Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CLINICAL RESEARCH
Sleep disorders and renal failure: exploring the role of creatinine and sleep apnea syndrome through cross-sectional studies and Mendelian randomization analysis
1
Department of Pediatrics,Affiliated Hospital of Inner Mongolia Medical University, Hohhot, Inner Mongolia Autonomous Region, China
2
Department of Pathophysiology, School of Basic Medicine, Inner Mongolia Medical University, Hohhot, Inner Mongolia Autonomous Region, China
3
Department of Urology, The First Hospital of Jilin University, Changchun, Jilin, China
4
Department of Plastic and Aesthetic Surgery, The First Hospital of Jilin University, Changchun, Jilin, China
5
Gastric and Colorectal Surgery Department, The First Hospital of Jilin University, Changchun, Jilin, China
These authors had equal contribution to this work
Submission date: 2024-09-03
Final revision date: 2024-12-11
Acceptance date: 2024-12-25
Online publication date: 2025-03-04
Corresponding author
Lei Hao
Assoc. Prof. Department of Pathophysiology Inner Mongolia Medical University No. 1 North Passage Road Hohhot City Inner Mongolia Autonomous Region China, 010107
Assoc. Prof. Department of Pathophysiology Inner Mongolia Medical University No. 1 North Passage Road Hohhot City Inner Mongolia Autonomous Region China, 010107
Peng Li
Assoc. Prof., Department of Pediatrics Affiliated Hospital of Inner Mongolia Medical University No. 1 North Passage Road Hohhot City Inner Mongolia Autonomous Region China, 010107.
Assoc. Prof., Department of Pediatrics Affiliated Hospital of Inner Mongolia Medical University No. 1 North Passage Road Hohhot City Inner Mongolia Autonomous Region China, 010107.
Article (PDF)
Supplementary files
References (48)
Sleep disorders - supplementary figs.pdf
Sleep disorders - Supplementary Table SI.XLSX
Sleep disorders - Supplementary Table SII.XLS
Sleep disorders - Supplementary Table SIII.XLSX
Sleep disorders - Supplementary Table SIV.XLSX
Sleep disorders - Supplementary Table SIX.XLSX
Sleep disorders - Supplementary Table SV.XLSX
Sleep disorders - Supplementary Table SVI.XLSX
Sleep disorders - Supplementary Table SVII.XLSX
Sleep disorders - Supplementary Table SVIII.XLSX
Sleep disorders - Supplementary Table SX.XLSX
Sleep disorders - Supplementary Table SXI.XLSX
Sleep disorders - Supplementary Table SXII.XLSX
Sleep disorders - Supplementary Table SXIII.XLSX
KEYWORDS
sleep disorderrenal failurecreatinineMendelian randomizationNational Health and Nutrition Examination Survey
TOPICS
Family MedicineGeneticsInternal Medicine and GeriatricsNephrologyPsychologyPublic HealthUrologyNeonatologyEpidemiology
ABSTRACT
Introduction:
The aim of the study was to explore potential factors affecting the emergence of sleep disorders in patients with renal failure.
Material and methods:
A cross-sectional study approach was employed in order to evaluate the relationship between renal failure and sleep disorders, and to validate the findings through Mendelian randomization (MR) analysis. Furthermore, we utilized a two-stage MR methodology to quantify the specific contribution of creatinine, mediated by sleep apnea syndrome, to the development of renal failure.
Results:
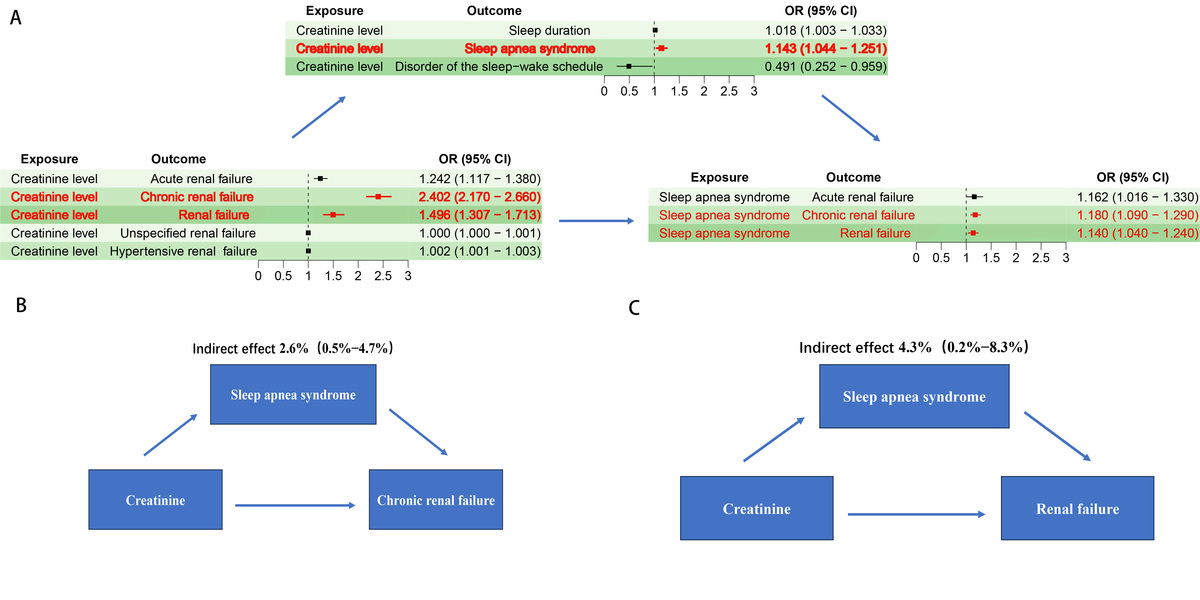
In the multivariate adjusted logistic regression analysis, compared to non-renal failure patients, time to fall asleep in minutes (OR = 0.01, 95% CI: 0.00–0.40, p = 0.022) was significantly reduced, while waking up during the night (OR = 0.73, 95% CI: 0.62–0.86, p = 0.003), feeling unrested during the day (OR = 0.65, 95% CI: 0.48–0.89, p = 0.015), and feeling overly sleepy during the day (OR = 0.67, 95% CI: 0.50–0.89, p = 0.014) were also decreased. In the study of sleep-related factors and renal failure, it was found that sleep apnea syndrome could serve as a mediating factor in mediating creatinine levels for the occurrence of chronic kidney failure (proportion mediated: 2.6%; 95% CI = 0.5–4.7%) and renal failure (proportion mediated: 4.3%; 95% CI = 0.2–8.3%).
Conclusions:
Compared to non-renal failure patients, patients with renal failure exhibit significantly reduced sleep onset time and sleep stability. Sleep apnea syndrome may act as a mediator, promoting creatinine-induced damage to the kidneys.
The aim of the study was to explore potential factors affecting the emergence of sleep disorders in patients with renal failure.
Material and methods:
A cross-sectional study approach was employed in order to evaluate the relationship between renal failure and sleep disorders, and to validate the findings through Mendelian randomization (MR) analysis. Furthermore, we utilized a two-stage MR methodology to quantify the specific contribution of creatinine, mediated by sleep apnea syndrome, to the development of renal failure.
Results:
In the multivariate adjusted logistic regression analysis, compared to non-renal failure patients, time to fall asleep in minutes (OR = 0.01, 95% CI: 0.00–0.40, p = 0.022) was significantly reduced, while waking up during the night (OR = 0.73, 95% CI: 0.62–0.86, p = 0.003), feeling unrested during the day (OR = 0.65, 95% CI: 0.48–0.89, p = 0.015), and feeling overly sleepy during the day (OR = 0.67, 95% CI: 0.50–0.89, p = 0.014) were also decreased. In the study of sleep-related factors and renal failure, it was found that sleep apnea syndrome could serve as a mediating factor in mediating creatinine levels for the occurrence of chronic kidney failure (proportion mediated: 2.6%; 95% CI = 0.5–4.7%) and renal failure (proportion mediated: 4.3%; 95% CI = 0.2–8.3%).
Conclusions:
Compared to non-renal failure patients, patients with renal failure exhibit significantly reduced sleep onset time and sleep stability. Sleep apnea syndrome may act as a mediator, promoting creatinine-induced damage to the kidneys.
REFERENCES (48)
1.
Kovesdy CP. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl 2022; 12: 7-11.
2.
Ruiz-Ortega M, Rayego-Mateos S, Lamas S, et al. Targeting the progression of chronic kidney disease. Nat Rev Nephrol 2020; 16: 269-88.
3.
Wang L, Xu X, Zhang M, et al. Prevalence of chronic kidney disease in China: results from the sixth china chronic disease and risk factor surveillance. JAMA Intern Med 2023; 183: 298-310.
4.
Chen J, Ricardo AC, Reid KJ, et al. Sleep, cardiovascular risk factors, and kidney function: the Multi-Ethnic Study of Atherosclerosis (MESA). Sleep Health 2022; 8: 648-53.
5.
Ricardo AC, Knutson K, Chen J, et al. The association of sleep duration and quality with CKD progression. J Am Soc Nephrol 2017; 28: 3708-15.
6.
Beecroft J, Duffin J, Pierratos A, et al. Enhanced chemo-responsiveness in patients with sleep apnoea and end-stage renal disease. Eur Respir J 2006; 28: 151-8.
7.
Cachia D, Swearer J, Ferguson W, Moonis M. Selective cognitive patterns resulting from bilateral hippocampal ischemia. Arch Med Sci 2011; 7: 168-72.
8.
Sakellaropoulou AV, Hatzistilianou MN, Emporiadou MN, et al. Association between primary nocturnal enuresis and habitual snoring in children with obstructive sleep apnoea-hypopnoea syndrome. Arch Med Sci 2012; 8: 521-7.
9.
Braam B, Lai CF, Abinader J, Bello AK. Extracellular fluid volume expansion, arterial stiffness and uncontrolled hypertension in patients with chronic kidney disease. Nephrol Dial Transplant 2020; 35: 1393-8.
10.
Zoccali C, Roumeliotis S, Mallamaci F. Sleep apnea as a cardiorenal risk factor in CKD and renal transplant patients. Blood Purif 2021; 50: 642-8.
11.
Tan LH, Chen PS, Chiang HY, et al. Insomnia and poor sleep in CKD: a systematic review and meta-analysis. Kidney Med 2022. 4: 100458.
12.
Hanly P. Sleep disorders and end-stage renal disease. Curr Opin Pulm Med 2008; 14: 543-50.
13.
Perl J, Unruh ML, Chan CT. Sleep disorders in end-stage renal disease: ‘Markers of inadequate dialysis’? Kidney Int 2006; 70: 1687-93.
14.
Kalantar-Zadeh K, Lockwood MB, Rhee CM, et al. Patient-centred approaches for the management of unpleasant symptoms in kidney disease. Nat Rev Nephrol 2022; 18: 185-98.
15.
Viggiano D, Wagner CA, Martino G, et al. Mechanisms of cognitive dysfunction in CKD. Nat Rev Nephrol 2020; 16: 452-69.
16.
Jacobi J. The pathophysiology of sepsis – 2021 update: Part 2, organ dysfunction and assessment. Am J Health Syst Pharm 2022; 79: 424-36.
17.
de Boer IH, Rue TC, Hall YN, et al. Temporal trends in the prevalence of diabetic kidney disease in the United States. JAMA 2011; 305: 2532-9.
18.
Ahluwalia N, Dwyer J, Terry A, et al. Update on NHANES dietary data: focus on collection, release, analytical considerations, and uses to inform public policy. Adv Nutr 2016; 7: 121-34.
19.
Ruhl CE, Menke A, Cowie CC, Everhart JE. Relationship of hepatitis C virus infection with diabetes in the U.S. population. Hepatology 2014; 60: 1139-49.
20.
Ismail AMA, Saad AE, Abd-Elrahman NA, Elfahl AMA. Effect of Benson’s relaxation therapy alone or combined with aerobic exercise on cortisol, sleeping quality, estrogen, and severity of dyspeptic symptoms in perimenopausal women with functional dyspepsia. Eur Rev Med Pharmacol Sci 2022; 26: 8342-50.
21.
Yuan Y, Tan W, Huang Y, et al. Association between hysterectomy and kidney stone disease: results from the National Health and Nutrition Examination Survey 2007-2018 and Mendelian randomization analysis. World J Urol 2023; 41: 2133-9.
22.
Burgess S, Thompson SG. Avoiding bias from weak instruments in Mendelian randomization studies. Int J Epidemiol 2011; 40: 755-64.
23.
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol 2013; 37: 658-65.
24.
Liu M, Heizhati M, Li N, et al. The relationship between obstructive sleep apnea and risk of renal impairment in patients with hypertension, a longitudinal study. Sleep Med 2023; 109: 18-24.
25.
Ismail A. Stress axis response to aerobic exercise in chronic obstructive pulmonary disease patients. Adv Rehabil 2022; 36: 24-32.
26.
Lee JJ, Sundar KM. Evaluation and management of adults with obstructive sleep apnea syndrome. Lung 2021; 199: 87-101.
27.
Fazlıoğlu N, Uysal P, Durmus S, et al. Significance of plasma irisin, adiponectin, and retinol binding protein-4 levels as biomarkers for obstructive sleep apnea syndrome severity. Biomolecules 2023; 13: 1440.
28.
Lv R, Liu X, Zhang Y, et al. Pathophysiological mechanisms and therapeutic approaches in obstructive sleep apnea syndrome. Signal Transduct Target Ther 2023; 8: 218.
29.
Hui L, Benca R. The bidirectional relationship between obstructive sleep apnea and chronic kidney disease J Stroke Cerebrovasc Dis 2021; 30: 105652
30.
Prabu P, Acree L, Waller JL, et al. Sleep apnea in end-stage renal disease patients: risk factors and mortality. J Investig Med 2023; 71: 465-70.
31.
Harmon RR, De Lima JJG, Drager LF, et al. Obstructive sleep apnea is associated with interdialytic weight gain and increased long-term cardiovascular events in hemodialysis patients. Sleep Breath 2018; 22: 721-8.
32.
Ogna A, Ogna VF, Mihalache A, et al. Obstructive sleep apnea severity and overnight body fluid shift before and after hemodialysis. Clin J Am Soc Nephrol 2015; 10: 1002-10.
33.
Lin CH, Lurie RC, Lyons OD. Sleep apnea and chronic kidney disease: a state-of-the-art review. Chest 2020; 157: 673-85.
34.
Loh HH, Lim QH, Chai CS, et al. Influence and implications of the renin-angiotensin-aldosterone system in obstructive sleep apnea: an updated systematic review and meta-analysis. J Sleep Res 2023; 32: e13726.
35.
Wang X, Guan L, Wu C, et al. Continuous positive airway pressure may improve hypertension in patients with obstructive sleep apnea-hypopnea syndrome by inhibiting inflammation and oxidative stress. Arch Med Sci 2023; 19: 237-41.
36.
Hernandez AV, Pasupuleti V, Scarpelli N, et al. Efficacy and safety of sacubitril/valsartan in heart failure compared to renin-angiotensin-aldosterone system inhibitors: a systematic review and meta-analysis of randomised controlled trials. Arch Med Sci 2023; 19: 565-76.
37.
Hanly PJ, Ahmed SB. Sleep apnea and the kidney: is sleep apnea a risk factor for chronic kidney disease? Chest 2014; 146: 1114-22.
38.
Chang CP, Li TC, Hang LW, et al. The relationships of sleep apnea, hypertension, and resistant hypertension on chronic kidney disease. Medicine 2016; 95: e3859.
39.
Beaudin AE, Raneri JK, Ahmed SB, et al. Risk of chronic kidney disease in patients with obstructive sleep apnea. Sleep 2022; 45: zsab267.
40.
Watanabe Y, Tanaka A, Furuhashi K, et al. Mortality and cardiovascular events in patients with chronic kidney disease and sleep apnea syndrome. Front Med (Lausanne) 2022; 9: 899359.
41.
Zamarrón E, Jaureguizar A, Gardia-Sanchez A, et al. Continuous positive airway pressure effect on albuminuria progression in patients with obstructive sleep apnea and diabetic kidney disease: a randomized clinical trial. Am J Respir Crit Care Med 2023; 207: 757-67.
42.
El-Baroudy N, El Falaki M, Hagras A, et al. Sleep disorders in children and adolescents on regular hemodialysis. Eur J Pediatr 2020; 179: 1139-46.
43.
Papandreou C, Babio N, Diaz-Lopez A, et al. Sleep duration is inversely associated with serum uric acid concentrations and uric acid to creatinine ratio in an elderly mediterranean population at high cardiovascular risk. Nutrients 2019; 11: 761.
44.
Yuen D, Richardson RMA, Fenton SSA, et al. Quotidian nocturnal hemodialysis improves cytokine profile and enhances erythropoietin responsiveness. ASAIO J 2005; 51: 236-41.
45.
Lavoie MR, Patel JA, Camacho M. Nocturnal dialysis improves sleep apnea more than daytime dialysis: a meta-analysis of crossover studies. Sleep Med 2019; 64: 37-42.
46.
Ismail AMA, Abdelhay M, Draz R, Response of salivary flow rate to transcutaneous electrical nerve stimulation in haemodialysis patients. Physiother Quart 2023; 31: 23-7.
47.
Nowicki M, Zawiasa-Bryszewska A, Taczykowska M, et al. The pattern of overnight changes in novel markers of acute kidney injury in patients with obstructive sleep apnea. Adv Clin Exp Med 2020; 29: 1065-72.
48.
Lévy P, Kohler M, McNicholas WT, et al. Obstructive sleep apnoea syndrome. Nat Rev Dis Primers 2015; 1: 15015.
Share
RELATED ARTICLE