Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CARDIOLOGY / RESEARCH PAPER
ST2L expression on monocyte subsets is associated with the severity of acute coronary syndrome and plaque vulnerability
1
Department of Cardiology, Shanghai Tenth People’s Hospital, Tongji University School of Medicine, Shanghai, China
Submission date: 2020-03-12
Final revision date: 2020-08-22
Acceptance date: 2020-09-02
Online publication date: 2021-05-03
Corresponding author
Jianhui Zhuang
Department of Cardiology, Shanghai Tenth People’s Hospital, Tongji University School of Medicine, Shanghai, China
Department of Cardiology, Shanghai Tenth People’s Hospital, Tongji University School of Medicine, Shanghai, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Pro-inflammatory monocyte infiltration and conversion to macrophages is an established risk factor for acute coronary syndrome (ACS) and plaque instability visualized by optical coherence tomography (OCT). Increased serum levels of soluble ST2 isoform (sST2) predict poor outcomes in patients with ACS. However, whether the transmembrane ST2 isoform (ST2L) could early assess the severity of ACS and the vulnerability of plaques remains elusive.
Material and methods:
Flow cytometry and ELISA were performed to evaluate the levels of ST2L on different monocyte subsets in ACS patients and serum concentration of sST2. Bone marrow-derived macrophages (BMDMs) were isolated and polarized to M1 or M2 phenotype, which levels of ST2L expression were detected by Quantitative RT-PCR and Immunoblots.
Results:
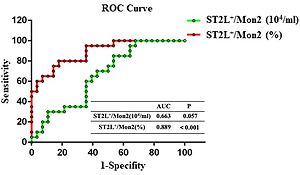
The proportion and absolute number of ST2L on monocyte subsets 1 (Mon1) and Mon2 significantly declined, accompanied with increased serum sST2, in ACS patients comparing with controls. However, only proportion of ST2L+/Mon2 remained closely associated with the severity of atherosclerotic plaques. Patients with thin cap fibrous atheroma (TCFA) calculated by OCT had lower absolute number (Non-TCFA 1.26×104 ± 0.63×104/ml vs. TCFA 0.92×104 ± 0.37×104/ml, P = 0.034) and lower percentage (Non-TCFA 17.65% ± 3.10% vs. TCFA 13.17% ± 2.29%, P < 0.001) of ST2L+/Mon2 than those without TCFA. In multivariate analysis, the proportion of ST2L+/Mon2 was considered as an independent determinant for TCFA. In BMDMs, sST2 and ST2L were highly expressed in M2 macrophage.
Conclusions:
Compared to circulating sST2, the proportion of ST2L expressing on Mon2 subsets was more strongly associated with the severity of ACS and plaque vulnerability.
Pro-inflammatory monocyte infiltration and conversion to macrophages is an established risk factor for acute coronary syndrome (ACS) and plaque instability visualized by optical coherence tomography (OCT). Increased serum levels of soluble ST2 isoform (sST2) predict poor outcomes in patients with ACS. However, whether the transmembrane ST2 isoform (ST2L) could early assess the severity of ACS and the vulnerability of plaques remains elusive.
Material and methods:
Flow cytometry and ELISA were performed to evaluate the levels of ST2L on different monocyte subsets in ACS patients and serum concentration of sST2. Bone marrow-derived macrophages (BMDMs) were isolated and polarized to M1 or M2 phenotype, which levels of ST2L expression were detected by Quantitative RT-PCR and Immunoblots.
Results:
The proportion and absolute number of ST2L on monocyte subsets 1 (Mon1) and Mon2 significantly declined, accompanied with increased serum sST2, in ACS patients comparing with controls. However, only proportion of ST2L+/Mon2 remained closely associated with the severity of atherosclerotic plaques. Patients with thin cap fibrous atheroma (TCFA) calculated by OCT had lower absolute number (Non-TCFA 1.26×104 ± 0.63×104/ml vs. TCFA 0.92×104 ± 0.37×104/ml, P = 0.034) and lower percentage (Non-TCFA 17.65% ± 3.10% vs. TCFA 13.17% ± 2.29%, P < 0.001) of ST2L+/Mon2 than those without TCFA. In multivariate analysis, the proportion of ST2L+/Mon2 was considered as an independent determinant for TCFA. In BMDMs, sST2 and ST2L were highly expressed in M2 macrophage.
Conclusions:
Compared to circulating sST2, the proportion of ST2L expressing on Mon2 subsets was more strongly associated with the severity of ACS and plaque vulnerability.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.