Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
NEUROLOGY / CLINICAL RESEARCH
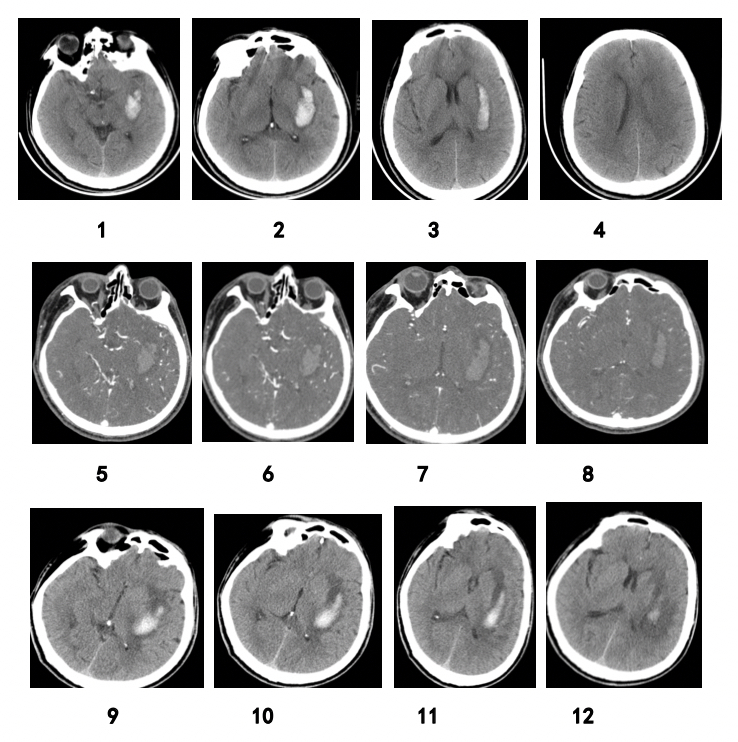
Predictive value of imaging manifestations of supratentorial hemorrhage in hematoma enlargement and clinical prognosis
1
Department of Neurology, Shanghai Pudong New Area People’s Hospital, Shanghai, China
2
Department of Neurology, Shanghai Seventh People’s Hospital, Shanghai, China
3
Department of Neurosurgery, Shanghai Public Health Clinic Center, Shanghai, China
4
Department of Neurosurgery, Shanghai Pudong New Area People’s Hospital, Shanghai, China
Submission date: 2023-03-15
Final revision date: 2023-05-03
Acceptance date: 2023-05-08
Online publication date: 2023-06-03
Corresponding author
Zheng Ping
Department of Radiography Shanghai Pudong New Area People’s Hospital 490, Chuanhuan Nan Rd Shanghai 201299, China
Department of Radiography Shanghai Pudong New Area People’s Hospital 490, Chuanhuan Nan Rd Shanghai 201299, China
KEYWORDS
cerebral angiographycerebral hemorrhagesensitivity and specificityhematomacomputed tomography angiographytomographyX-ray computed
TOPICS
ABSTRACT
Introduction:
Intracerebral hemorrhage (ICH) is an important cause of death and disability. This study aimed to explore the imaging indicators identifying hematoma expansion in primary ICH and to provide a basis for its clinical treatment.
Material and methods:
Hematoma expansion was evaluated by plain computed tomography (CT) scan and multi-detector-row CT angiography (MDCTA).
Results:
This study included a total of 203 patients with intracerebral hemorrhage. The size of the hematoma at the time of admission was 32.5–92.3 ml (mean: 45.5 ml). Original or reconstructed MDCTA images with contrast extravasation were available in 35 (17.2%) cases. Patients were divided into two groups based on whether or not hematoma expansion had occurred: the hematoma expansion group (n = 87) and the no hematoma expansion group (n = 116). Percentages of patients with spot signs in the two groups were 37.93% and 3.45%, respectively, and percentages of those with spot sign ± blend sign ± black hole sign ± island sign (%) were 48.30% and 1.72%, respectively, with statistically significant differences. The sensitivity, specificity, and positive and negative predictive values of hematoma enlargement were 37.93%, 98.27%, and 94.29% and 67.86%, respectively. The sensitivity, specificity, and positive and negative predictive values of blend density sign ± irregular sign in predicting hematoma enlargement in ICH patients were 97.7%, 76.7%, and 75.9% and 97.8%, respectively.
Conclusions:
Blend density sign ± irregular sign can be used as substitute signs. The more irregular and uneven density the hematoma, the more likely it is that the hematoma will be enlarged.
Intracerebral hemorrhage (ICH) is an important cause of death and disability. This study aimed to explore the imaging indicators identifying hematoma expansion in primary ICH and to provide a basis for its clinical treatment.
Material and methods:
Hematoma expansion was evaluated by plain computed tomography (CT) scan and multi-detector-row CT angiography (MDCTA).
Results:
This study included a total of 203 patients with intracerebral hemorrhage. The size of the hematoma at the time of admission was 32.5–92.3 ml (mean: 45.5 ml). Original or reconstructed MDCTA images with contrast extravasation were available in 35 (17.2%) cases. Patients were divided into two groups based on whether or not hematoma expansion had occurred: the hematoma expansion group (n = 87) and the no hematoma expansion group (n = 116). Percentages of patients with spot signs in the two groups were 37.93% and 3.45%, respectively, and percentages of those with spot sign ± blend sign ± black hole sign ± island sign (%) were 48.30% and 1.72%, respectively, with statistically significant differences. The sensitivity, specificity, and positive and negative predictive values of hematoma enlargement were 37.93%, 98.27%, and 94.29% and 67.86%, respectively. The sensitivity, specificity, and positive and negative predictive values of blend density sign ± irregular sign in predicting hematoma enlargement in ICH patients were 97.7%, 76.7%, and 75.9% and 97.8%, respectively.
Conclusions:
Blend density sign ± irregular sign can be used as substitute signs. The more irregular and uneven density the hematoma, the more likely it is that the hematoma will be enlarged.
REFERENCES (27)
1.
Khan NA, McAlister FA, Pilote L, et al. Temporal trends in stroke incidence in South Asian, Chinese and white patients: a population based analysis. PLoS One 2017; 12: e0175556.
2.
Chaturvedi S, Greenberg SM. Intracerebral hematoma expansion: making predictions (about the future). Neurology 2011; 76: 1204-5.
3.
Xie N, Li X, Zhong Q, et al. Association of systolic blood pressure and pulse pressure with microalbuminuria in treatment-naïve hypertensive patients. Arch Med Sci 2019; 15: 832-6.
4.
Li N, Wang Y, Wang W, et al. Contrast extravasation on computed tomography angiography predicts clinical outcome in primary intracerebral hemorrhage: a prospective study of 139 cases. Stroke 2011; 42: 3441-6.
5.
Cao Z, Li S, Yang H, et al. Associations of behaviors, biological phenotypes and cardiovascular health with risks of stroke and stroke subtypes: a prospective cohort study. Eclinicalmedicine 2021; 33: 100791.
6.
Ljubisavljevic S, Ignjatovic A, Ljubisavljevic M. Headache secondary to nontraumatic brain hemorrhage: a single-center, retrospective clinical study. Arch Med Sci 2019; 19: 1028-36.
7.
Morotti A, Li Q, Mazzoleni V, et al. Non-contrast CT markers of intracerebral hemorrhage expansion: the influence of onset-to-CT time. Int J Stroke 2023; 18; 704-11.
8.
Zimmer S, Meier J, Minnerup J, et al. Prognostic value of non-contrast CT markers and spot sign for outcome prediction in patients with intracerebral hemorrhage under oral anticoagulation. J Clin Med 2020; 9: 1077.
9.
de Berker H, de Berker A, Aung H, et al. 265 Use of support vector machine to predict discharge destination on an acute stroke ward. J Neurol Neurosurg Psychiatry 2022; 93: A90.
10.
Odderson IR. The National Institutes of Health Stroke Scale and its importance in acute stroke management. Phys Med Rehabil Clin N Am 1999; 10: 787-800.
11.
Almandoz JED, Yoo AJ, Stone MJ, et al. Systematic characterization of the computed tomography angiography spot sign in primary intracerebral hemorrhage identifies patients at highest risk for hematoma expansion: the spot sign score. Stroke 2009; 40: 2994-3000.
12.
Divani AA, Majidi S, Luo X, et al. The ABCs of accurate volumetric measurement of cerebral hematoma. Stroke 2011; 42: 1569-74.
13.
Arba F, Rinaldi C, Boulouis G, et al. Noncontrast computed tomography markers of cerebral hemorrhage expansion: diagnostic accuracy meta-analysis. Int J Stroke 2021; 17: 17474930211061640.
14.
Boulouis G, Morotti A, Charidimou A, et al. Noncontrast computed tomography markers of intracerebral hemorrhage expansion. Stroke 2017; 48: 1120-5.
15.
Sporns PB, Schwake M, Schmidt R, et al. Computed tomographic blend sign is associated with computed tomographic angiography spot sign and predicts secondary neurological deterioration after intracerebral hemorrhage. Stroke 2018; 48: 131-5.
16.
Orito K, Hirohata M, Nakamura Y, et al. Leakage sign for primary intracerebral hemorrhage: a novel predictor of hematoma growth. Stroke 2016; 47: 958-63.
17.
Group TE. EuroQol – a new facility for the measurement of health-related quality of life. Health Policy 1990; 16: 199-208.
18.
Qingke B, Ping Z, Jianying Z, et al. Clinical comparison of intravenous thrombolysis and bridging artery thrombectomy in hyperacute ischemic stroke with unknown time of onset. Arch Med Sci 2021; 17: 1804-10.
19.
Ping Z, Huiyu S, Min L, et al. Explainable machine learning for long-term outcome prediction in two-center stroke patients after intravenous thrombolysis. Front Neurosci 2023; 17: 1146197.
20.
Hutanu A, Iancu M, Dobreanu M, et al. Extended lipid profile in Romanian ischemic stroke patients in relation to stroke severity and outcome: a path analysis model. Arch Med Sci 2021; 17: 864-73.
21.
Zeng J, Zheng P, Xu J, et al. Prediction of motor function by diffusion tensor tractography in patients with basal ganglion haemorrhage. Arch Med Sci 2011; 7: 310-4.
22.
Ping Z, Min L, Qiuyun L, et al. Prognostic nomogram for the outcomes in acute stroke patients with intravenous thrombolysis. Front Neurosci 2022; 16: 1017883.
23.
Cabañero-Martínez MJ, Cabrero-García J, Richart-Martínez M, et al. The Spanish versions of the Barthel index (BI) and the Katz index (KI) of activities of daily living (ADL): a structured review. Arch Gerontol Geriat 2009; 49: e77-84.
24.
Liu J, Xu H, Chen Q, et al. Prediction of hematoma expansion in spontaneous intracerebral hemorrhage using support vector machine. Ebiomedicine 2019; 43: 454-9.
25.
Wu TC, Liu YL, Chen JH, et al. The added value of intraventricular hemorrhage on the radiomics analysis for the prediction of hematoma expansion of spontaneous intracerebral hemorrhage. Diagnostics 2022; 12: 2755.
26.
Huang YW, Huang HL, Li ZP, et al. Research advances in imaging markers for predicting hematoma expansion in intracerebral hemorrhage: a narrative review. Front Neurol 2023; 14: 1176390.
27.
He GN, Guo HZ, Han X, et al. Comparison of CT black hole sign and other CT features in predicting hematoma expansion in patients with ICH. J Neurol 2018; 265: 1883-90.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.