Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
NEUROLOGY / CLINICAL RESEARCH
Risk factors for cerebral hyperperfusion syndrome after carotid revascularization: a meta-analysis involving 158,624 participants
1
Department of Neurosurgery, The University-Town Hospital of Chongqing Medical University, Chongqing, China
These authors had equal contribution to this work
Submission date: 2024-05-11
Final revision date: 2024-08-02
Acceptance date: 2024-08-09
Online publication date: 2024-09-07
Corresponding author
Guojing Liu
Department of Neurosurgery, The University-Town , Hospital of Chongqing Medical University, Chongqing 401331, China
Department of Neurosurgery, The University-Town , Hospital of Chongqing Medical University, Chongqing 401331, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
This study aimed to identify the risk factors associated with cerebral hyperperfusion syndrome (CHS) following carotid revascularization.
Material and methods:
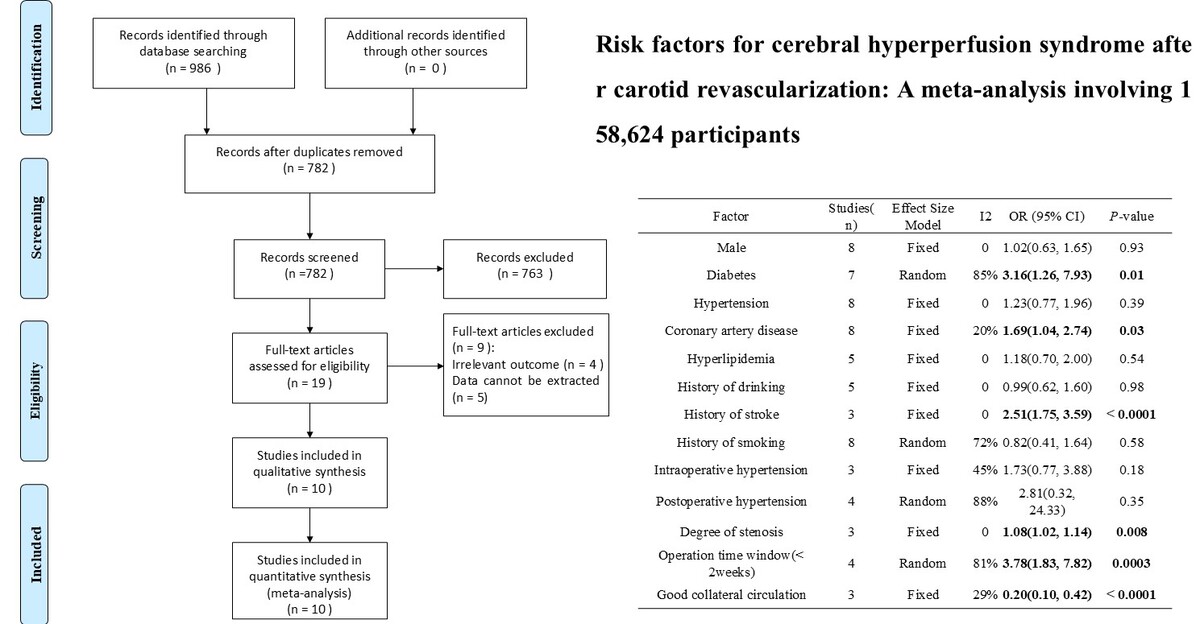
Comprehensive searches of the Cochrane Library, PubMed, Embase, Web of Science, CBM, CNKI, VIP, and Wanfang databases yielded potentially eligible studies published up to April 30, 2024. We conducted a meta-analysis using RevMan 5.3.
Results:
Our analysis incorporated ten studies, encompassing 158,624 participants. The results demonstrated that diabetes (OR = 3.16, 95% CI (1.26, 7.93), p = 0.01), coronary artery disease (OR = 1.69, 95% CI (1.04, 2.74), p = 0.03), a history of stroke (OR = 2.51, 95% CI (1.75, 3.59), p < 0.00001), degree of stenosis (OR = 1.08, 95% CI (1.02, 1.14), p = 0.008), and an operation time window of less than two weeks (OR = 3.78, 95% CI (1.83, 7.82), p = 0.0003) constituted risk factors for CHS following carotid revascularization. Conversely, robust collateral circulation served as a protective factor (OR = 0.20, 95% CI (0.10, 0.42), p < 0.0001). Other factors such as male gender (OR = 1.02, 95% CI (0.63, 1.65), p = 0.93), hypertension (OR = 1.23, 95% CI (0.77, 1.96), p = 0.39), hyperlipidemia (OR = 1.18, 95% CI (0.70, 2.00), p = 0.54), prior alcohol consumption (OR = 0.99, 95% CI (0.62, 1.60), p = 0.98), smoking history (OR = 0.82, 95% CI (0.41, 1.64), p = 0.58), intraoperative hypertension (OR = 1.73, 95% CI (0.77, 3.88), p = 0.18), and postoperative hypertension (OR = 2.81, 95% CI (0.32, 24.33), p = 0.35) showed no significant association with post-revascularization CHS.
Conclusions:
This investigation elucidated the risk and protective factors for CHS after carotid artery revascularization. Further research and clinical application will aid in refining strategies for the prevention and management of CHS.
This study aimed to identify the risk factors associated with cerebral hyperperfusion syndrome (CHS) following carotid revascularization.
Material and methods:
Comprehensive searches of the Cochrane Library, PubMed, Embase, Web of Science, CBM, CNKI, VIP, and Wanfang databases yielded potentially eligible studies published up to April 30, 2024. We conducted a meta-analysis using RevMan 5.3.
Results:
Our analysis incorporated ten studies, encompassing 158,624 participants. The results demonstrated that diabetes (OR = 3.16, 95% CI (1.26, 7.93), p = 0.01), coronary artery disease (OR = 1.69, 95% CI (1.04, 2.74), p = 0.03), a history of stroke (OR = 2.51, 95% CI (1.75, 3.59), p < 0.00001), degree of stenosis (OR = 1.08, 95% CI (1.02, 1.14), p = 0.008), and an operation time window of less than two weeks (OR = 3.78, 95% CI (1.83, 7.82), p = 0.0003) constituted risk factors for CHS following carotid revascularization. Conversely, robust collateral circulation served as a protective factor (OR = 0.20, 95% CI (0.10, 0.42), p < 0.0001). Other factors such as male gender (OR = 1.02, 95% CI (0.63, 1.65), p = 0.93), hypertension (OR = 1.23, 95% CI (0.77, 1.96), p = 0.39), hyperlipidemia (OR = 1.18, 95% CI (0.70, 2.00), p = 0.54), prior alcohol consumption (OR = 0.99, 95% CI (0.62, 1.60), p = 0.98), smoking history (OR = 0.82, 95% CI (0.41, 1.64), p = 0.58), intraoperative hypertension (OR = 1.73, 95% CI (0.77, 3.88), p = 0.18), and postoperative hypertension (OR = 2.81, 95% CI (0.32, 24.33), p = 0.35) showed no significant association with post-revascularization CHS.
Conclusions:
This investigation elucidated the risk and protective factors for CHS after carotid artery revascularization. Further research and clinical application will aid in refining strategies for the prevention and management of CHS.
REFERENCES (41)
1.
Pelz DM, Fox AJ, Spence JD, Lownie SP. Carotid stenosis and stroke: historical perspectives leading to current challenges. Canad J Neurol Sci 2024; 1-6. doi: 10.1017/cjn.2024.40.
2.
Zhang Y, Bai Y, Xie J, et al. Carotid plaque components and other carotid artery features associated with risk of stroke: a systematic review and meta-analysis. J Stroke Cerebrovasc Dis 2022; 31: 106857.
3.
van Dam-Nolen DHK, van Egmond NCM, Koudstaal PJ, van der Lugt A, Bos D. Sex differences in carotid atherosclerosis: a systematic review and meta-analysis. Stroke 2023; 54: 315-26.
4.
Vasavada AM, Singh P, Firdaus A, et al. Carotid endarterectomy versus stenting for the treatment of patients with carotid artery stenosis: an updated systematic review and meta-analysis. Cureus 2023; 15: e35070.
5.
Aggarwal A, Whitler C, Jain A, Patel H, Zughaib M. Carotid artery stenting versus carotid artery endarterectomy in asymptomatic severe carotid stenosis: an updated meta-analysis. Cureus 2023; 15: e50506.
6.
Zhao H, Deng H, Li B, Lei D, Ji Y. Advances in the treatment of carotid atherosclerotic stenosis. J Chengdu Med Coll 2024; 19: 187-92.
7.
Kan X, Wang Y, Xiong B, et al. Carotid artery stenting versus carotid endarterectomy in the treatment of symptomatic and asymptomatic carotid stenosis: a systematic review and meta-analysis. J Interv Med 2018; 1: 42-8.
8.
Müller MD, Lyrer P, Brown MM, Bonati LH. Carotid artery stenting versus endarterectomy for treatment of carotid artery stenosis. Cochrane Database Syst Rev 2020; 2: Cd000515.
9.
Abbott AL, Paraskevas KI, Kakkos SK, et al. Systematic review of guidelines for the management of asymptomatic and symptomatic carotid stenosis. Stroke 2015; 46: 3288-301.
10.
Jiang P, Zhang H, Wang X, Cao F, Li C. A case report of the treatment of carotid artery stenosis by staged angioplasty based on intraoperative TCD monitoring. Heliyon 2024; 10: e30003.
11.
Xu M, Yan P, Zhao Y, Wang H, Sun Q, Du Y. Neurosonological parameters may predict the risk of cerebral hyperperfusion syndrome after carotid artery stenting. World Neurosurg 2024; 187: e77-85.
12.
Funatsu T, Imamura H, Tani S, Adachi H, Adachi H, Sakai N. Cerebral hyperperfusion syndrome after stenting for revascularization of intracranial internal carotid artery dissection. Clin Neurol Neurosurg 2023; 227: 107667.
13.
Fujimura M, Kaneta T, Mugikura S, Shimizu H, Tominaga T. Temporary neurologic deterioration due to cerebral hyperperfusion after superficial temporal artery-middle cerebral artery anastomosis in patients with adult-onset moyamoya disease. Surg Neurol 2007; 67: 273-82.
14.
Shi Z, Wu L, Wang Y, Zhang H, Yang Y, Hang C. Risk factors of postoperative cerebral hyperperfusion syndrome and its relationship with clinical prognosis in adult patients with moyamoya disease. Chin Neurosurg J 2023; 9: 10.
15.
Edwards AM, Birchler CR, Park S, Baker JM, Molnar RG. Cerebral hyperperfusion syndrome presenting as status epilepticus following carotid endarterectomy. Cureus 2021; 13: e20551.
16.
Nemoto S, Maeda T, Yamashita K, et al. Asymptomatic subarachnoid hemorrhage following carotid endarterectomy: illustrative case. J Neurosurg Case Lessons 2023; 6: CASE23476.
17.
Li N, Zhou F, Lu X, et al. Impaired dynamic cerebral autoregulation as a predictor for cerebral hyperperfusion after carotid endarterectomy: a prospective observational study. World Neurosurg 2024; 181: e312-21.
18.
González García A, Moniche F, Escudero-Martínez I, et al. Clinical predictors of hyperperfusion syndrome following carotid stenting: results from a national prospective multicenter study. JACC Cardiovasc Interv 2019; 12: 873-82.
19.
Hsu AC, Williams B, Ding L, Weaver FA, Han SM, Magee GA. Risk factors for cerebral hyperperfusion syndrome following carotid revascularization. Ann Vasc Surg 2023; 97: 89-96.
20.
Li Y, Liu C, Chen Z, Lin H. Analysis of influencing factors of cerebral hyperperfusion syndrome after carotid artery forming and stent implantation. China Health Standard Manag 2020; 11: 52-5.
21.
Ma B, Chen H, Huang J. Risk factors for cerebral hyperperfusion syndrome after stentplacement in symptomatic severe carotid artery stenosis. China Med Engineering 2023; 31: 58-62.
22.
Ni L, Liu C, Cui L, et al. Risk analysis for cerebral hyperperfusion syndrome after carotid endarterectomy. Chinese J Surg 2013; 51: 800-3.
23.
Wang S, Han J, Cheng L, Li N. Risk factors and preventive measures of cerebral hyperperfusion syndrome after carotid artery interventional therapy. Exp Ther Med 2017; 14: 2517-20.
24.
Wang X. Analysis of related factors of cerebral hyperperfusion syndromeafter stenting for internal carotid artery system vascular stenosis [Master] 2019.
25.
Wu J, Ma B, Wu Y, et al. Risk factors and preventive measures of cerebral hyperperfusionsyndrome after carotid angioplasty and stenting. J Clin Radiol 2023; 42: 831-6.
26.
Xia H. Analysis of risk factors for hyperperfusion statefollowing carotid artery stenting [Master] 2020.
27.
Zhang Y. Risk factors for hyperperfusion syndrome following carotid artery stenting [Master ] 2013.
28.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71.
29.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010; 25: 603-5.
30.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21: 1539-58.
31.
Thornton A, Lee P. Publication bias in meta-analysis: its causes and consequences. J Clin Epidemiol 2000; 53: 207-16.
32.
Lin YH, Liu HM. Update on cerebral hyperperfusion syndrome. J Neurointerv Surg 2020; 12: 788-93.
33.
Meyers PM, Higashida RT, Phatouros CC, et al. Cerebral hyperperfusion syndrome after percutaneous transluminal stenting of the craniocervical arteries. Neurosurgery 2000; 47: 335-43.
34.
Nakagawa I, Park H, Kotsugi M, et al. Elective carotid stenting after urgent best medical treatment suppresses recurrent stroke in patients with symptomatic carotid artery severe stenosis. Clin Neurol Neurosurg 2020; 195: 105855.
35.
Farooq MU, Goshgarian C, Min J, Gorelick PB. Pathophysiology and management of reperfusion injury and hyperperfusion syndrome after carotid endarterectomy and carotid artery stenting. Exp Transl Stroke Med 2016; 8: 7.
36.
Newman JE, Bown MJ, Sayers RD, et al. Post-carotid endarterectomy hypertension. part 1: association with pre-operative clinical, imaging, and physiological parameters. Eur J Vasc Endovasc Surg 2017; 54: 551-63.
37.
Vacca VM, Thomas SB. Cerebral hyperperfusion syndrome following carotid artery revascularization. Nurs Crit Care 2017; 12: 32-9.
38.
Meng, Yun, Shang F, Zhou H. Relationship between degree of carotid artery stenosis and reperfusion injury after CAS. Hebei Med 2017; 23: 5.
39.
Meng L, Gelb AW. Regulation of cerebral autoregulation by carbon dioxide. Anesthesiology 2015; 122: 196-205.
40.
Nielsen MY, Sillesen HH, Jørgensen LG, Schroeder TV. The haemodynamic effect of carotid endarterectomy. Eur J Vasc Endovasc Surg 2002; 24: 53-8.
41.
Xu S, Wu P, Shi H, Ji Z, Dai J. Hyperperfusion syndrome after stenting for intracranial artery stenosis. Cell Biochem Biophys 2015; 71: 1537-42.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.