Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CARDIOLOGY / RESEARCH PAPER
Sleep Duration May Not Have Any Effect on The Risk of Stroke: Insights from Mendelian Randomization and Prospective Cohort Studies
1
Department of Twin Research and Genetic Epidemiology, King's College London, United Kingdom
2
First Department of Internal Medicine, Division of Endocrinology and Metabolism, Diabetes Center, AHEPA University Hospital, Aristotle University of Thessaloniki, Greece
3
Faculty of Science, Liverpool Hope University, United Kingdom
4
Liverpool Centre for Cardiovascular Science, University of Liverpool and Liverpool Heart & Chest Hospital, United Kingdom
5
Institute of Cardiovascular and Medical Sciences, University of Glasgow, United Kingdom
6
Department of Hypertension, Chair of Nephrology and Hypertension, Medical University of Lodz (MUL), Poland
7
Polish Mother’s Memorial Hospital Research Institute (PMMHRI), Poland
8
Cardiovascular Research Centre (CRC), University of Zielona Gora, Poland
Submission date: 2021-11-09
Final revision date: 2021-11-26
Acceptance date: 2021-11-27
Online publication date: 2021-11-27
Corresponding author
Maciej Banach
Department of Hypertension, Chair of Nephrology and Hypertension, Medical University of Lodz (MUL), Lodz, Poland
Department of Hypertension, Chair of Nephrology and Hypertension, Medical University of Lodz (MUL), Lodz, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Due to contentious associations between sleep and stroke risk we performed a meta-analysis of cohort studies and utilized Mendelian randomization (MR).
Material and methods:
For the meta-analysis we pooled prospective studies and then reviewed the largest genome-wide association studies regarding self-reported or accelerometer-derived sleep duration with stroke [ischemic (IS), cardioembolic (CES), large artery (LAS), small vessel (SVS)]. Inverse variance weighted method (IVW), weighted median (WM)-based method, MR-Egger and MR-Pleiotropy RESidual Sum and Outlier (PRESSO) were performed. To determine the impact of single nucleotide polymorphisms (SNPs) leave-one-out method was applied.
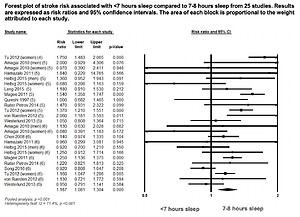
Results:
Pooled prospective studies demonstrated shorter (<7h) [n=25 studies, I2 = 71.4, p <0.001; risk ratio (RR): 1.18, 95%CI: 1.08-1.30, p <0.001] and longer (>8h) [n=16 studies, I2 = 53.6, p <0.001; RR: 1.38, 95%CI: 1.24-1.53, p <0.001] sleep increased stroke risk (compared with 7-8h), but were subject to high levels of heterogeneity. In MR, self-reported sleep duration had no significant effect on IS (IVW: beta = -0.031, p = 0.747), CES (IVW: beta = -0.039, p = 0.849), LAS (IVW: beta = -0.246, p = 0.328) and SVS (IVW: beta = -0.102, p = 0.667) risk. This was also observed for short and long accelerometer-derived sleep (all p >0.126). Estimated associations had no significant heterogeneity and MR-PRESSO revealed no outliers. There was low likelihood of pleiotropy (all estimations p >0.539) and associations were not driven by single SNPs.
Conclusions:
Meta-analysis revealed shorter and longer sleep increased total stroke risk, but with high heterogeneity. MR analysis showed no causal associations between sleep duration and stroke risk.
Due to contentious associations between sleep and stroke risk we performed a meta-analysis of cohort studies and utilized Mendelian randomization (MR).
Material and methods:
For the meta-analysis we pooled prospective studies and then reviewed the largest genome-wide association studies regarding self-reported or accelerometer-derived sleep duration with stroke [ischemic (IS), cardioembolic (CES), large artery (LAS), small vessel (SVS)]. Inverse variance weighted method (IVW), weighted median (WM)-based method, MR-Egger and MR-Pleiotropy RESidual Sum and Outlier (PRESSO) were performed. To determine the impact of single nucleotide polymorphisms (SNPs) leave-one-out method was applied.
Results:
Pooled prospective studies demonstrated shorter (<7h) [n=25 studies, I2 = 71.4, p <0.001; risk ratio (RR): 1.18, 95%CI: 1.08-1.30, p <0.001] and longer (>8h) [n=16 studies, I2 = 53.6, p <0.001; RR: 1.38, 95%CI: 1.24-1.53, p <0.001] sleep increased stroke risk (compared with 7-8h), but were subject to high levels of heterogeneity. In MR, self-reported sleep duration had no significant effect on IS (IVW: beta = -0.031, p = 0.747), CES (IVW: beta = -0.039, p = 0.849), LAS (IVW: beta = -0.246, p = 0.328) and SVS (IVW: beta = -0.102, p = 0.667) risk. This was also observed for short and long accelerometer-derived sleep (all p >0.126). Estimated associations had no significant heterogeneity and MR-PRESSO revealed no outliers. There was low likelihood of pleiotropy (all estimations p >0.539) and associations were not driven by single SNPs.
Conclusions:
Meta-analysis revealed shorter and longer sleep increased total stroke risk, but with high heterogeneity. MR analysis showed no causal associations between sleep duration and stroke risk.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.