Introduction
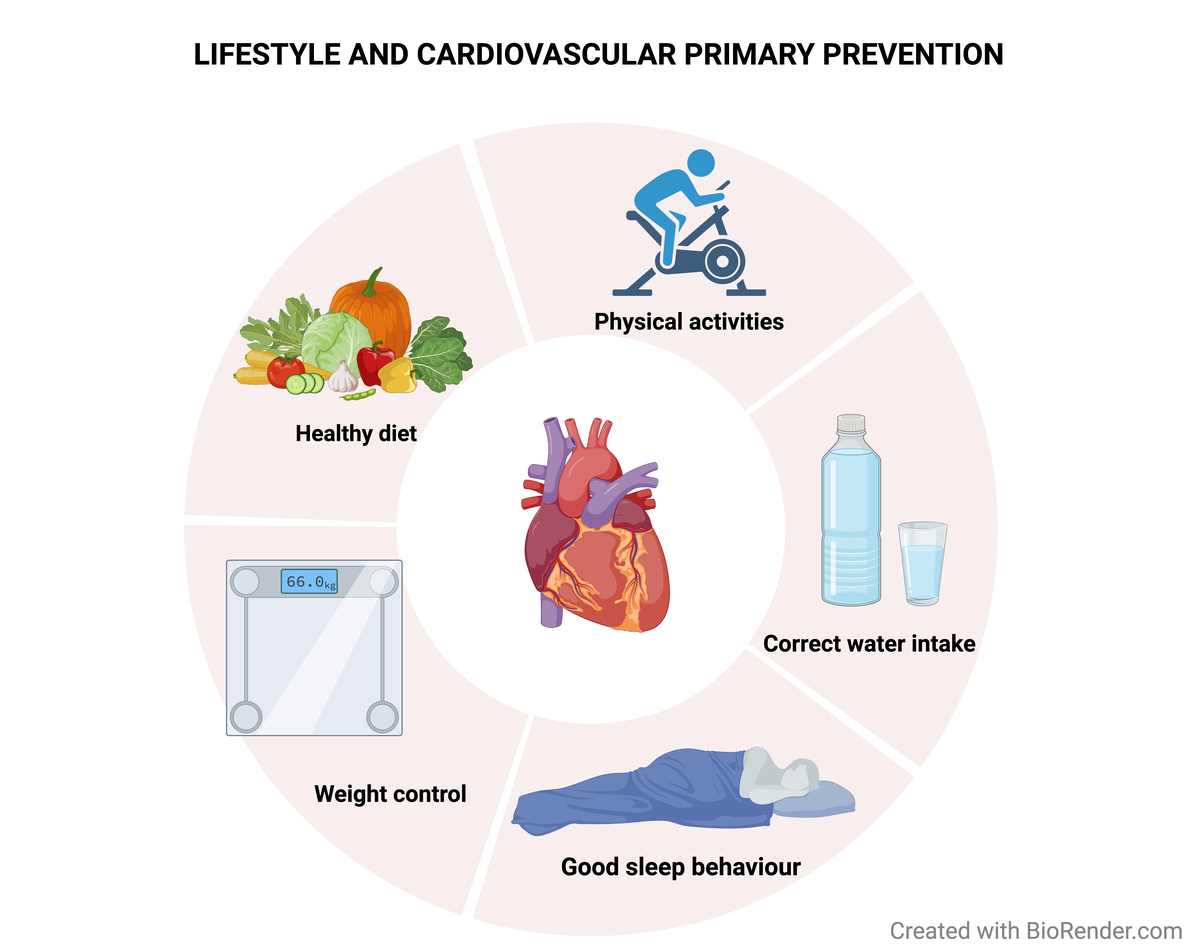
Despite major progress in recent decades, cardiovascular diseases (CVD) still represent the leading cause of mortality and morbidity worldwide [1]. Recent international guidelines on cardiovascular prevention have underscored the pivotal role of adopting a healthy lifestyle and dietary habits [2, 3]. While these guidelines advocate for a holistic approach to mitigate the burden of cardiovascular diseases, there still remains a significant gap in translating these recommendations into practical and patient-tailored advice within the healthcare community [4]. Lifestyle measures can significantly reduce the risk of developing cardiovascular diseases. By making changes such as adhering to a healthy diet, participating in regular physical activity, quitting smoking, and limiting alcohol intake, individuals can positively impact their cardiovascular health and decrease their chances of developing life-threatening conditions. The components of metabolic syndrome (MS), namely obesity, hypertension, impaired glucose metabolism, and dyslipidemia, constitute significant and modifiable cardiovascular (CV) risk factors. Recognizing individuals with metabolic syndrome is crucial, as they are deemed to be at an increased risk of cardiovascular disease. Achieving weight loss through a healthy diet is a pivotal step in the management of this condition [5].
Definition of a “healthy diet”
According to the Scientific Group of the United Nations Food System Summit, a healthy diet is “health-promoting and disease-preventing; providing adequacy, without excess, of nutrients and health promoting substances from nutritious foods and avoids the consumption of health-harming substances” [6]. However, characterizing a healthy diet and nutritious food is not as simple as it appears. Scientific research suggests that certain dietary choices can either benefit or harm our overall health. Furthermore, there is no consensus among experts on how to establish nutrient requirements that would be effective for each individual. Personalization may be necessary to ensure that dietary recommendations are tailored to each person’s unique characteristics. Unfortunately, we have yet to achieve this level of precision in the field of nutrition science. In addition, there remains an incomplete understanding of the nutrient and “anti-nutrient” content of food, for instance substances that impact the absorption and bioavailability of nutrients. According to the World Heart Organization, for an adult, a healthy diet includes: fruits and vegetables (at least 5 portions), legumes, nuts, and whole grains. Less than 5–10% of total energy intake should be derived from sugars, and less than 30% from fats; within this fat intake, a preference for unsaturated fats over saturated fats and trans fats is advocated. Additionally, daily salt intake should be limited to less than 5 g [7]. However, it is important to note that these guidelines, particularly the recommendation on total fat intake, are subject to ongoing debate. Traditional Mediterranean diets, for instance, often exceed this fat intake percentage while still being associated with lower CVD risks, suggesting the critical role of fat quality rather than quantity.
Diets with proven benefits
Among the top ten dietary strategies to reduce atherosclerotic cardiovascular disease (ASCVD), it is recommended to utilize evidence-based heart-healthy eating patterns [8].
Some of the diets with proven benefits include the Mediterranean-style dietary pattern, the Dietary Approaches to Stop Hypertension (DASH) diet, vegetarian, vegan, flexitarian plant-based dietary patterns and low-fat/very high carbohydrate diets (Table I).
Table I
Comparative overview of evidence-based eating patterns with proven benefits
The Mediterranean diet is a dietary pattern that has been traditionally followed in olive-growing countries of the Mediterranean basin, such as Greece, Southern Italy, and Spain. It is characterized by the abundant use of olive oil as the primary culinary fat (preferring use of unsaturated fats over saturated ones), and the consumption of fruits and vegetables, legumes, nuts, and cereals. Moderate intake of red wine is also a part of the Mediterranean diet, usually consumed with meals. Additionally, the Mediterranean diet includes moderate consumption of fish and dairy products, and low consumption of whole milk, butter, or cream. Red and processed meats and sweet desserts are also consumed in low amounts [9]. As already shown, countries that adopt the Mediterranean diet pattern showed a lower risk of coronary heart disease (CHD) compared to northern European countries and the United States over 25 years of observations [10]. Adherence to the Mediterranean diet also appears to reduce liver fat in non-alcoholic fatty liver disease (NAFLD) [11]. The Seven Countries Study was the first to examine the relationship between the intake of various food groups and 25-year mortality rates from coronary heart disease [10]. The study involved 12,763 middle-aged men from seven different countries (USA, Finland, The Netherlands, Italy, former Yugoslavia, Greece, and Japan) who were divided into 16 cohorts. The participants’ food and drink consumption was recorded during the observation period. The vital status of all men, including mortality data and causes of death, was checked regularly for 25 years. The study revealed significant differences in food-group consumption, with Northern Europe having high dairy product consumption, the USA having high meat consumption, and Southern Europe having high consumption of legumes, fish and wine and Japan having high consumption of fish, cereals and soy products. Dietary patterns associated with elevated mortality rates from CHD were distinguished by increased consumption of butter, dairy products, and other animal-derived foods containing high levels of saturated fatty acids and cholesterol. In contrast, dietary patterns linked to low or comparatively low mortality rates from CHD were characterized by elevated intake of cereals, legumes, vegetable products, fish, oils, and moderate consumption of wine. These findings justify the current interest in the Mediterranean diet’s role in preventing CHD, both primary and secondary.
Among the milestone studies that contributed to the growing body of evidence supporting the health benefits of a Mediterranean diet was the PREDIMED study, a randomized controlled trial (RCT) examining whether the addition of extra virgin olive oil or mixed nuts to a Mediterranean diet could reduce cardiovascular events [12]. This study was a multicenter, nutritional intervention RCT, conducted in Spain. The study involved over 7,000 participants aged 55-80 years, followed for an average of 4.8 years, who were at high risk of cardiovascular disease. Participants were randomly assigned to three groups: the Mediterranean diet supplemented with extra virgin olive oil, the Mediterranean diet supplemented with mixed nuts, and the control group following a low-fat diet. The primary outcome of the study was the occurrence of major adverse cardiovascular events (MACE), such as heart attacks, strokes, and cardiovascular-related deaths. Additionally, the study aimed to measure secondary outcomes such as changes in weight, blood pressure, blood lipid levels, and markers of inflammation. The results of the study, published in 2013, showed that both Mediterranean diet groups had a significantly lower risk of MACE compared to the control group: those following the Mediterranean diet supplemented with extra virgin olive oil experienced a 30% reduction in the risk of MACE, while those on the Mediterranean diet with mixed nuts experienced a 28% risk reduction. These findings demonstrate the protective effects of the Mediterranean diet in preventing cardiovascular diseases and highlight the importance of incorporating healthy dietary habits in daily life.
The Mediterranean diet’s role in prevention is further underscored when considering the so-called French paradox [13], which refers to the observation that the French population tends to have a low incidence of CHD despite having a diet rich in saturated fats, which are typically associated with higher risk of CHD. This paradox was initially popularized in the 1980s and has since intrigued scientists and nutritionists. This apparent contradiction is actually not a paradox at all but a manifestation of the varying degrees of adherence to the Mediterranean diet across different regions of France. It is more pronounced in the South, with higher adherence to the Mediterranean diet and, consequently, a lower rate of cardiovascular incidents, which contrasts with the North. This gradient effect reflects the diet’s protective benefits [14].
Another prospective cohort study, conducted in the UK, with more than 23,000 participants without histories of cardiovascular events such as myocardial infarctions or strokes, demonstrated that adherence to a Mediterranean diet led to a significant reduction in cardiovascular disease rates [15]. Several other studies conducted in non-Mediterranean countries (Subarctic Region, Denmark, the Netherlands) have confirmed the protective effects of the Mediterranean diet [16–18]. The Mediterranean diet is rich in antioxidant and anti-inflammatory molecules which can influence cell redox state, modulating enzyme systems, gene and protein expression, with a protective effect on vascular inflammation, foam cell formation and thrombosis, lowering low-density lipoprotein (LDL) cholesterol and triglyceride levels, as well as incidence and progression of type 2 diabetes, reducing blood pressure and promoting overall heart health [19–23]. The Mediterranean diet has also demonstrated potential benefits in the field of oncology, as shown by the study of Couto et al. 24 in 2011 [24], which examined the relationship between adherence to the Mediterranean dietary pattern and overall cancer risk. The authors used data from the European Prospective Investigation Into Cancer and Nutrition (EPIC), a large multi-center prospective cohort study that included 142,605 men and 335,873 women. Notably, the study showed that higher adherence to a Mediterranean diet was associated with a lower risk of overall cancer. In particular, for every two-point increment in adherence to the Mediterranean diet score, the risk of cancer decreased by 4% overall. This finding suggests that the Mediterranean diet could have a significant public health impact on cancer prevention. While focusing on primary prevention, it is worth briefly acknowledging the findings of the Lyon Heart Trial [25], which evaluated the benefits of a Mediterranean-style diet on cardiovascular disease, particularly following a first myocardial infarction. The study demonstrated that people following the Mediterranean-style diet had a 50% to 70% lower risk of recurrent heart disease over a follow-up period of 46 months. Notably, the trial was concluded prematurely due to the unexpectedly large effect size, underscoring the potential for dietary modification in disease prevention strategies.
Furthermore, extensive research has been conducted on the DASH diet and the findings have consistently demonstrated its efficacy in reducing high blood pressure levels [26]. This dietary approach has also been linked to several other health benefits, such as enhanced lipid profiles, better weight management, and a reduced risk of cardiovascular disease, e.g. prevention of heart failure [27, 28]. Therefore, it is frequently recommended for individuals dealing with hypertension or aiming to improve their heart health. The main objective of this diet is to encourage the consumption of nutrient-rich foods while also reducing the intake of unhealthy fats and sodium (salt). The DASH diet emphasizes the importance of incorporating fruits, vegetables and whole grains, rich in vitamins, fiber, and antioxidants. Moreover, individuals are advised to choose lean protein sources such as poultry and fish, as they contain lower levels of saturated fats compared to red meat. A key component of the DASH diet involves limiting sodium intake, which entails decreasing the consumption of high-sodium foods such as processed meats and fast-food items. By doing so, individuals can significantly lower their blood pressure levels [29]. Lastly, the DASH diet advises limiting the consumption of sugary beverages, which has been associated with increased blood pressure and other cardiovascular risks.
An alternative healthy dietary pattern is the plant-based diet, which includes vegetarian, vegan, and flexitarian versions, highlighting the consumption of fruits, vegetables and legumes, while restricting or abstaining from animal-derived products [30]. When comparing omnivores, who consume a variety of food sources including both plant-based and animal-derived products, and vegetarians and vegans, who predominantly or exclusively rely on plant-based foods for sustenance, the latter have a lower body mass index (BMI), LDL cholesterol, glucose, and C reactive protein and trimethylamine-N-oxide (TMAO) levels, and a lower incidence of overall and cardiovascular mortality [31, 32]. Numerous potential biological pathways may explain the positive effect on cardiovascular health of plant-based diets. Firstly, the high fiber content triggers satiety, increasing gastric distension and delaying gastric emptying, prolonging nutrient absorption, and lowering cholesterol levels. Polyunsaturated and monounsaturated fats enhance insulin sensitivity while the high content of polyphenols reduces oxidative stress. Furthermore, polyphenols play a crucial role in inhibiting platelet aggregation, reducing vascular inflammation and LDL oxidation, which results in an improvement of lipid profile. Conversely, certain dietary components commonly found in animal-derived foods, such as heme iron, have been linked to an increased risk of cardiovascular events due to their oxidative properties. It has also been shown that nitrates, nitrites, and sodium used in the preservation of processed meats may also increase blood pressure levels, and impair the insulin response and endothelial function, all of which may lead to cardiovascular problems. Moreover, researchers found that some low-fat, high-carbohydrate diets reduce rates of ASCVD and are somehow cardioprotective. These are characterized by a reduction in dietary fat, particularly saturated and trans fats, and an increase in carbohydrate consumption, particularly fruits, vegetables and legumes; complex carbohydrates are preferred over refined or processed carbohydrates. Fatty acids can be categorized as saturated and unsaturated, with the latter further classified as monounsaturated (MUFA) and polyunsaturated (PUFA) [33]. Saturated fatty acids (SFAs) are commonly found in animal fats while unsaturated fatty acids are primarily found in plant-based oil. Polyunsaturated fatty acids are classified into omega-3 and omega-6, with the former having anti-inflammatory properties and potential cardiovascular benefits [34]. Trans-fatty acids, produced through hydrogenation, should be avoided or minimized in the diet due to their link to an increased risk of heart disease [35]. It is recommended to prioritize unsaturated fats, including MUFAs and PUFAs, while minimizing saturated fats and avoiding trans fats. Research has revealed that SFAs can elevate the levels of LDL cholesterol, trigger inflammation and impede endothelial function, all of which can result in the formation of plaques. Moreover, SFAs can induce oxidative stress and contribute to the development and progression of atherosclerosis. Furthermore, SFAs promote blood clotting, leading to a prothrombotic state and increasing the chances of experiencing cardiovascular events such as heart attacks and strokes [36]. Although certain evidence suggests that preferring polyunsaturated fat over saturated fat can reduce the risk of cardiovascular disease, there are limited epidemiologic or clinical trial data to support the notion that substituting saturated fat with carbohydrate provides any advantages. Particularly, replacement with refined carbohydrates can exacerbate atherogenic dyslipidemia, insulin resistance, hypertriglyceridemia and obesity [37, 38]. It is likely that these aforementioned diets are considered healthy as they do not place a high emphasis on one macronutrient, but rather emphasize consuming a balanced diet that includes healthy fats, whole grains, fruits, vegetables, and lean proteins, thus reducing cardiovascular risk.
Carbohydrates: quality matters for health
According to the carbohydrate–insulin model [39], diets characterized by a high carbohydrate content elevate blood glucose levels and stimulate insulin secretion. Consequently, this inhibits the release of fatty acids from adipose tissue into the bloodstream and redirects circulating fat toward adipose storage rather than its oxidation by metabolically active tissues. This phenomenon may induce a state of cellular “internal starvation” resulting in an adaptation to reduce energy expenditure and increase hunger levels. As a result, insulin resistance, obesity, and the development of type 2 diabetes can occur over time. According to the carbohydrate-insulin model, positive energy balance results primarily from endocrine dysregulation of adipose tissue [40]. For the above assumption, low and very-low carbohydrate diets have gained popularity in recent years, but their impact on health remains a subject of debate. These diets result in a reduction in body weight, as proteins provide a higher level of satiety and ketone bodies provide direct appetite suppression. In addition, blood glucose levels and glycosylated hemoglobin are improved, plasma lipid profiles are improved, with an increase in HDL cholesterol, a reduction in total cholesterol, and a reduction in blood triglycerides [41]. Nevertheless, the enduring impacts and feasibility of these dietary approaches are still under investigation. A key consideration is the quality of the macronutrients substituted for carbohydrates. According to Seidelamann et al. [42], both high and low percentages of carbohydrates are associated with an increase in mortality. In particular, diets low in carbohydrates that are primarily based on animal proteins were associated with higher mortality, whereas those that are based on plant proteins were associated with lower mortality. The nature or composition of carbohydrates is also found to be important. In the PURE study [43], a prospective cohort study involving over 130,000 individuals without cardiovascular disease with the aim to assess the relationship between consumption of fruits, vegetables, legumes and cardiovascular disease and mortality, the researchers discovered that increased consumption of fruits, vegetables, and legumes correlated with a decreased risk of major cardiovascular disease, cardiovascular and non-cardiovascular mortality, and overall mortality. These foods, attributed to their antioxidant and polyphenol constituents, are recognized for their ability to lower blood pressure, inhibit lipid oxidation, and enhance endothelial function. Additionally, their rich fiber content has been demonstrated to attenuate the insulin response to carbohydrates and reduce total and LDL cholesterol levels [43]. There are several markers of carbohydrate quality; particularly, there are four main markers: high-quality carbohydrates, low glycemic index and glycemic load, high fiber, and low sugar, whose consumption leads to weight loss and maintenance, enhanced glycemic control, improved blood lipids, and blood pressure regulation [44]. Moreover, their intake is associated with a reduction in the incidence of cardiovascular disease, cardiovascular mortality, and overall mortality. The consumption of sugar-sweetened beverages is associated with obesity, diabetes, heart disease, and stroke. However, other important food sources of sugars, such as grains and grain products, dairy products, and fruits and fruit products, did not show harmful associations. It has been observed that putting emphasis on the quantity of carbohydrates may not be as effective as focusing on the quality of carbohydrates. It is recommended to prioritize the quality of carbohydrates over their quantity for better health outcomes [44].
The role of eggs
Over the years, research and debate have focused on the impact of egg consumption on cholesterol levels and cardiovascular risk, considering not only the dietary cholesterol but also the choline content, which is metabolized by gut bacteria into trimethylamine (TMA) and subsequently oxidized to TMAO. While it is hypothesized that TMAO may contribute to atherosclerosis, this pathway has not been definitively linked to the causal mechanism for atherosclerosis. Furthermore, eggs contain essential nutrients, comprising high-quality protein, vitamins and minerals, and antioxidants, including lutein and zeaxanthin, which help prevent inflammation, oxidation, and atherosclerosis [45]. There are no controlled trials demonstrating an adverse impact of egg consumption on cardiovascular disease risk among individuals at lower or higher risk. For example, in a study where healthy volunteers consumed 0, 1, 2, 4, or 6 egg yolks during a 24-hour period, while an increase in plasma TMAO was noted beyond two eggs, no corresponding increase in markers of cardiovascular risk such as high-sensitivity C-reactive protein (hsCRP) or oxidized low-density lipoprotein was observed [46].
The evidence strongly suggests that in a wide variety of apparently healthy subjects, adding eggs to normal dietary intake does not adversely affect blood lipid profiles, which are risk factors for coronary heart disease across a range of ages and ethnicities [45]. Overall, the available research indicates that consuming eggs does not have detrimental effects on certain markers associated with cardiovascular disease risk in individuals at high risk for CVD, such as overweight and obese adult men [47]. In their study, Blesso et al. [48], included 37 individuals suffering from metabolic syndrome who were randomly assigned either to consume three whole eggs or an egg substitute for 12 weeks. Over time, the total carbohydrate intake decreased significantly in all participants, resulting in improvements in dyslipidemia and decreases in waist circumference, weight, and percent body fat. In the EGG group, which consumed more dietary cholesterol and choline than the sub-group, reduction of tumor necrosis factor-α and serum amyloid A was observed. In general, the available research suggests that eating eggs does not negatively alter some markers of CVD risk in individuals at high risk for CVD, such as overweight and obese adults [45]. Thus, eggs can be part of a healthy, balanced diet when consumed with moderation.
Focus on TMAO
Recently, TMAO has been gaining attention for its potential association with cardiovascular risk [49]. This molecule derives from the metabolism of certain dietary components, particularly choline and carnitine. There is a high level of choline and carnitine in red meat, which is metabolized in the gut by bacteria in TMA, which is then transported to the liver and converted into TMAO. While TMAO has been associated with several mechanisms that could contribute to cardiovascular disease, such as oxidative stress and inflammation, it has not been confirmed as a direct causative agent in atherosclerosis [50]. Additionally, TMAO has been implicated in potential carcinogenic processes [51]. The association between TMAO, red meat consumption, and cardiovascular risk is an area of ongoing research. Although reducing the intake of choline and carnitine-rich foods can lower TMAO levels in some individuals, the clinical significance of this reduction is still under debate [52]. Therefore, the discussion of TMAO in relation to cardiovascular disease should be approached with caution, acknowledging that the current evidence does not definitively place it within the causal pathway of atherosclerosis.
Other nutritional issues
Coffee
Coffee and tea are two of the most widely consumed beverages globally. Besides caffeine, coffee and tea contain hundreds of other active biochemical compounds including polyphenols such as catechins and chlorogenic acid, which have anti-oxidant and anti-inflammatory properties [53]. Several studies have shown that frequent coffee consumption at low-moderate levels (2–3 cups per day) has beneficial effects on the cardiovascular system [54]. In particular, by decreasing arterial stiffness, regular coffee intake decreases the risk of hypertension [55, 56]. Furthermore, coffee has been linked to weight loss through various mechanisms, including hindering the absorption of fatty acids in the gut, suppressing lipogenesis and elevating the body’s basal metabolic rate [57, 58]. Coffee consumption triggers the release of gastrointestinal peptides such as gastric inhibitory polypeptide (GIP) while decreasing the secretion of glucagon-like peptide-1 (GLP-1), reducing glucose absorption in the small intestine. Additionally, the phenols in coffee stimulate insulin-mediated cellular glucose uptake by activating GLUT-4 and the insulin receptor. These mechanisms may explain the lower incidence of type 2 diabetes mellitus among regular coffee consumers [59]. Coffee intake, in particular unfiltered coffee, apparently increases serum triglycerides, cholesterol and LDL. This is attributed to high concentration of cholesterol-elevating diterpenes such as cafestol and kahweol, which inhibit cholesterol 7α-hydroxylase, a key enzyme in bile acid synthesis [60, 61]. In summary, moderate coffee intake is linked to a noteworthy decrease in the likelihood of CHD [62] and incident heart failure HF [63]. Additionally, the available evidence indicates that coffee consumption is not only safe but may also offer protection against atrial arrhythmias, particularly atrial fibrillation [64]. Furthermore, coffee consumption is associated with reduced occurrence of transient ischemic attacks and strokes. This positive impact is attributed to polyphenols, which contribute to enhanced endothelial function, increased bioavailability of nitric oxide, and favorable glucose profiles [65]. Moderate and regular consumption of caffeinated beverages, especially a daily intake of 2–3 cups of coffee or tea, seems to pose no harm across a diverse spectrum of cardiovascular conditions and might even have potential health benefits [66, 67].
Nuts
Nuts are a rich source of complex carbohydrates, unsaturated fats, including monounsaturated fatty acids and polyunsaturated fatty acids, fiber, vitamins, minerals, and phytosterols. Research indicates that consuming nuts may reduce the risk of cardiovascular disease, overweight, and obesity [68, 69]. The protective effects of frequent nut consumption on coronary heart disease deaths and nonfatal outcomes were first observed in the early 1990s in study participants who did not have a history of heart disease or diabetes [70]. Since then, a growing body of observational studies and clinical trials has confirmed the cardioprotective effects of nuts [71–73]. In particular, incorporating hazelnuts and cashews into the diets of normolipidemic and hyperlipidemic men and women has been linked to lower total and LDL cholesterol levels resulting from reduced cholesterol and bile acid absorption, increased bile acid and cholesterol excretion, and increased LDL cholesterol receptor activity due to their low saturated fat content and high MUFA and PUFA content [74, 75]. Furthermore, the consumption of nuts may potentially enhance endothelial function due to their rich protein content and L-arginine, which is a precursor to nitric oxide, an endogenous vasodilator [76]. Research has shown that consuming nuts significantly improves endothelial function as measured by flow-mediated dilatation. α-linolenic acid, which is present in nuts, may increase the fluidity of endothelial membranes, promote nitric oxide synthesis, and reduce inflammation in endothelial cells [77]. In addition to nuts, other nutritional issues that are important to consider include the omega-3 fatty acids, which are essential polyunsaturated fats for human health, primarily found in certain types of fish. Omega-3 fatty acids include eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA) and α-linolenic acid (ALA). According to research, omega-3 fatty acids can significantly reduce the risk of cardiovascular disease [78]. In 1980, a study conducted in Japan compared fishermen who consumed high quantities of fish with rural residents who had comparatively low fish intake. The findings revealed a significantly lower mortality rate from ischemic heart disease and cerebrovascular disease among fishermen when compared to rural residents. Fishermen consumed an average of 2600 mg of EPA per day, which is approximately three times that of rural residents [79]. An association was observed between the fishermen’s diet and reduced platelet aggregation capacity and viscosity of blood, along with a 30% decrease in triglyceride levels compared to the dietary habits of rural residents. Additionally, supplementation with fish oil has been shown to moderately lower blood pressure, potentially due to a reduction in systemic vascular resistance [80]. Furthermore, the consumption of omega-3 PUFA may increase the expression of endothelial nitric oxide synthase and the production of NO. In addition, E-selectin, VCAM-1, and ICAM-1, serum markers of endothelial dysfunction, are improved by omega-3 PUFA intake [81]. The reduction of serum triglycerides in patients suffering from hypertriglyceridemia has been demonstrated by omega-3 PUFAs. This reduction is associated with mechanisms such as reduced hepatic synthesis and secretion of VLDL triglycerides and increased triglyceride clearance from chylomicrons and VLDL particles [82].
Fiber-rich foods
Fibers are a type of carbohydrate that cannot be digested by human enzymes. Soluble and insoluble fibers are the two main types of dietary fiber. In the digestive tract, soluble fiber dissolves in water and a gel-like substance is obtained, which increases transit time for food, delays gastric emptying, reduces nutrient absorption, and slows digestion [83]. By fermentation, soluble fiber is converted into short-chain fatty acids, which decrease cholesterol synthesis in the liver, resulting in lower blood cholesterol levels [84]. Insoluble fiber does not dissolve in water, and, unlike soluble fiber, insoluble fiber decreases transit time and increases fecal bulk, promoting regular bowel movements and preventing constipation. Over the years, observational studies and randomized control trials have suggested that dietary fiber intake was associated with a lower risk of heart disease, having favorable effects on serum lipoproteins, blood pressure, insulin sensitivity, both in diabetic and non-diabetic subjects, and body weight, due to delayed gastric emptying and increased satiety [85–89]. The WHO suggests a daily intake of at least 25 g of dietary fiber for adults.
Calcium and vitamin D
Vitamin D and calcium are essential nutrients that significantly affect bone health. The role they play in cardiovascular health has been studied in recent decades.
It has been proposed that vitamin D may positively affect the cardiovascular system through multiple mechanisms, such as inhibition of the renin-angiotensin-aldosterone system, insulin sensitization, and regulation of immunity, along with effects that combat fibrosis, hypertrophy, and atherosclerosis [90].
As a result of low levels of vitamin D, renin gene expression and smooth muscle cell proliferation may increase, which in turn causes an increase in blood pressure, resulting in hypertension. Additionally, a reduction in vitamin D may lead to a decrease in insulin sensitivity, resulting in diabetes and an increase in pro-inflammatory cytokines and adhesion molecules, resulting in endothelial dysfunction and atherosclerosis [91].
In observational studies, vitamin D deficiency has been linked to an increased risk of cardiovascular disease [92, 93].
However, vitamin D supplementation did not appear to have a cardiovascular benefit in randomized trials [94, 95]. Of interest, the D-Health Trial was a large randomized controlled trial investigating the effect of vitamin D on mortality among older Australians [96]. The study involved 21,315 participants aged 60 years or older, who were randomized to receive either 60,000 IU of vitamin D3 or a placebo once a month for 5 years. The primary endpoint was all-cause mortality. The trial found that after a median follow-up of 5.7 years, there was no significant difference in all-cause mortality between the two groups. Similarly, no significant difference was observed for cardiovascular mortality or mortality from other causes. A subsequent analysis of the D-Health Trial [97], focusing on major cardiovascular events (including myocardial infarction, stroke, and coronary revascularization), showed that the rate of major cardiovascular events was slightly lower in the vitamin D group compared to the placebo group, with a hazard ratio of 0.91 (95% CI: 0.81 to 1.01).
In contrast, calcium supplements appear to increase the risk of cardiovascular disease in both observational studies and randomized controlled trials [98, 99].
Calcium levels increase smooth muscle contraction in the arteries, increasing blood pressure. As a result of its accumulation in vessels, it contributes to vascular calcification and increases the risk of thrombotic events by activating the coagulation cascade [100].
Accordingly, it is generally recommended to obtain these nutrients through a balanced diet that includes vitamin D-rich and calcium-rich foods [90].
Hydration and water intake
It is recommended to drink an adequate amount of water throughout the day and adjust intake based on individual needs and activity levels. Researchers demonstrated that reductions in total fluid intake significantly increase plasma vasopressin levels. Vasopressin stimulates the release of glucocorticoids leading to the upregulation of serum- and glucocorticoid-induced kinase 1 (SGK1) [101]. As a result of the higher vasopressin levels in low drinkers, SGK1 expression is also increased, resulting in a relevant influence on SGK1-sensitive functions. SGK1 augments renal tubular salt reabsorption, resulting in increased salt appetite and salt intake, predisposing to hypertension. In addition, SGK1 increases the sensitivity of blood platelets to stimulators, resulting in an increase in degranulation and aggregation. Furthermore, SGK1 stimulates the expression of tissue factors, thus stimulating coagulation [102].
Antioxidant-rich food
Reactive oxygen and nitrogen species are generated endogenously as part of regular cellular and metabolic activities. Oxidative stress ensues when the production of these reactive species surpasses the body’s antioxidant defenses, leading to oxidative damage that affects the normal functioning of cells and organisms. By neutralizing free radicals, antioxidants reduce oxidative stress and its potential damage to cells and tissues. Oxidative stress is believed to play a role in numerous chronic conditions, notably cardiovascular disease [103, 104]. There are various types of antioxidants, including vitamin antioxidants, such as vitamins C, E, and β-carotene, mineral antioxidants, such as zinc and selenium, and phytochemical antioxidants, such as flavonoids, polyphenols, and carotenoids, abundant in fruits, nuts, vegetables, and whole grains. Increased consumption of vitamin C, carotenoids, and α-tocopherol, indicators of fruit and vegetable intake, is linked to a decreased likelihood of cardiovascular disease, overall cancer incidence, and mortality from all causes [105]. However, a plethora of randomized trials have demonstrated that the utilization of antioxidant supplements, including β-carotene, vitamin A, vitamin C, vitamin E, and selenium, fails to confer any discernible benefits in the prevention of cardiovascular disease, cancer, or mortality [106]. It is possible that the advantages of consuming certain foods may not be solely attributable to the presence of antioxidants alone, but instead may be due to the combination of all the various components present in the food. Therefore, it could be beneficial to consider the overall nutritional content of foods rather than solely focusing on one specific component [105].
Research suggests that including dietary fiber, fruits and vegetables, legumes, and whole grains in the diet can lead to lower cholesterol levels, reduced blood pressure, and improved vascular function [107, 108].
Polyphenols, potent antioxidant compounds prevalent in plant-based foods and beverages, have been extensively researched for their role in reducing CVD risk. Green tea polyphenols, particularly catechins, have demonstrated efficacy in attenuating endothelial hyperpermeability, a critical factor in the pathogenesis of CVD, by modulating reactive oxygen species (ROS) production via the NADPH oxidase pathway [109]. Zuo et al. [110] found that treatment with GTPs decreased endothelial permeability and reduced ROS levels both in vivo in rats fed a high-fat diet and in vitro in bovine aortic endothelial cells treated with high glucose. Moreover, GTPs down-regulated the expression of NADPH oxidase subunits, mitigating ROS production and thus hyperpermeability induced by high glucose.
Additionally, black tea, often consumed more frequently in Western countries than green tea, is another significant source of dietary polyphenols. Black tea’s main phenolic components include theaflavins, which contribute to its high antioxidant activity, rivaling that of many other dietary agents. Research conducted by Rechner et al. [111] indicated that a consumer brew of black tea provides substantial polyphenols, averaging 262 mg of gallic acid equivalents per serving. This figure includes 65 mg of specifically quantified polyphenols, with thearubigins accounting for 75–82% of the total phenolics. The study also highlighted that the antioxidant activity of a serving of black tea is robust, corresponding closely with both the measured total phenolics and the sum of HPLC-quantified polyphenols.
The evidence underscores the importance of dietary polyphenols, especially from green and black tea, as antioxidants that can contribute to cardiovascular health by reducing oxidative stress and endothelial dysfunction, two key factors in the development of CVD.
Sodium reduction
High blood pressure and hypertension are a major risk factor for cardiovascular diseases. Reducing sodium intake lowers blood pressure and risk of hypertension. It also decreases cardiovascular disease and mortality risk [87]. There is a widely debated pathophysiological link between sodium intake and blood pressure elevations. Elevated salt consumption leads to water retention, expansion of circulating volumes, heightened cardiac output, and increased kidney perfusion pressure. This hemodynamic load leads to adverse microvascular remodeling. Furthermore, as suggested in several studies, excessive salt intake may cause microvascular endothelial inflammation, potentiation of local vasoconstrictive effectors and oxidative stress, causing microvascular dysfunction and increasing vascular resistances [112]. Furthermore, salt intake can have detrimental effects not only on small arteries but also on larger elastic arteries, triggering gradual structural modifications in the arterial wall. This results in alterations in the extracellular matrix of the arterial wall, fostering arterial stiffening through mechanisms independent of blood pressure [113]. So, reduction in salt intake, to approximately 5.0 g of salt per day, as recommended by the World Health Organization, reduces blood pressure values with possible benefit for vascular function and the cardiovascular system.
Weight control and cardiovascular benefits
Obesity prevalence is continuously increasing all over the world [114].
It is associated with metabolic alterations and chronic diseases, particularly cardiovascular disease. Obesity is an autonomous risk factor for cardiovascular diseases, including coronary artery disease, heart failure, and atrial fibrillation [115]. Obesity also exhibits a robust correlation with additional risk factors such as hypertension, dyslipidemia, atherosclerosis and diabetes mellitus [116]. Adipose tissue must be considered as an endocrine organ able to synthesize hormones and adipokines responsible for a low-grade systemic inflammatory state, an emblem of metabolic dysfunction. As a result, obesity is associated with impaired insulin signaling, insulin resistance and diabetes, and imbalance in cholesterol and triglyceride levels [117]. Obesity is correlated with chronic overactivity of the sympathetic nervous system. This, coupled with heightened activation of the renin-angiotensin-aldosterone system and compression of the kidneys due to surrounding adipose tissue, contributes to the development of hypertension [118]. American Guidelines recommend 300 min/week of moderate-intensity exercise for significant (≥ 5%) body weight loss or for weight loss maintenance [119]. However, according to research, either an isolated dietary intervention or combining a dietary intervention with an exercise program has proven to be more efficient at losing weight than exercise alone [120]. A global campaign should focus on both prevention and treatment of obesity in order to lower the risk of cardiovascular diseases associated with obesity [121].
Physical activities
Sedentary behavior and physical inactivity are significant modifiable CVD risk factors [122]. Sedentary behavior refers to activities that involve very little or no physical movement with low energy expenditure, such as reading, watching television or playing board games. Physical inactivity is not meeting the recommended levels of physical activity for health benefits, a minimum of 150 min per week of moderate aerobic physical activity or 75 min per week of vigorous aerobic physical activity, according to American Guidelines. In some laboratory experiments involving rats, Bey et al. observed that in addition to increasing postprandial glucose and insulin levels, sedentary behavior leads to decreased lipoprotein lipase activity, increased triglyceride uptake into red skeletal muscle, and decreased LDL concentrations [123].
Furthermore, sedentary behavior is associated with upregulation of some genes and downregulation of others. This results in mitochondrial dysfunction and oxidative stress, leading to impaired skeletal muscle quality and function [124]. Extensive epidemiological investigations and meta-analyses have revealed a substantial dose-response relationship between sedentary behavior and both all-cause and cardiovascular disease mortality. Engaging in high levels of physical activity seems to mitigate the adverse cardiovascular effects of sedentary behavior [125, 126]. There is a strong correlation between physical inactivity and a range of health issues, including impaired glucose metabolism, arterial stiffness, and endothelial dysfunction. These problems may be associated with increased afterload, left ventricular stiffening, chamber remodeling, and an elevated risk of developing heart failure [127, 128]. For this reason, regular physical activity is essential to maintain optimal cardiovascular health and reduce the risk of adverse outcomes. According to researchers, exercise training reduces systemic inflammation and oxidative stress and improves mitochondrial function. This results in improved skeletal muscle function and insulin sensitivity, a decrease in arterial and left ventricular stiffness, and, overall, a reduced risk of cardiac dysfunction [129, 130]. Physical activity benefits are linked to improvements in cardiorespiratory fitness, which is the ability of the circulatory and respiratory systems to efficiently transport oxygen during physical activity. Enhanced cardiorespiratory fitness correlates with a decreased prevalence of numerous CVD risk factors, such as hypertension, obesity, metabolic syndrome, and type 2 diabetes mellitus [131]. In conclusion, it is imperative to encourage regular physical activity to promote cardiovascular well-being and overall health.
Sleep duration
The initial definition of cardiovascular health (CVH), developed in 2010, was based on 7 health behaviors and health factors. When these behaviors and factors are optimized, they are linked to an extended cardiovascular disease-free lifespan and an enhanced quality of life. The 7 components of CVH included indicators of dietary quality, physical activity, exposure to cigarette smoking, BMI, blood pressure, total cholesterol and fasting blood glucose. In 2022, sleep was included as an additional CVH component [132]. In a systematic review, Gallicchio et al. [133] examined the associations between sleep duration and all-cause and/or cause-specific mortality. The researchers found that individuals who report sleeping for an average of 7 to 7.9 h per night have a lower risk of all-cause mortality compared to both short and long sleepers. In both men and women, this finding holds true. The specific mechanisms underlying sleep duration and mortality are being investigated [134]. Short sleep has obesogenic effects, including upregulation of appetite, lower energy expenditure, and impaired glucose metabolism [135]. Sleep deprivation, whether acute or longer term, is associated with high levels of cytokines, especially interleukin-6, tumor necrosis factor α, and C-reactive protein, a marker of cardiovascular risk [136]. This proinflammatory response, coupled with an overactive sympathetic nervous system resulting from short sleep, contributes to high blood pressure, according to researchers [137]. There is a strong association between sleep disorders and cardiovascular diseases, including coronary heart disease, hypertension, and cardiovascular disease [138]. Further studies are necessary to elucidate the effect of sleep duration on human health.
Conclusions
As the world is facing a continuously growing pandemic of obesity and physical inactivity associated with chronic stress and poor quality of sleep for many individuals, it seems more than ever crucial to implement guidelines by reinforcing awareness of non-pharmacological measures which may be applied in all individuals [139, 140]. These measures obviously should not be considered as “challengers” of pharmacological treatments in very high-risk individuals in primary prevention but more as “partners”, as both provide complementary benefits by decreasing major cardiovascular events and mortality.