Introduction
Rheumatoid arthritis (RA) is an autoimmune disease characterized by inflammatory synovitis, with peripheral joints, especially small joints in the hands and feet, being the most commonly affected sites [1]. The cervical spine is the site most susceptible to RA except for the hands and feet. Cervical instability refers to the displacement of the cervical spine beyond its physiological limits under physiological loads, which can manifest as a series of clinical syndromes such as neck pain, restricted movement, dizziness, chest tightness, etc. In severe cases, it can cause death due to compression of the cranial nerves, brainstem, or spinal cord [2, 3].
Cervical instability in rheumatoid arthritis is not rare in clinical practice, with an incidence ranging from 9% to 88% [4], but cervical spine involvement is not included in the various guidelines for RA (American College of Rheumatology, ACR and European League Against Rheumatism, EULAR) or in the indicators for disease assessment, and cervical instability in RA is often not given enough attention in clinical practice [5]. However, cervical instability can seriously affect patients’ quality of life and disease prognosis, but due to the uncertainty of the incidence situation, as well as the lack of specific clinical symptoms and the uncertainty of the risk factors, it often fails to receive sufficient attention from clinicians.
However, due to the limitations of the study sample size, the previous studies did not thoroughly analyze the risk factors for cervical instability in RA. Therefore, this study aims to comprehensively and systematically analyze the risk factors for cervical instability in RA including multiple relevant factors, and provide a theoretical basis for the early identification, prevention, and intervention of cervical instability in RA.
Material and methods
Standard protocol approvals and patient consents
The PROSPERO registry has the research protocol prospectively recorded under Registration. According to the PRISMA statement, this systematic review and meta-analysis was conducted, and it was then reported in accordance with the MOOSE standards. Furthermore, there was no need for ethics in this meta-analysis [6, 7].
Inclusion criteria
Study type: Case-control studies, cohort studies, and cross-sectional studies published on the influence factors of cervical instability in RA.
Study subjects: Diagnosed according to the RA classification criteria established by the American College of Rheumatology (1987) or European League Against Rheumatism (2010).
Criteria for determining cervical instability: Taking X-rays as an example, the definitions are as follows: ① Atlantoaxial subluxation (AAS): Considered as AAS when the anterior atlantodental interval is greater than 3 mm or (and) the posterior atlantodental interval is less than 14 mm [8]. ② Vertebral subluxation (VS): Using the Ranawat value, the distance from the anterior and posterior arch of the atlas to the center of the odontoid process is measured. VS is considered when the value is less than 15 mm for males and less than 13 mm for females [9]. ③ Subaxial subluxation (SAS): Considered SAS when the relative displacement between adjacent vertebral bodies below the axis is greater than 3.5 mm [9].
Outcome indicators: Risk factors for cervical instability caused by RA.
Exclusion criteria
(1) Study subjects with a clear history of other cervical spine diseases or cervical spine trauma. (2) Articles that are duplicates, inaccessible, or without the full text. (3) Studies evaluated as low-quality research. (4) Reviews, conference papers, patents, etc.
Literature search strategy
We conducted a comprehensive search of literature published before November 17, 2022 in PubMed, Embase, Cochrane Library, the China National Knowledge Infrastructure (CNKI) database, the Wan Fang database, the Chinese Scientific Journal Databases (VIP) database, and the Chinese Biomedical Literature database (CBM). English search terms and search patterns include: “Rheumatoid”, “Arthritis”, “Rheumatoid arthritis”, “Cervical Spine Instabilities”, “Cervical instability”, “Neck symptom”. Additional studies were also identified by a hand search of all the references of retrieved articles.
Literature screening and quality extraction
All literature was imported into EndNote. Duplicate literature was first removed, and then two researchers (Xiaoling Zhu and Jinhua Shen) independently read the titles and abstracts to eliminate obviously irrelevant literature. Then, the full texts were read, and literature that did not meet the inclusion and exclusion criteria was removed based on the topic. Finally, data were extracted and cross-checked. If there were any disagreements, a third researcher (Jianghong Tan) was consulted to assist in judgment. The extracted data mainly included the title, first author’s name, publication year, study type, study area, sample size, and influencing factors.
Literature quality assessment
The cross-sectional studies included in this study were evaluated for bias risk according to the standards recommended by the Agency for Healthcare Research and Quality (AHRQ). The quality of cohort studies and case-control studies was evaluated using the Newcastle-Ottawa Scale (NOS). The AHRQ evaluation criteria consisted of 11 items, which were evaluated as “yes,” “no,” or “unclear.” One point was given for a “yes” response, and zero points were given for all other responses. A higher score indicated a higher quality of literature [10]. The NOS mainly evaluated the quality of the study in three aspects: selection of the study population, comparability between groups, and measurement of results [11].
Statistical analysis
Meta-analysis was performed using RevMan 5.3 software. The heterogeneity of the study results was tested using the χ2 test, with a significance level of α = 0.1. If significant heterogeneity was found between the studies (p < 0.1, I2 ≥ 50%), a random effects model was used for analysis. Otherwise, a fixed effects model was used for analysis.
Results
Literature selection
A total of 1178 relevant articles were initially identified, including 63 from PubMed, 1081 from Embase, 8 from Cochrane Library, 4 from the CNKI database, 6 from Wanfang Data, 13 from the VIP database, and 3 from CBM. After removing duplicate literature, 731 articles were obtained. A total of 686 articles were excluded based on the title and abstract, and 45 articles were screened by reading the full text. Thirty-one articles were subjected to full-text screening again, and 1 article was cited after reading the literature. Finally, 8 articles were included (Figure 1).
Characteristics and quality assessment of included literature
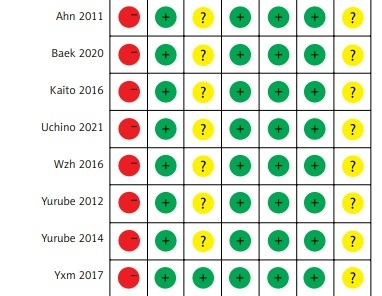
A total of 8 articles [12–19] were included in this study, involving 3078 patients with RA. Five articles had a quality score of ≥ 7, and 3 articles had a score of 5–6. The basic characteristics and quality assessment results of the included literature are shown in Table I. In addition, the graph of risk of bias is shown in Figure 2.
Table I
Basic characteristics and quality evaluation of the included literature
Meta-analysis results
The effect of disease duration on cervical instability in RA
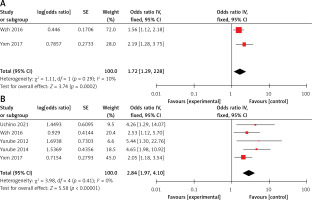
Two articles compared the effect of disease duration on cervical instability in RA. The heterogeneity of the literature was low, with I2 = 10% and p > 0.05. A fixed effects model was used for analysis, and the meta-analysis results showed that patients with longer disease duration had a 1.72 times higher risk of cervical instability than those with shorter disease duration (p < 0.05) (Figure 3 A).
The effect of long-term glucocorticosteroid use on cervical instability in RA
A total of 5 studies on the effect of long-term glucocorticosteroid use were included. The heterogeneity test showed that I2 = 0% and p > 0.05, indicating very low heterogeneity. A fixed effects model was used for analysis, and the meta-analysis results showed that the risk of cervical instability in patients who used glucocorticosteroids for more than 1 year was higher than that in patients who used glucocorticosteroids for less than 1 year, with a statistically significant difference (p < 0.05) (Figure 3 B).
The effect of Steinbrocker stage on cervical instability in RA
Five studies compared the effect of Steinbrocker stage on cervical instability in RA. The heterogeneity of the literature was low, with I2 = 42% and p > 0.05. A fixed effects model was used for analysis, and the meta-analysis results showed that the risk of cervical instability in patients with Steinbrocker stage III or IV was higher than that in patients with Steinbrocker stage I or II, with a statistically significant difference (p < 0.05) (Figure 3 C).
The effect of disability at baseline on cervical instability in RA
Two studies compared the effect of disability at baseline on cervical instability in RA. The heterogeneity between the studies was low, with I2 = 0% and p > 0.05. A fixed effects model was used for analysis. The meta-analysis results showed that the risk of cervical instability in patients with RA who had 3 or more hand joint impairments at baseline was 24.57 times higher than that in patients with less than 3 hand joint impairments at baseline (Figure 3 D).
The effect of peripheral joint destruction on cervical instability in RA
A total of 2 studies were included, and the heterogeneity between the studies was low, with I2 = 0% and p > 0.05. A fixed effects model was used for analysis. The meta-analysis results showed that the risk of cervical instability in patients with peripheral joint destruction was 2.24 times higher than that in patients with normal peripheral joints (Figure 3 E).
The effect of male gender on cervical instability in RA
A total of two studies were included, and the heterogeneity between the studies was low, with I2 = 0% and p > 0.05. A fixed effects model was used for analysis. The meta-analysis results showed that the risk of cervical instability in male patients with RA was 1.7 times higher than that in female patients (Figure 3 F).
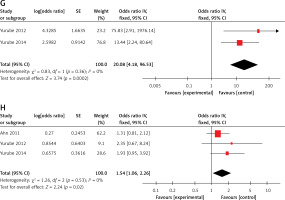
The impact of Steinbrocker stages I–IV on the development of cervical instability leading to disability in RA
Two studies were included with low heterogeneity (I2 = 0%, p > 0.05), and a fixed-effects model was selected for analysis. The meta-analysis results showed that the risk of developing cervical instability leading to disability in patients with Steinbrocker I–IV stages was 20.08 times higher than in those without disability (Figure 3 G).
The impact of previous joint surgery on cervical instability in RA
Three studies were included with low heterogeneity (I2 = 0%, p > 0.05), and a fixed-effects model was selected for analysis. The meta-analysis results showed that patients who had previous joint surgery had a higher risk of developing cervical instability compared to those without joint surgery, and the difference was statistically significant (p < 0.05) (Figure 3 H).
Sensitivity analysis
Random-effects and fixed-effects models were used to calculate the impact factors in this study, and the results were compared. It was found that there was little difference in the results calculated by these two models (95% CI included 1 or did not include 1), indicating that the results were stable and reliable (Table II).
Table II
Sensitivity analysis results of risk factors for cervical instability in RA
Discussion
This study included a total of 8 articles, all of which clearly stated the inclusion and exclusion criteria as well as the diagnostic standards for the study subjects. The included articles were of medium to high quality, and the conclusions were relatively reliable. The comprehensive analysis of this study found that male gender, disease duration, long-term use of steroids, Steinbrocker stage, baseline disability, peripheral joint destruction, development of disability in Steinbrocker stages I–IV, and previous joint surgery were the main risk factors for cervical instability in RA.
Disease duration
RA cervical instability has a high incidence rate and poor prognosis. Multiple studies have shown that RA disease duration is related to cervical instability, and the longer the disease duration, the higher the risk of cervical instability [20, 21]. As the disease duration lengthens, it indicates that the patient’s ligament and bone damage caused by RA become more severe. In addition, the patient’s compliance with treatment may greatly decrease, and once cervical instability occurs due to poor disease control, the surrounding muscles will also undergo pathological changes, further disrupting the cervical dynamic balance and worsening cervical disease [22]. Therefore, for RA patients with a longer disease duration, we should closely monitor their cervical spine, conduct regular X-ray screening, and increase their disease awareness and treatment compliance to delay bone damage.
Long-term glucocorticosteroid use
Glucocorticoids are the cornerstone of treatment for RA patients, but long-term use of glucocorticosteroids (> 1 year) can cause many adverse reactions. Several studies have shown that long-term use of steroids is an independent risk factor for RA cervical instability, which is consistent with the findings of our study [14, 15]. Long-term use of glucocorticosteroids may lead to apoptosis of joint chondrocytes, accelerate bone destruction, and induce cervical instability [23]. Meanwhile, it can accelerate the loss of bone minerals, destruction of bone microstructure, and decrease in bone density, thus accelerating bone damage [24]. In addition, long-term use of glucocorticosteroid without being able to stop the drug may indicate that the disease is not effectively controlled. Long-term inflammation stimulation can accelerate ligament and bone damage and cervical dynamic imbalance, and aggravate cervical instability [13].
Steinbrocker stage and peripheral joint bone destruction
Steinbrocker stage is an imaging classification used to evaluate the severity of RA joints and to classify RA disease stages. Steinbrocker stage III or IV indicates the presence of bone destruction in peripheral joints. This study showed that patients with Steinbrocker stage III or IV have a higher risk of cervical instability than those with Steinbrocker stages I or II, which is consistent with the findings of Yurube et al. and Uchino et al. [14, 16]. Additionally, the study by Wen et al. also showed that peripheral joint bone destruction is the strongest risk factor for RA cervical instability [13]. RA causes destruction of cartilage and bone due to erosive synovitis and neovascularization. The mechanism of cervical spine involvement is similar to that of peripheral joint bone destruction, as both have abundant synovium and greater mobility, making the cervical spine more susceptible to instability. Therefore, in RA patients with peripheral joint bone destruction, the progression and severity of cervical spine involvement will be accelerated [25].
Baseline disability and development of disability in Steinbrocker stages I–IV
Baseline disability refers to the presence of three or more disabled hand joints on bilateral hand X-rays [26]. The results of this study showed that baseline disability is an independent risk factor for cervical instability in RA patients, which is similar to the findings of Yurube [14, 15]. A multivariate analysis showed that the likelihood of developing AAS in patients with peripheral joint damage at 5 years of disease duration was 15.9 times higher than that of patients with peripheral joint damage at 10 years of disease duration, indicating that the progression of cervical instability in RA is closely related to the presence of peripheral joint disability [27]. Additionally, some studies have shown that the development of three or more disabled hand joints in Steinbrocker stages I–IV is the best predictor of cervical instability in RA [15]. Therefore, we should pay close attention to the presence of peripheral joint disability at baseline and changes in peripheral joint disability during the course of RA.
Male gender
The results of this study showed that male RA patients have a 1.7 times higher risk of atlantoaxial subluxation than female patients, which is consistent with the results of some foreign studies [28–30]. This may be related to the fact that the overall Ranawat value (the distance from the anterior and posterior arch line of the atlas to the center of the odontoid process) is higher in males than in females, and decreases with age after the diagnosis of RA. On the other hand, it may also be related to the fact that the definition of vertical subluxation is < 15 mm for males and < 13 mm for females [29].
Previous joint surgery
The results of this study showed that previous joint surgery is an independent risk factor for cervical instability in RA, which is consistent with some foreign studies [19, 31]. Collins et al. [31] found that more than 60% of RA patients undergoing joint replacement surgery had cervical instability on imaging, indicating that the spine, like other joints, is easily affected by the long-term effects of RA, and that patients with cervical instability also have active and destructive inflammation in peripheral joints [19]. At the same time, many studies have shown that RA patients who have undergone previous joint surgery often experience cervical instability, and the progression of cervical spine involvement is also accelerated [32, 33]. Therefore, we should pay close attention to RA patients who have undergone previous joint surgery.
Rehabilitation interventions
There are several rehabilitation interventions that can also have a significant impact on cervical instability in RA. For example, chiropractic care could help by relaxing hypertonic musculature, relieving neural compromise, disrupting periarticular adhesions, and restoring spinal function [34]. Neck exercises improve muscular endurance and strength to keep the head upright. Chiropractic care can relieve atlantoaxial instability [35]. The chiropractic regimen consisted of upper thoracic spine mobilization/adjustment, electrical muscle stimulation of the cervical extensors, home exercises and neck bracing.
In conclusion, there are several limitations to this study. Only two studies were included that focused on male patients, disease duration, baseline disability, peripheral joint damage, and Steinbrocker stages I–IV that lead to disability, which may have influenced the results to some extent. Based on the results of this meta-analysis, it is recommended that healthcare professionals strengthen their assessment and management of high-risk individuals for RA cervical instability, adopt targeted preventive measures, reduce the risk of RA cervical instability, and improve the clinical prognosis of patients. Given the limitations of the literature included in this study, it is recommended that future research continues to include more high-quality, multicenter, large-sample original studies to supplement and validate the findings.