Multiple sclerosis (MS) is caused by an autoimmune process that leads to diffuse demyelination of the central nervous system (CNS) [1]. The symptomatology of MS consists of a variety of signs and symptoms such as weakness and fatigue, spasticity, reduced mobility and ambulation, impaired coordination, depression and sexual dysfunction (SD).
The most commonly proposed theory is that the etiology of MS is related to the complex interaction between genetic predisposition and environmental factors. Some of these factors can be modified, which can influence not only the development of the disease but also the progression of the disability and prognosis of the treatment outcomes. One of the recently underlined factors is impaired sexual functioning. The disease most commonly affects young adults, and hence those who are sexually active.
According to the World Health Organization (WHO), sexual dysfunction (SD) is a syndrome that includes at least one of the following symptoms: loss of sexual desire, sexual aversion and lack of sexual pleasure, lack of genital response (erectile dysfunction in men and vaginal dryness or lack of lubrication in women), orgasmic dysfunction, premature ejaculation, vaginismus and dyspareunia [2].
Numerous neurological/mental disorders decrease the quality of sexual life and lead to sexual dysfunction [3]. Approximately one-third of young and middle-aged chronically medicated male patients with schizophrenia suffer from SD [4]. Major depression is associated with erectile dysfunction in male sufferers [5]. A newly recognized mental disorder with a neurological basis called misophonia significantly decreases the quality of sexual life and leads to SD in sufferers of both sexes and their partners [6].
It is believed that SD in MS patients is associated with three groups of factors: neurological changes directly resulting from the disease (demyelination and atrophy of the nerve fiber involved in transmitting signals related to sexual reactivity), chronic fatigue, and physical disability (secondary factors) and psychological and socio-cultural aspects of chronic disease (tertiary factors) [7].
The study presents a discussion of intimacy and sexuality, and explores the ways MS can affect one’s sexual life, which is still very important.
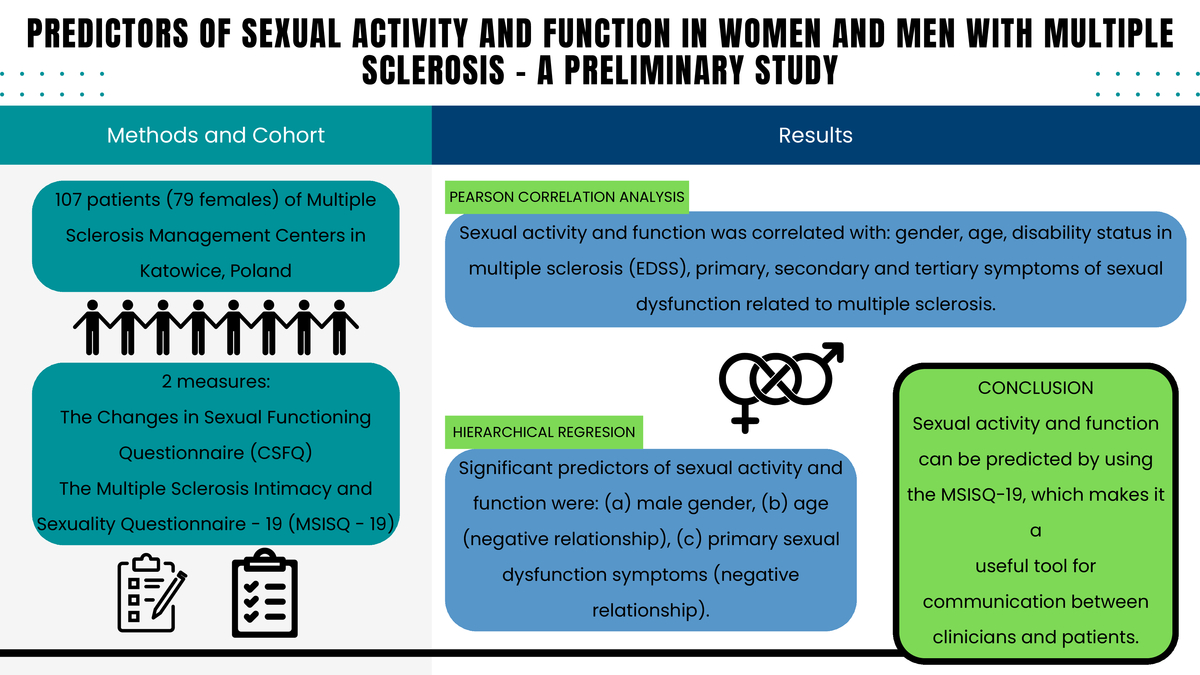
The present preliminary study aimed to assess among patients with MS the relationship between sexual activity and function (explained variable) and such predictors as gender, age, disability status in multiple sclerosis, and symptoms of sexual dysfunction related to multiple sclerosis. It was predicted that significant predictors of sexual activity and function among patients with MS would be gender (men will function better), age (negative relationship), disability status in MS (negative relationship) and symptoms of sexual dysfunction related to the disease (negative relationship).
Material and methods
Participants and procedure
In total, 134 patients (99 females/35 males who were consecutively admitted to Multiple Sclerosis Management Centers in Katowice, Poland between 2022 and 2024) were recruited for the study. Participants who had not experienced an exacerbation within the past 30 days and had no medical conditions, such as cardiac diseases, endocrine disorders, musculoskeletal system diseases, current glucocorticoid therapy, or respiratory diseases, were included. Patients who met the inclusion criteria were included in the final study group (N = 107, 79 females/28 males). All the patients had a definite diagnosis of relapsing-remitting or secondary progressive MS [8] and preservation of at least some ambulatory function (Expanded Disability Status Scale (EDSS) 1.0–7.0, with a median score of 2.0) [9].
The group was racially homogeneous. All participants included in the study were Caucasian. All resided in the Silesian province, most in the Upper Silesia region.
Measures
The Changes in Sexual Functioning Questionnaire (CSFQ)
This measure was used to assess sexual activity and function [10]. A Polish version of the instrument was previously translated (forward-backward method). Previous studies demonstrated its adequate reliability and validity [11, 12]. It consists of 14 items to which participants respond on a 5-point scale that varies depending on the question (e.g. Compared with the most enjoyable it has ever been, how enjoyable or pleasurable is your sexual life right now? 1 – no enjoyment or pleasure, 2 – little enjoyment or pleasure, 3 – some enjoyment or pleasure, 4 – much enjoyment or pleasure, 5 – great enjoyment or pleasure). It includes 5 subscales (pleasure, desire/frequency, desire/interest, arousal/excitement, orgasm/completion) and a total score. The range (min.–max.) of the total score for the CSFQ is 14-70. A CSFQ score of ≤ 41 for women and ≤ 47 for men indicates sexual problems. The higher the result obtained by the participant, the better he/she functions in terms of sexual activity and function. In our analysis Cronbach’s α coefficient (internal consistency) was (no results for the pleasure subscale, which consists of 1 item): (a) total score: 0.89, (b) desire/frequency: 0.74, (c) desire/interest: 0.72, (d) arousal/excitement: 0.75, (e) orgasm/completion: 0.77.
The Multiple Sclerosis Intimacy and Sexuality Questionnaire-19 (MSISQ-19)
This measure was used to assess symptoms of sexual dysfunction related to multiple sclerosis [13]. It was only used in a clinical sample. It consists of 19 items to which participants respond on a 5-point scale (from 1 – never to 5 – always) assessing the last 6 months (item example: Pain, burning, or discomfort in my body). It includes 3 subscales: primary, secondary, tertiary. The primary and tertiary subscales of sexual dysfunction consist of 5 items each. The secondary sexual dysfunction subscale consists of 9 items. The range (min.–-max) of the total MSISQ-19 score is 19–95. An MSISQ-19 score of > 30 or a score above 3 on any MSISQ-19 item indicates sexual problems. The higher the result, the higher are the levels of symptoms of sexual dysfunction related to MS. In our analysis Cronbach’s α coefficient (internal consistency) was: (a) primary: 0.85, (b) secondary: 0.88, (c) tertiary: 0.86.
The Expanded Disability Status Scale (EDSS)
The assessment of neurological status of MS patients was based on the Expanded Disability Status Scale (EDSS) [9] and was performed by an experienced and neurostatus.net-certified neurologist (EM). The scale ranges from 0.0 (normal neurological status) to 10.0 (death due to MS), increasing in half-point increments. From grade 4.5 the patient’s mobility is limited, and at grade 5.0 daily activities are limited. A score of 9.0 indicates a patient who is bedridden. Due to the nature of the scale, standard reliability coefficients such as Cronbach’s α cannot be calculated for it.
Statistical analysis
IBM SPSS Statistics 29 was used for statistical analysis. Hierarchical regression was used to verify the second hypothesis related to assessment of predictors in the field of sexual activity and function among patients with MS. The main assumptions related to multiple regression models have been met. Variance inflation factors did not exceed 10 and tolerance was higher than 0.2. In the regression model, sexual activity and function (total score) was a criterion variable. As a first step, we entered gender and age. As a second step, we entered disability status in multiple sclerosis, and, as a third step, we entered symptoms of sexual dysfunction related to multiple sclerosis (three dimensions categorized as primary, secondary, and tertiary symptoms of sexual dysfunction). In this way, it was possible to examine the extent to which disability status in multiple sclerosis and symptoms of sexual dysfunction related to multiple sclerosis incrementally predicted sexual activity and function, after accounting for variance associated with the other variables (gender and age).
Results
Preliminary analysis: Pearson correlation analysis
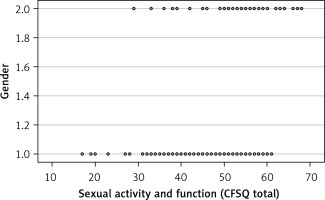
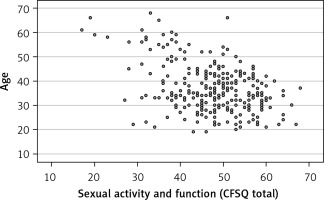
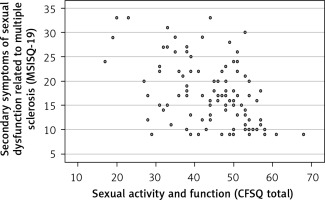
As preliminary analyses for the regression model, Pearson correlation analysis was performed (Table I). The analysis results indicate that all predictors were significantly associated (and in the expected direction) with the explained variable (sexual activity and function). This is proven by the following results regarding the relationship between sexual activity and function and (the confirming data): (a) gender: r = 0.28, p < 0.01 (positive relationship which means male gender according to gender coding according to dichotomous variable – women (1) and men (2)), (b) age: r = –0.51, p < 0.001 (negative relationship), (c) disability status in multiple sclerosis: r = –0.46, p < 0.001 (negative relationship), (d) primary symptoms of sexual dysfunction related to multiple sclerosis: r = –0.57, p < 0.001 (negative relationship), (e) secondary symptoms of sexual dysfunction related to multiple sclerosis: r = –0.46, p < 0.001 (negative relationship), (f) tertiary symptoms of sexual dysfunction related to multiple sclerosis: r = –0.42, p < 0.001 (negative relationship). Figures 1–6 present the obtained relationships.
Table I
Correlation analysis (Pearson’s r)
| Parameter | Gender | Age | Disability status in multiple sclerosis (EDSS) | Primary symptoms of sexual dysfunction related to multiple sclerosis | Secondary symptoms of sexual dysfunction related to multiple sclerosis | Tertiary symptoms of sexual dysfunction related to multiple sclerosis |
|---|---|---|---|---|---|---|
| Sexual activity and function (total score) | 0.28** | –0.51*** | –0.46*** | –0.57*** | –0.46*** | –0.42*** |
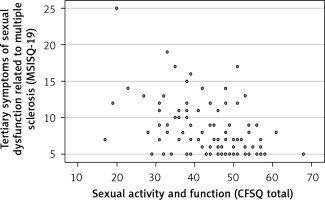
Figure 3
Relationships between sexual activity and function and disability status in multiple sclerosis
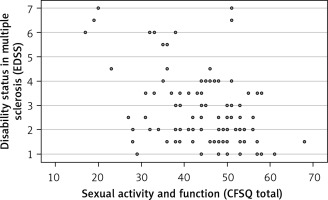
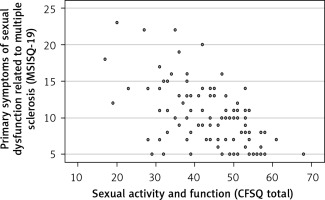
Figure 4
Relationships between sexual activity and function and primary symptoms of sexual dysfunction related to multiple sclerosis
Regression analyses
The regression analyses results are shown in Table II. Hierarchical regression was used to evaluate whether variables of interest explain a statistically significant amount of variance (symptoms of sexual dysfunction related to multiple sclerosis) in the dependent variable (sexual activity and function) after accounting for all other variables. The analyzed model (taking into account 6 predictors) turned out to be statistically significant, F(6, 106) = 14.66, p < 0.001, Adj. R2 = 0.44, ΔFp < 0.001.
Table II
Results of hierarchical regression analysis for sexual activity and function
Finally, the significant predictors of sexual activity and function were: (a) male gender: β = 0.20, p < 0.01, (b) age: β = –0.31, p < 0.01 (negative relationship), and (c) primary sexual dysfunction symptoms: β = –0.42, p < 0.001 (negative relationship). This means that with regard to the relationships in the regression model, it turns out that the increasing level of sexual activity and function can be predicted on the basis of male gender, a decrease in the level of age, and a decrease in the level of the primary symptoms of sexual dysfunction related to multiple sclerosis. Importantly, after running the subscales of the MSISQ-19 questionnaire in the regression model (step 3), the assessment of disability based on EDSS (β = –0.06, p > 0.05) was no longer a significant predictor.
Discussion
The aim of our study was to assess among patients with MS the relationship between sexual activity and function (explained variable) and such predictors as gender, age, disability status in multiple sclerosis, and symptoms of sexual dysfunction related to multiple sclerosis.
Sexual dysfunction is one of the most frequent disorders in multiple sclerosis patients, but at the same time, it is often underdiagnosed and undertreated [14]. The most popular tool for assessment of the neurological state in MS is the Expanded Disability Status Scale [9]. Its novel version, provided by Neurostatus.net – a platform for training and certification of physicians – contains only one question about sexual dysfunction, included in the “Bowel and Bladder Functions” section. In addition, the question is marked as “optional” due to “obvious difficulties in assessment by the examining physician”. Many of the neurologists in fact do not ask patients about SD at all. In a medical center in Austria, only 15% of neurologists reported discussing sexuality with every MS patient [15]. Tudor et al. tried to identify different barriers to seeking help for sexual dysfunction in MS. The commonest were the dominance of neurological symptoms, the presence of family or friends and not being asked [16]. In the UK, in 2018, a project called Pelvic Health Clinic was established to cope with the problem. The clinic provided a monthly service to see patients who had been identified by the MS team as having ‘pelvic health’ needs. Patients were given advice and counselling on contraception, menopause, and sexual problems. The project was highly valued by both clinicians and patients [17]. Another issue is the fact that not all patients are even aware of the impact of the disease on their sexual lives. Foley and Beier proved that access to information materials on sexual disorders in MS caused a significant improvement in the self-assessment of sexual life by patients who used these materials [18]. All these actions seem to be a good approach to creating an effective solution for MS patients with SD. But until the actions are introduced, it is crucial to use an effective screening test to identify the group that needs help. In our study, we used the Multiple Sclerosis Intimacy and Sexuality Questionnaire-19 (MSISQ-19). By analyzing our data, we aimed to check its effectiveness and suitability.
To assess the general sexual function in patients with MS we chose the Changes in Sexual Functioning Questionnaire – a tool developed in 1997. It allows one to assess not only the current state but also how it changed with time, which is, as we believe, suitable for a progressive disease. According to our investigation, it had been used in a group of MS patients only once, in a study by Petersen et al., assessing the differences in sexual disorders in patients with MS and with epilepsy [19]. Subsequently, it was widely used in the domain of sexology in combination with psychiatry and gynecology [10, 11].
In our analysis, we discovered that sexual activity and function (measured by CSFQ) in MS is correlated with gender, age, EDSS, and all the subscales of MSISQ-19. Many studies emphasize the difference between men’s and women’s sexual problems. Lew-Starowicz et al. found a strong influence of decreased desire on sexual quality of life in women and no such correlation in men [20]. A direct comparison was made by Turkish researchers in 2013 and it showed that women had significantly higher (worse) total scores of MSISQ-19 than men [21]. However, Marck et al. in their study did not find any gender differences in satisfaction with sexual function [7]. An age-related decline in sexual function is a common problem in both healthy and unhealthy individuals [22]. In our study sexual function was worse in older patients, which corresponds with the thesis. In research by Romano et al., MS patients were divided into three groups: ‘young adult’, ‘middle adult’, and ‘mature adult’. It was confirmed that with age more and more sexual dysfunctions were present [23]. According to the data found in the literature, the prediction of SD using EDSS is uncertain. Domingo et al. described a correlation between MS-related disability and SD [24]. On the other hand, Dobrakowski et al. found no association between EDSS score and SD [25].
Regression analysis showed that ultimately an increasing level of sexual activity and function can be predicted based on gender (men), a decrease in the level of age, as well as a decrease in the level of primary sexual dysfunction symptoms related to MS (but not based on disability status in multiple sclerosis or secondary and tertiary sexual dysfunction symptoms related to MS). These results are therefore partially consistent with the second hypothesis of our study and confirm the predictions regarding gender, age (negative relationship), and symptoms of sexual dysfunction, but in the scope of only one subscale named “primary” (negative relationship). A very interesting observation is that in the hierarchical regression, at the moment of adding the MSISQ-19 to the analysis, the EDSS score lost its importance. This suggests that the MSISQ-19 is a better predictor of sexual dysfunctions than the EDSS.
Limitations: The limitations of this study must be acknowledged. Firstly, in all subscales of the CSFQ, the internal consistency, described by Cronbach’s α coefficient, was below 0.8 (0.72–0.77). The result meets the basic criteria; however, a possible limited reliability must be taken into account. Secondly, in our study, we did not collect data about medication, e.g. anti-depressants, which can also affect sexual function.
In conclusion, male gender may predispose to better functioning in the context of sexual functioning among MS patients. In contrast, increases in age, disability status (EDSS), and MSISQ-19 score predispose to more disturbed sexual activity and function. The MSISQ-19 is a useful tool for the prediction of sexual disturbances: it provides more complex information about SD than the EDSS score alone. MSISQ-19 can be used by clinicians as a screening test, with the aim of identifying the target group and initiating adequate help and treatment.