pressure, CI – cardiac index, PVR – pulmonary vascular resistance, MVsatO2 – mixed venous oxygen saturation, AOsatO2 – aortic oxygen saturation, NT-proBNP – N-terminal prohormone B-type natriuretic peptide, TnT – troponin T, 6MWT – 6-minute walking test.
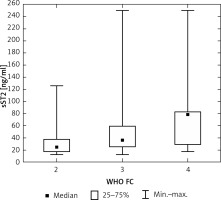
We found no significant differences in the median sST2 concentration according to sex (median sST2 concentration in females and males was 29.1 [IQR: 20.6–42.3 ng/ml] and 39.8 [IQR: 25.2–58.1 ng/ml], respectively; p = 0.103) and the etiology of PH (median sST2 concentration in patients with CTEPH was 34.0 [IQR: 22.2–48.4] ng/ml, and in patients with iPAH 29.4 [IQR: 21.4–52.0] ng/ml, p = 0.94). The median sST2 concentration in patients characterized by FC II was 25.139 ng/ml [IQR: 17.28–37.41 ng/ml], FC III 36.626 ng/ml [IQR: 25.34–58.85 ng/ml], and FC IV 78.579 ng/ml [IQR: 29.19–83.19 ng/ml]. Significant differences were found between the median sST2 according to WHO FC (FC II vs. FC III p = 0.002; FC III vs. FC IV p = 0.12; FC II vs. FC IV p = 0.008). Figure 2 presents the sST2 concentration in certain WHO FCs in the general study population.
Figure 2
Median soluble ST2 (sST2) concentration in particular WHO functional classes in the study population
In the general study population, we found significant hemodynamic correlations between sST2 concentration and mean right atrial pressure (mRAP) (r = 0.562; p < 0.05), mPAP (r = 0.252; p < 0.05), CI (r = – 0.404; p < 0.05), PVR (r = 0.410; p < 0.05), and MVsat02 (r = –0.392; p < 0.05). The assessment of functional capacity and biochemical parameters of heart overload revealed a significant correlation between sST2 and WHO FC (r = 0.355; p < 0.05), as well as NT-proBNP (r = 0.550; p < 0.05) and TnT (r = 0.436; p < 0.05). In addition, a significant negative correlation between sST2 and 6MWT (r = –0.422; p < 0.05) was observed. However, we found no significant correlations between plasma sST2 concentration and age (r = –0.037, p > 0.05) or body mass index (r = 0.103, p > 0.05). In patients with iPAH, sST2 strongly and significantly correlated with NT-proBNP (r = 0.725; p < 0.05) and TnT (r = 0.635; p < 0.05), whereas in patients with CTEPH this correlation was not significant. Correlations between sST2 and hemodynamic parameters were materially stronger in the subgroup of patients with iPAH, but a significant correlation between sST2 and mPAP was found (r = 0.134; p < 0.05) only in patients with CTEPH. Table II presents the correlations between sST2 and functional, biochemical, and hemodynamic parameters in the general study population and both subgroups.
Table II
Clinical and hemodynamic correlations with soluble ST2
| Variable | PH population (r value) | iPAH (r value) | CTEPH (r value) |
|---|---|---|---|
| mRAP [mm Hg] | 0.562* | 0.666* | 0.425* |
| mPAP [mm Hg] | 0.252* | 0.134 | 0.479* |
| PCWP [mm Hg] | 0.073 | –0.011 | 0.229 |
| CI [l/min × m2] | –0.404* | –0.478* | –0.334* |
| CO | –0.370* | –0.420* | –0.306* |
| PVR [Wood units] | 0.410* | 0.383* | 0.456* |
| MVsatO2 (%) | –0.392* | –0.578* | –0.192 |
| AOsatO2 (%) | –0.132 | –0.106 | –0.131 |
| HR | 0.220 | 0.372* | 0.125 |
| NT-proBNP [pg/ml] | 0.550* | 0.725* | 0.248 |
| TnT [ng/ml] | 0.436* | 0.635* | 0.171 |
| 6MWT [m] | –0.422* | –0.487* | –0.335* |
| WHO class | 0.355* | 0.393* | 0.299* |
| Weight [kg] | –0.024 | –0.0143 | 0.030 |
| Height [m] | 0.010 | 0.094 | –0.082 |
| BMI [kg/m2] | 0.103 | 0.147 | 0.159 |
| Age [years] | –0.037 | 0.019 | –0.083 |
* P < 0.05. PH – pulmonary hypertension, iPAH – idiopathic pulmonary arterial hypertension, CTEPH – chronic thromboembolic pulmonary hypertension, mRAP – mean right atrial pressure, mPAP – mean pulmonary artery pressure, PCWP – pulmonary capillary wedge pressure, CI – cardiac index, PVR – pulmonary vascular resistance, MVsatO2 – mixed venous oxygen saturation, AOsatO2 – aortic oxygen saturation, NT-proBNP – N-terminal prohormone B-type natriuretic peptide, TnT – troponin T, 6MWT – 6-minute walking test.
A total of 5 (5%) patients died during the observation period (median: 7.67 months, IQR: 3.3–10.77 months). One patient (M, 69-year-old, CTEPH) died because of pneumonia, 2 patients (F, 72-year-old, iPAH; M, 61-year-old, iPAH) died because of end-stage heart failure. One death (F, 20-year-old, CTEPH) was sudden, presumed cardiac, and 1 patient (F, 53-year-old, iPAH) died because of a neurological event. All the patients who died had the sST2 concentration above the median (32.8 ng/ml). Thus, a ST2 concentration above the median was associated with worse clinical prognosis (Figure 3). We found a significant difference between group A and B regarding survival (p = 0.02 by log-rank test). Table III presents characteristics of patients with sST2 concentration below the median (group A) and above the median (group B).
Table III
Characteristics of patients with soluble ST2 (sST2) concentration below (group A) and above (group B) the median. Data are presented as n (%), mean ± SD, or median [IQR]
[i] WHO FC – World Health Organization functional class, mRAP – mean right atrial pressure, mPAP – mean pulmonary artery pressure, PCWP – pulmonary capillary wedge pressure, CI – cardiac index, PVR – pulmonary vascular resistance, MVsatO2 – mixed venous oxygen saturation, AOsatO2 – aortic oxygen saturation, NT-proBNP – N-terminal pro-brain natriuretic peptide, TnT – troponin T, 6MWT – 6-minute walking test.
Discussion
This is one of the very first studies to characterize the utility of soluble ST2 concentration for the assessment of disease severity and patient outcomes in two types of PH, in addition to well-established and widely used biomarkers. Previous studies have evaluated numerous biomarkers in cohorts of patients with PH of different etiologies, but a specific biomarker with additional prognostic value is still not well defined. There are still only limited data regarding sST2 levels in PH of different etiologies. Soluble ST2 is a part of IL-33/ST2 ligand interaction, which is supposed to form a cardioprotective system, and is upregulated in response to myocardial injury or stress in cardiomyocytes and fibroblasts [11]. One of the main and most common problems for all forms of PH, regardless of etiology, is right heart overload. This appears to be a major factor stimulating the release of sST2. However, it should be remembered that in PAH and CTEPH, cytokines and interleukins have great significance in the pathophysiology of these conditions [22, 23]. The reason for assessment of the sST2 level in patients in CTEPH and IPAH was to investigate if there exist any differences in sST2 concentration in the context of different mechanisms underlying the two diseases.
There are currently several methods for evaluating sST2 concentration in human plasma. The quantitative lateral flow test for rapid sST2 concentration measurement – the ASPECT-PLUS ST2 test – was successfully applied in our study. Pursuant to the manufacturer’s manual, in healthy volunteers, the interquartile values of ST2 were between 15 and 25 ng/ml, whereas the concentration of 35 ng/ml falls between the 90th and 95th centiles of the healthy population [24]. In patients diagnosed with heart failure with sST2 protein concentrations ≥ 35 ng/ml, the risk of adverse events (hospitalization or death in 1 year) has been reported to be higher than in patients with ST2 protein concentrations below this value [17, 24–26]. Dieplinger et al. evaluated the ASPECT-PLUS ST2 test and performed an assay comparison with the MBL ST2 test and PRESAGE ST2 ELISA in a cohort of patients with acute dyspnea. At the sST2 level cut-off of 35 ng/ml, proposed in previous studies, the sST2 results obtained with the ASPECT-PLUS ST2 test were similar to those obtained with the MBL ST2 test as well as with the PRESAGE ST2 ELISA assay [27]. In our study median sST2 values in CTEPH and iPAH patients were close to the cut-off for risk stratification of patients with heart failure (i.e., 35 ng/ml) [25].
Several studies have been performed previously in order to assess the reference values of sST2 concentration in a healthy population. Lu et al. established the gender-specific reference values using 245 female and male serum samples from the United States population. The sST2 concentration was significantly higher in males than in females (24.9 vs. 16.9 ng/ml; p < 0.0001), but there was no correlation of sST2 concentration with age in either gender (r = –0.07; p = 0.14). More precisely, the reference intervals for sST2 levels were evaluated to be 8.6–49.3 for males and 7.2–33.5 ng/ml for females [24]. These values were similar to those obtained from Framingham Heart Study participants [28], but substantially higher in comparison to those assessed by Dieplinger et al. [29]. Notably, in the healthy cohort from the Framingham Heart Study, the strongest correlations of sST2 were found with age and sex. There is some inconsistency regarding correlation of sST2 with age and sex in the data available. Coglianese et al. hypothesized that this trend may reflect the effects of sex hormones on sST2 concentration: in their study women on hormone replacement therapy (estrogen without progestin) had the lowest concentration of sST2 [28]. Dieplinger et al. revealed significant gender-dependent, but not age-related, differences in sST2 concentration [29]. To sum up, there are still no consistent results in the available literature. However, it should be emphasized that cofactors influencing other biomarker concentrations, such as renal function or body mass index (BMI), did not significantly correlate with sST2 levels [28]. In our study we found no significant correlations with age or BMI as well as no significant differences in sST2 concentration according to gender status. Further studies are needed to investigate these specific discrepancies.
There is growing evidence that the sST2 concentration could be useful in monitoring disease severity and provides information about prognosis in patients suffering from cardiovascular diseases with additive value to well-established biomarkers, such as natriuretic peptides and cardiac troponins [30–32]. In 2003, Weinberg et al. announced that sST2 is an emerging biomarker in patients with heart failure [33]. Since then, numerous researchers have suggested that sST2 seems to be a useful biomarker with additive prognostic value to natriuretic peptide of both acute and chronic heart failure as well as in ST-elevation myocardial infarction patient cohorts [13–15, 34, 35]. Thus, according to the 2017 American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines sST2 has great additional clinical value in risk stratification of patients with chronic and acute heart failure [36].
However, the importance of sST2 concentration in the population of patients with right heart failure due to PH still remains unclear. Previously, the association between sST2 concentration and right ventricular systolic pressure was reported by Shah et al. [37]. In addition, Carlomango et al. reported increased sST2 concentration in patients with PAH, with the suggestion that the increase of sST2 concentration was closely related to right ventricular dilatation and systolic dysfunction. However, it is worth mentioning that only 25 patients with PAH of various etiologies and 10 in the control group were enrolled in their study [18]. The sST2 concentration was significantly higher in patients suffering from PAH compared to the control group. Furthermore, sST2 correlations with parameters of right ventricle remodeling assessed with cardiac magnetic resonance (CMR), and with functional as well as biochemical parameters, such as 6MWT distance and NT-proBNP, were noted [18]. Zheng et al. enrolled in their study 40 idiopathic PAH patients and 24 healthy controls. Their results revealed elevated sST2 concentration in patients with PAH compared to the control group. Pearson correlation analysis revealed a significant correlation between sST2 and CI, mean RAP, mixed venous oxygen saturation and arterial oxygen saturation [38]. The correlations obtained in our study seem to be stronger than those obtained by Zheng. In 2019 Geenen et al. investigated sST2 concentration in 104 patients with PH of various etiologies. Median sST2 concentration in their study was similar to that obtained in our study (34.5 ng/ml vs. 32.8 ng/ml). The results revealed significant correlation of sST2 levels and hemodynamic parameters, 6MWT, functional class and NT-proBNP [19]. Our results also revealed significant correlations with hemodynamic parameters, NT-proBNP, TnT, and functional capacity. Moreover, our results reflect the strong pathophysiological basis observed in previous research concerning the role of sST2 concentration in patients with right heart overload due to PH. Notably, in contrast to the results obtained by Geenen et al., in our study sST2 concentration did not differ significantly between PH subgroups. There can be several reasons for our results. Firstly, the number of patients enrolled in our study was relatively small and it could be insufficient to reveal statistically significant differences between PH subgroups. Secondly, the similar sST2 concentrations between PH subgroups in our study could be due to similar hemodynamic parameters (such as mPAP and PVR), and hence a similar degree of right ventricular overload in both groups. Thus, it could also be the proof that there is only a small share of endothelium as the source of sST2 [20], because differences in the endothelium remodeling lie at the basis of pathophysiological differences between those two types of PH. However, much could be speculated about the significant differences in sST2 levels and correlations between particular types of PH, observed in previous studies. The role of sST2 in PH may be associated with its role in fibrosis of cardiac muscle in response to increased pulmonary vascular resistance induced by PH, but the relationship between sST2 concentration and the pulmonary vascular bed has not been investigated thoroughly [18, 37]. We hypothesize that the differences in sST2 concentration between particular PH subgroups, observed in previous studies, may result from endothelial dysfunction and different pathological changes occurring in the vessels in the course of CTEPH and iPAH. Additionally, cytokines seem to contribute to the pathogenesis of PH; thus it has been proposed that the pathway of the IL33/ST2 receptor could be included in the PAH development [20, 22]. Interestingly, Willems et al. revealed that the sST2 concentration significantly increased 24 h after patients underwent peripheral vascular surgery, arterial bypass or femoral endarterectomy [39]. Obtained results suggest that sST2 may be related to arterial injury. In addition, Pascual-Figal et al. reported that the lungs demonstrate upregulation of sST2 mRNA. The authors also identified an association between increased alveolus thickness and upregulation of sST2, indicating the degree of pulmonary congestion and ST2 production. Thus, sST2 level may be influenced by dynamic contributions of the lungs and vascular endothelium [40]. This may suggest that sST2, rather than being limited to cardiac remodeling only, may reflect the broad condition of the heart, lung and pulmonary vascular bed system [40, 41]. As a result, sST2 may be considered as a comprehensive and useful biomarker in addition to other widely used biomarkers, secreted predominantly from ventricular tissues, in the diagnostic process, monitoring disease severity and risk stratification in patients with PH [42]. Further studies with larger cohorts are needed to investigate this process; however, it seems that a combination of multiple biomarkers may be beneficial in guiding PH diagnosis and therapy.
This study has several limitations. First, the number of subjects was relatively low. Only iPAH and CTEPH patients were enrolled, and other types of PH were excluded. Second, the prognostic value of sST2 was established only according to death. Finally, we did not use the FDA-approved ELISA format, but we tried to evaluate the ASPECT-PLUS ST2 test, a rapid quantitative lateral flow for measurement of sST2 in human plasma, which has not yet been approved by the FDA.
In conclusion, the results suggested that sST2 could be a promising biomarker of right ventricular failure in patients with precapillary PH, alongside already well-established and widely used biomarkers such as NT-proBNP and troponin T. The sST2 protein correlates with myocardial strain and injury markers of heart failure, as well as invasive hemodynamic parameters of PH. Moreover, sST2 seems to be a marker of poor clinical prognosis in patients with pulmonary hypertension, but further studies are needed to evaluate its prognostic value.