The outbreak of COVID-19 caused by the coronavirus SARS-CoV-2 has become a pandemic threat that affects the healthcare system globally. Effective treatments against SARS-CoV-2 are urgently needed. To date, there is no proven therapy for mild COVID-19. As new drug development usually takes several years, repurposing clinically approved drugs has been adopted as the strategy to respond immediately to emerging infectious diseases [1, 2]. Many FDA-approved medicines and natural product-based medicines have been screened for anti-SARS-CoV-2 activity, and some have been shown to possess potential activity against SARS-CoV-2 [3–6]. Remdesivir is the only antiviral repurposed drug that has been registered by the US FDA for moderate to severe COVID-19. Dexamethasone, tocilizumab and sarilumab are anti-inflammatory repurposed drugs recommended by the World Health Organization (WHO) for severe COVID-19. The IL-6 receptor blockers tocilizumab and sarilumab are monoclonal antibodies approved for use in rheumatoid arthritis. The continued use of some high potential repurposed drugs, such as hydroxychloroquine, chloroquine, and azithromycin, has been discouraged as accumulated evidence from research did not support their clinical uses against COVID-19 [7]. There are several more potential drugs that are still under investigation at different stages of disease severity (Figure 1) [7, 8].
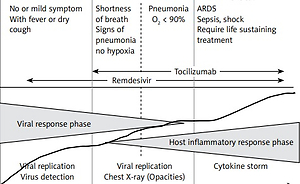
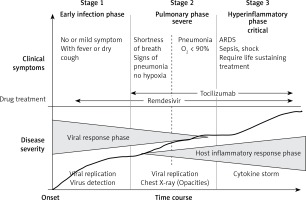
Figure 1
COVID-19 disease staging and treatment. The figure illustrates three clinical stages: early infection, severe (pulmonary phase) and critical stage, phase-specific drugs, and the progress of the disease (adapted from [7] and [8])
This article describes clinically significant research on drugs repurposed for COVID-19 treatment. The information may assist in the decision to use, discontinue, or further develop these drugs. Six widely used repurposed drugs with controversial reports on clinical effectiveness, i.e., remdesivir, ivermectin, favipiravir, azithromycin, tocilizumab, and andrographolide, were selected for discussion. The articles were searched from PubMed and Science Direct databases using the following keywords: “repurposed drugs”, AND “COVID-19” AND “remdesivir”, OR “ivermectin”, OR “favipiravir” OR “ azithromycin” OR “tocilizumab” OR “andrographolide”. The search was performed until July 2022.
Remdesivir by Gilead Science (Veklury). Remdesivir was originally developed to treat hepatitis C and subsequently repurposed for SARS-CoV-2. Remdesivir is a prodrug that is metabolized to an active triphosphate form to inhibit viral RNA synthesis. In vitro and in vivo data support the activity of remdesivir against SARS-CoV-2 and thus support its further evaluation as a potential therapeutic drug for repurposing against COVID-19 [5]. Several randomized clinical trials (RCTs) have been conducted in patients with COVID-19 [9–13]. It was successfully approved by the US FDA in October 2020 for clinical use in adults and pediatric patients (12 years of age and older) with COVID-19, including hospitalized patients with moderate to severe symptoms. The approval of remdesivir (Veklury) by the US FDA was based on three randomized, controlled trials, i.e., ACTT-1 [9], SIMPLE Moderate COVID-19 [10], and SIMPLE Severe COVID-19 [11, 12]. ACTT-1 was a randomized, double-blind, placebo-controlled trial involving 1,062 hospitalized patients in the US, Europe, and Asia. The primary endpoint parameter of this study was the time to recover from the disease. The results showed that remdesivir significantly reduced the time to recovery compared with placebo (mean: 10 vs. 15 days, rate ratio for recovery 1.29 (95% CI: 1.12–1.49, p < 0.001). SIMPLE Moderate COVID-19 was a phase III, multinational, randomized open-label trial involving 584 patients with moderate disease conducted at more than 180 trial sites around the world. It was demonstrated that the patients in the 5-day remdesivir group had significant clinical status distribution on day 11 compared with those receiving standard care (odds ratio (OR) = 1.65 (95% CI: 1.09–2.48), p = 0.02). SIMPLE Severe COVID-19 was a phase III open randomized, controlled trial involving 397 severe COVID-19 patients. It was found that the treatment for 5 or 10 days had similar clinical benefits (time to achieve clinical improvement and duration of hospitalization). Currently, remdesivir is widely used in many countries, with guidelines recommending its use in patients with severe or critical COVID-19 [13, 14]. A retrospective, single-center, case-control study was conducted in Italy in 192 hospitalized patients with confirmed SARS-CoV-2 infection to evaluate the impact of remdesivir on intensive care unit (ICU) admission, the need for orotracheal intubation, and in-hospital mortality [15]. Remdesivir was given at the dose of 200 mg/day 1 as a loading dose, followed by 100 mg once daily for the subsequent 4 days as maintenance dose. No impact of remdesivir in these groups of patients was found. In a retrospective analysis of clinical efficacy in Spain, remdesivir was shown to reduce mortality in very old patients (≥ 80 years, 4,331 cases) hospitalized with COVID-19 [16]. A nationwide, registry-based study including all Italian hospitalized patients with COVID-19 treated with remdesivir (16,462 cases) was performed to assess the impact of major confounders on crude 15-day and 29-day mortality [17]. The results suggest that mortality in SARS-CoV-2 hospitalized patients is substantially influenced by the days between SARS-CoV-2 diagnosis and drug prescription. The network meta-analysis involving six studies was performed to assess the efficacy of remdesivir in hospitalized patients with COVID-19 requiring supplemental oxygen. Among patients requiring supplemental oxygen at baseline, the use of remdesivir compared to best supportive care improved the risk of mortality, recovery, and need for oxygen support in patients receiving oxygen at any flow or low flow [18].
The WHO made a conditional recommendation against administering remdesivir in addition to usual care in hospitalized patients with COVID-19 infection, regardless of disease severity [7]. The WHO decision was based on four RCTs and the report of a living systematic review on drug treatment for COVID-19 [13, 14, 19, 20]. It was concluded that the evidence to support the efficacy of remdesivir for reduction of mortality, the need for mechanical ventilation, time to clinical improvement, duration of hospitalization and viral clearance is insufficient and more evidence from clinical trials is needed, especially in specific subgroups of patients, i.e., children, older adults, and pregnant women. Although there was no evidence of increased risk of severe adverse events from the trials, further pharmacovigilance is needed. Solid evidence should be provided to support the critical outcome parameters that impact matter the patients, particularly with a relatively high cost of the drug and availability in only the intravenous formulation, which requires administration in hospital settings. Furthermore, remdesivir is contraindicated in those with liver or renal dysfunction. Although remdesivir has already been registered by the US FDA for COVID-19, Gilead Science continues to conduct more studies, including those in children, older adults, and pregnant women. Furthermore, a new formulation (an aerosolized solution) was developed and tested in mild cases of COVID-19 (study ID NCT04539262) [21]. Apart from remdesivir monotherapy, several ongoing clinical trials are exploring the potential of combining remdesivir with other repurposed drugs for COVID-19 treatment by targeting multiple targets of the virus and human host simultaneously. The most promising combination is remdesivir–baricitinib [22]. The mortality rate was lower and disease recovery was found to be 8 days shorter compared to remdesivir treatment alone. This combination may be helpful in moderate and severe SARS-CoV-2 infection with or without ventilation but not in severe COVID-19 patients. It was proposed that remdesivir–baricitinib should be given to patients in the early stage of SARS-CoV-2 infection to support fast recovery, stop further disease progression, and control mortality. In addition, the remdesivir–baricitinib combination at a very low dose may have a role in COVID-19 prophylaxis in suspected cases including asymptomatic and pre-symptomatic cases. The combination of remdesivir and interferon β-1b also appears effective for COVID-19 treatment. A multicenter, prospective open-label, randomized-controlled trial was conducted in high-risk adults hospitalized for COVID-19 [23]. Early treatment with interferon β-1b (16 million units daily for 5 days) and remdesivir (200 mg loading on day 1, followed by 100 mg daily dose for 4 days) was safe and better than remdesivir only in alleviating symptoms, shortening viral shedding and hospitalization with earlier seropositivity in high-risk patients.
Ivermectin by Merck (Vermectin). Ivermectin is another repurposed drug that has gained much international attention in the last several months. Ivermectin is currently available globally for parasitic infections, e.g., onchocerciasis (river blindness), strongyloidiasis, ascariasis, and scabies. It has been used widely for decades and is included in the WHO Essential Medicine List. The antiviral activity of ivermectin against SARS-CoV-2 was confirmed in vitro [5]. Information from the systematic review and meta-analysis suggests the role of ivermectin in the prevention and treatment of COVID-19 infection [24]. Ivermectin has a good safety profile, and in addition a low cost of treatment (100 times lower than the newer drugs). In addition, ivermectin is readily available in most countries, especially in low to middle-income countries where access to the more recent and expensive drugs may not be feasible.
The meta-analysis was based on information from 15 trials with 2,438 patients (databases up to April 25, 2021). Ivermectin was shown to reduce the risk of death by an average of 0.62 (95% CI: 0.27–0.81) compared with the control (no ivermectin) with a relative risk (RR) of 0.38 (95% CI: 0.19–0.73), and risk of death of 2.3% vs. 7.8% among the hospitalized patients. The quality of evidence was rated as moderate certainty. In addition, a meta-analysis of ivermectin prophylaxis was carried out in 3 trials involving 738 participants. Ivermectin prophylaxis among health care workers and COVID-19 contacts was shown to reduce the risk of infection by 86% (79–91%), with a RR of 0.14 (95% CI: 0.09–0.21). The quality of evidence was rated as low certainty due to limitations in the study design and the number of trials included in the analysis (3 trials). In terms of safety, a meta-analysis of 11 trials was performed with a total number of 1,533 participants. No significant difference between ivermectin and the control was found regarding the risk of severe adverse events (RR = 1.65, 95% CI: 0.44–6.09). The quality of evidence was rated as insufficient certainty. The secondary outcome parameters, such as the need for mechanical ventilation, provided less certain evidence, suggesting that ivermectin may not be of benefit to COVID-19 patients.
A real-time meta-analysis of 61 studies with 19,432 patients (http://c19ivermectin.com/) showed 74% and 85% improvement for early treatment and prophylaxis of COVID-19 by ivermectin (RR = 0.26 (0.16–0.43) and 0.15 (0.09–0.250), respectively). When only 23 RCTs were included in the analysis, early and late treatment with ivermectin provided 62% (RR of 0.38 (0.27–0.53)) and 46% improvement, respectively. The mortality rate improvement was 68%. Although the improvement and mortality rates of ivermectin for prophylaxis reported were in accordance with the recent systematic review and meta-analysis [24], the quality of evidence remains an issue of interpretation. Another real-time meta-analysis study [25] reported 63% and 83% improvement for early treatment and prophylaxis (RR = 0.37 (0.28–0.47) and 0.17 (0.11–0.26)), respectively.
Despite a number of reports on the clinical benefits of ivermectin for prevention and treatment of COVID-19, more recent studies argued against its clinical effectiveness for such purposes. A randomized, double-blind, placebo-controlled study was conducted in 501 nonhospitalized individuals with COVID-19 in Argentina [26]. Ivermectin had no significant effect on preventing hospitalization of patients with COVID-19. Two large multicenter randomized, double-blind, placebo-controlled clinical trials were conducted to evaluate the effectiveness of ivermectin in inpatients and outpatients with mild to severe COVID-19 infection [27]. Ivermectin given at the dose of 0.4 mg/kg of body weight per day for 3 days did not provide a significant potential effect on clinical improvement, reduction of ICU admission, requirement for invasive ventilation, and death in hospitalized patients. There was also no evidence to support the prescription of ivermectin in terms of recovery, reduction of hospitalization, or increased negative RT-PCR 5 days after treatment in outpatients. A double-blinded, randomized controlled trial was conducted in Thailand in 983 adults aged > 18 years with suspected COVID-19. The efficacy of a 3-day once daily dose (400–600 μg/kg/day) of ivermectin for the prevention and treatment of COVID-19 in confirmed PCR-positive cases [28]. This ivermectin should not be used for either prevention or treatment of COVID-19 in populations with a high rate of COVID-19 vaccination. In a multi-arm randomized clinical trial conducted in 393 patients with PCR-confirmed COVID-19 infection and mild symptoms, single-dose (12 mg) and double-dose (24 mg) ivermectin early treatment was not superior to the placebo in preventing progression to hospitalization and improving the clinical course in mild COVID-19 [29]. A phase II randomized trial was conducted in 112 patients with asymptomatic, mild, or moderate COVID-19 with predominantly hematological illnesses [30]. A single dose of 12 or 24 mg of ivermectin did not reduce viral loads, prevent symptom progression, or reduce mortality in patients with predominantly hematological illnesses who developed mild to moderate COVID-19.
A systematic review and meta-analysis [31] screened 318 records, of which all the high-risk bias studies were excluded. Thirty-one studies were ongoing and 18 studies were awaiting classification or clarification of inconsistency. Thus, in this review, only 14 RCTs were assessed, including 1,678 patients with ivermectin treatment compared with no treatment, placebo, or standard of care. Nine, 4 and 1 study, respectively, involved the investigation of ivermectin efficacy for treatment of moderate COVID-19 inpatients, mild COVID-19 outpatients, and for prevention of SARS-Co-V-2 infection. The sample size of the included studies ranged from 24 to 476 subjects. The authors found only a few studies of high quality; most of the studies had small sample sizes. The quality of evidence (of each outcome parameter) was rated as low to very low certainty. The authors concluded that the currently available evidence does not support the clinical use of ivermectin for the treatment or prevention of COVID-19. Furthermore, there was no evidence to recommend the optimal dosage regimen of ivermectin for both purposes. The most recent systematic review (19 studies) and meta-analysis (17 studies) were performed to evaluate the efficacy of ivermectin for COVID-19 patients based on current peer-reviewed RCTs and to address disputes over the existing evidence [32]. Ivermectin did not have any significant effect on the outcomes of COVID-19 patients with regards to progression to severe disease, negative RT-PCR, disease recovery, duration of hospitalization, time to negative RT-PCR, or viral load. Future studies should address the following gaps: the need for high-quality RCT, the precise definition and relevant time point of outcome measurement, the sufficient reports of patient status according to the WHO clinical progress scale, the studies on severe COVID-19, and the recommendation of optimal dose regimens.
The WHO does not recommend the use of ivermectin in patients with COVID-19 except in the context of a clinical trial [7, 33]. To date, the evidence to support the use of ivermectin for COVID-19 from different clinical studies is still inconclusive [7, 20]. The impacts of ivermectin on mortality, mechanical ventilation, hospital admission, duration of hospitalization, and viral clearance remain uncertain. However, the evidence does support its safety and efficacy in improving survival rates, especially compared to the other repurposed drugs. Currently available evidence was rated as very low certainty due to significantly serious imprecision for most outcome parameters with wide confidence intervals. In addition, there were serious concerns related to the risk of bias in study design and article publication [7]. During the initial phase of the COVID-19 pneumonia pandemic, it was thought that ivermectin might be helpful in patients infected with COVID-19 pneumonia, but this was later proven to be false due to its severe risks/side effects. The Infectious Disease Society of America (IDSA) recommends against the use of ivermectin for COVID-19 pneumonia [34]. Future studies should focus on the quality and RCT study design in patients with varying degrees of severity. A dose-finding study may be required to establish an appropriate dose regimen for COVID-19 [35]. Currently, there are 102 ongoing clinical trials that study the potential use of ivermectin in the treatment and prophylaxis of COVID-19 [36].
Favipiravir by FUJIFILM Toyama Chemical (Avigan). Favipiravir is an antiviral drug approved for influenza in Japan in 2014. The antiviral activity was shown to be through inhibition of the proliferation of SARS-CoV-2. In an in vitro study, favipiravir reduced SARS-CoV-2infection with a half-maximal effective concentration (EC50) of 61.88 µM, a half-cytotoxic concentration (CC50) of > 400 µM, and a selectivity index (SI) of > 6.46. There is a wide window between the CC50 and EC50 values, which indicates that high doses of favipiravir can be safely used [37].
Avifavir (Favipiravir) has been developed for the treatment of COVID-19 in Russia. The pilot phase II/III clinical trial was carried out in patients with moderate symptoms [38]. The study design was an open, randomized, controlled trial. The investigated dose regimens were 1,600 mg given twice a day on the first day, followed by 600 mg twice a day on days 2–14, or 1800 mg twice a day on the first day, followed by 800 mg on days 2–14. Avifavir was found to be superior to the standard treatment (chloroquine or lopinavir/ritonavir). The study recruited 60 patients with COVID-19 (20 in each group). About 62.5% of the patients in the avifavir-treated group were free of infection within 4 days, compared with 30% in the control group (p = 0.018). The fever in the avifavir-treated group recovered faster than in the control group (median: 2 vs. 4 days, p = 0.007). Based on the results of this pilot study, the Russian Ministry of Health approved avifavir for COVID-19 under Emergency Used Authorization (EUA) and approved the continuation of the phase III trial with dosage adjustment to higher than 44 mg/kg for 10 days. Updated information on phase III is not yet available.
A retrospective observational study was conducted in 247 hospitalized adult patients with COVID-19 at five tertiary care hospitals in Thailand [39]. The results showed promising effectiveness of favipiravir for treating COVID-19 patients. In another retrospective study in 421 Thai patients who received favipiravir for COVID-19 during admission to a hospital, low rates of hospital transfer and mortality were observed in mild-to-moderate COVID-19 patients [40]. Older age, high baseline NEWS2 score, and a low loading dose of favipiravir (≤ 45 mg/kg/day) was identified as poor prognostic factors for early clinical improvement. A phase II double-blind randomized controlled outpatient favipiravir trial was conducted in 149 asymptomatic or mildly symptomatic adults with a positive SARS-CoV2 RT-PCR within 72 h of enrollment [41]. The results supported the use of favipiravir at commonly used doses (1,800 mg BID day 1,800 mg BID days 2–10) in outpatients with uncomplicated COVID-19. Early treatment with favipiravir within 3 days of admission reduced the length of stay in hospital and improved clinical manifestations of COVID-19 patients [42].
Several RCT studies [43–49] have evaluated the efficacy of favipiravir at each study site, compared with other treatments – chloroquine, lopinavir/ritonavir, arbidol, baloxavir marboxil, darunavir/cobicistat, and tocilizumab. The doses and duration of various treatment were different. Overall, the sample size of each study was limited, ranging from 30 to 274 cases. The follow-up period varied from 14 to 30 days. Patients’ symptoms ranged from mild to severe. The results obtained from these studies are different and conflicting in some aspects. This makes it difficult to decide whether or not to use favipiravir for COVID-19 treatment.
A systematic review and meta-analysis [50] involving 11 reports of 1,019 patients with mild to moderate symptoms was reported. The studies included four RCTs [38, 43–47], one before-after non-randomized controlled trial [51, 52], and six observational studies (no comparator) or cases series [53–58]. The favipiravir group had significantly better activity on viral clearance on day 7 after treatment (OR = 2.49, 95% CI: 1.19–5.22), while no difference was detected on day 14. Clinical improvement was better than in the control group on both day 7 and day 14 (OR = 1.60 (95% CI: 1.03–2.49) and OR = 3.03 (95% CI: 1.17–7.80), respectively). Favipiravir was capable of clearing the virus within 7 days and contributed to the clinical improvement within 14 days, demonstrating the potential role of favipiravir in treating mild to moderate COVID-19. It was noted, however, that the included studies had a high risk of bias, and the quality of the data was rated as low certainty.
Another review [51] included only controlled trials, eight open, randomized controlled clinical trials [38, 43–49] and one before-after controlled trial [52]. The study involved 827 COVID-19 patients from China, Russia, Oman, Egypt, Japan, and India. The meta-analysis showed a significant improvement in clinical symptoms compared to controls for the 7-day follow-up period (RR = 1.24 (95% CI: 1.09–1.41), p = 0.001), but no significant differences were found in viral clearance, oxygen demand, ICU transfer rate, and incidence of adverse reactions or mortality. It was concluded that the evidence from the analysis might not support favorable benefits from favipiravir in terms of mortality among COVID-19 patients with mild to moderate symptoms. Delayed initiation of treatment may explain the low efficacy in clinical trials; thus, initiation of favipiravir treatment early in the course of illness should be considered [45]. Future clinical trials with appropriate study design and sufficient sample sizes are needed to assess the efficacy and safety of favipiravir for COVID-19. Recently, favipiravir was included in the PRINCIPLE trial as a possible COVID-19 treatment for people recovering at home and in an outpatient setting [53]. Favipiravir has been approved for COVID-19 under Emergency Use Authorization (EUA) in many countries such as Russia, India, China and Bangladesh and has been used off-label in many other countries. In the real-world setting, favipiravir was shown to be well tolerated, with no new safety concerns [59]. Current information is not sufficient to support or reject the use of favipiravir for COVD-19 treatment in patients aged 65 years or older, and further studies in this group of patients are required [60]. Patients with non-severe pneumonia at admission and whose fever resolved within 2 days of treatment were found to be more likely to improve following favipiravir treatment [61]. Preclinical studies demonstrated the risk for teratogenicity and embryotoxicity and the drug is contraindicated during pregnancy [62]. Results of a recent case series study conducted in 9 pregnant women, however, indicate that favipiravir is not likely to be a major teratogen. Nevertheless, it was recommended that pregnant women exposed to favipiravir should be closely followed up.
A meta-analysis was conducted for randomized controlled trials (RCTs) and non-RCTs [63]. Overall, 157 studies (24 RCTs, 1 non-RCT, 21 observational studies, 2 case series, and 106 case reports) were included. Adding favipiravir to the standard of care provided better outcomes (viral clearance, defervescence, chest radiological improvement, hospital discharge at days 10–11) for hospitalized patients with COVID-19.
Considering the approved status, evidence on the safety and key indicators of efficacy of favipiravir in COVID-19 from trials/registries in various countries, favipiravir appears to be helpful in the management of COVID-19, particularly mild to moderate disease. The rapid viral clearance, higher clinical recovery rate, and availability as an oral drug with a proven safety profile make favipiravir a promising repurposed drug for COVID-19. The worldwide ongoing clinical studies on favipiravir to demonstrate the clinical benefits of favipiravir in shortening the disease course, early hospital discharge, and reducing the need for oxygen requirement will provide further insights on its clinical efficacy, safety, and therapeutic place in the overall management of COVID-19.
Azithromycin. Azithromycin is a macrolide antibiotic used widely for bacterial infections. In addition, it has been shown to possess anti-inflammatory, immunomodulatory, and antiviral activities across a wide range of viral infections [54]. In an in vitro study using Vero E-6 cells, azithromycin exhibited antiviral activity against SARS-CoV-2 with EC50, EC90, CC50 and SI of 2.12 µM, 8.65 µM, > 40 µM and > 19, respectively [55]. Based on the pharmacological activities and its safety profile [56–57], azithromycin was proposed to be another potential treatment for COVID-19.
A recent systematic review and meta-analysis of randomized clinical trials in COVID-19 patients have been carried out, including seven studies and 8,822 patients [58]. All of the included studies were randomized controlled trials [64–70]. Among them, only one was a randomized, double-blinded, placebo-controlled trial [70]. The primary outcome parameter was mortality assessed at 6 days in one study [70], 15 days in one study [65], and 28–30 days in five studies [64, 66–69]. Only five studies with a total of 8,754 patients were included in the analysis of the mortality parameter, as two studies did not report the mortality. The mortality rates of 21.2% and 22% in patients with azithromycin and standard of care, respectively, were comparable (OR = 0.96 (95% CI: 0.88–1.05), p = 0.317). Azithromycin did not reduce the mortality rate in any of the included trials and was not associated with the need for invasive mechanical ventilation and length of stay. In terms of safety outcome parameters, there was no difference in the QTc interval or the incidence of arrhythmia. It was concluded that azithromycin did not provide benefit to COVID-19 patients.
A more recent study, a randomized placebo-control trial of azithromycin on COVID-19 was conducted in 263 outpatients [71]. The patients were randomized to receive azithromycin or placebo at the ratio of 2 : 1; 145 patients received azithromycin and 72 patients received placebo. Azithromycin was given as a single oral dose of 1.2 g. There was no difference between the two groups in the primary outcome parameter – the symptom-free rate on day 14. It was concluded that there was no benefit of azithromycin for COVID-19 outpatients.
The current evidence does not support the use of azithromycin in COVID-19 despite its good activity against SARS-CoV-2, together with anti-inflammatory and immunomodulatory activities. The US and UK National Institute of Health recommend against the use of azithromycin for COVID-19 [14, 72]. The decision was based on the evidence that the efficacy of azithromycin was not better than standard care in reducing the risk of death in inpatients with COVID-19, as well as the risk of hospitalization or death in patients with COVID-19 in the community [64–71]. Ongoing studies however, focus on combination therapy of azithromycin with other repurposed drugs such as hydroxychloroquine and chloroquine. Both azithromycin and hydroxychloroquine-chloroquine have been widely used for management based on in vitro studies favoring antiviral effects against the SARS-CoV-2 virus. The findings of some studies were in favor of combination therapy [73–75], while those of other studies were not [76–80]. A retrospective monocentric cohort study was conducted evaluated the 6-week mortality of hospitalized COVID-19 patients treated with azithromycin-hydroxychloroquine combination and other regimens in France [81]. The combination was associated with lower mortality [82]. The combination was significantly associated with increased adverse events. However, the inference of these findings was from observational studies and large randomized trials are imperative to show the future path for using azithromycin-hydroxychloroquine combination therapy. However, as hydroxychloroquine use in COVID-19 has been banned, this may no longer be required.
Tocilizumab (Actemra/RoActemra). Interleukin-6 (IL-6) is one of the critical mediators of autoimmunity, inflammation, and the cytokine storm [83]. Several observational and in vitro studies have shown that IL-6 is a crucial cytokine associated with the severity and mortality of COVID-19 [84, 85]. Tocilizumab is a recombinant humanized, monoclonal, anti-interleukin (IL) 6 receptor antibody that binds to both soluble and membrane-bound IL-6 receptors, inhibiting the IL-6 receptor signal transduction to inflammatory mediators. Tocilizumab has been used to treat rheumatoid arthritis with a promising efficacy and safety profile in different populations [86–92]. The immunomodulatory effects of tocilizumab might be important in patients who have COVID-19 with immune system dysfunction and inflammation, and it may also provide a mortality benefit [93–95].
Although results from various trials on the clinical efficacy of tocilizumab in COVID-19 are controversial [96–98], a prospective pairwise meta-analysis concluded that tocilizumab reduces mortality [99]. The analysis included 10,930 patients from 27 trials. By day 28, the number of deaths in the groups receiving IL-6 blockers, tocilizumab and sarilumab were 1,407 (out of 6,449 cases) and 1,158 (out of 4,481 cases), with absolute mortality risks of 22% and 25%, respectively (OR = 0.83 (95% CI: 0.74–0.92, p < 0.001) and OR = 1.08 (0.86–1.36, p = 0.52) for tocilizumab and sarilumab, respectively). The ORs of tocilizumab and sarilumab for the association with mortality compared with the patients in the usual care or placebo group who received corticosteroids were 0.77 (95% CI: 0.68–0.87) and 0.92 (95% CI: 0.61–1.38), respectively. The corresponding ORs for the association with progression to invasive mechanical ventilation or death were 0.74 (95% CI: 0.66–0.82) and 1.0 (0.74–1.34), respectively. A retrospective cohort study was conducted among COVID-19 patients who received tocilizumab in a tertiary care hospital [100]. The drug was administered intravenously at a dose of 8 mg/kg, with a maximum first dose of 800 mg, and a second dose of 400 or 600 mg was given in the event of laboratory or respiratory worsening, with a maximum cumulative dose of 1400 mg. Patients who were mechanically ventilated at the time of administration of tocilizumab had a significantly higher risk of death by day 28. In contrast, those who received tocilizumab earlier during therapy from the onset of symptoms had better survival outcomes. Tocilizumab improved the outcomes in COVID-19 patients with comorbidities such as diabetes, hypertension, dyslipidemia, obesity, and pulmonary diseases.
The preliminary results of the global phase III randomized, double-blind, multicenter REMDACTA study in hospitalized patients with severe COVID-19 pneumonia comparing tocilizumab with remdesivir and placebo with remdesivir suggested that IL-6 inhibitors alone might be insufficient to suppress the inflammatory phase of COVID-19. In the CORIMUNOTOCI trial [97], an open-label RCT conducted in 130 hospitalized patients in France with moderate or severe COVID-19 pneumonia, patients in the tocilizumab group were shown to have a lower mortality rate or need for ventilation on day 14 but not on day 28, compared with patients in the standard care group (24% vs. 36%, median posterior hazard ratio (HR) 0.58 (90% credible interval 0.33–1.00). In the COVACTA trial [101], a global, randomized, double-blind, placebo-controlled study of 438 hospitalized patients with severe COVID-19 pneumonia, tocilizumab did not improve clinical outcome parameters, i.e., the requirement for intensive care, ventilators, and supplemental oxygen, as well as reduction of mortality on day 28 (OR = 1.19 (95% CI: 0.81–1.76), p = 0.36). In the EMPACTA trial [102], a global, randomized, double-blind, placebo-controlled trial in 389 hospitalized patients with COVID-19 pneumonia not requiring ventilation, the percentage of progression to mechanical ventilation or death by day 28 was 44% lower in patients who received tocilizumab and standard of care compared with placebo and standard of care (12.0% vs. 19.3%, HR = 0.56 (95% CI: 0.32–0.97), p = 0.04). However, there was no significant difference in all-cause mortality on day 28 (10.4% vs. 8.6%; weighted difference 2.0%, 95% CI: –5.2 to 7.8). The REMAP-CAP trial [103], a multinational RCT, was conducted in 803 critically ill patients with suspected or confirmed COVID-19 to evaluate the clinical efficacy of the two IL-6 blockers tocilizumab and sarilumab. Patients were randomly assigned to receive tocilizumab (353 cases), sarilumab (48 cases) or standard treatment (402 cases) within 24 h of admission to the ICU. The median number of days without organ support (primary endpoint) were 10, 11 and 0 (interquartile range: –1 to 16, 0 to 16 and –1 to 15), respectively. In comparison with the control group, the median adjusted OR for tocilizumab and sarilumab groups were 1.64 (95% CI: 1.25–2.14) and 1.76 (95% CI: 1.17–2.91), with posterior probabilities of superiority greater than 99.9% and 99.5%, respectively. In-hospital mortality rates in the tocilizumab and sarilumab groups were 28.0% and 22.2%, respectively. Tocilizumab and sarilumab were found to be effective in all secondary endpoints, including 90-day survival, times to ICU admission and hospital discharge, and improvements in the WHO ordinal scale on day 14.
A cohort study was conducted in 82 patients who had a confirmed SARS-CoV-2 infection and who were treated with tocilizumab at 400 or 600 mg [104]. The results showed that early administration of tocilizumab in patients needing oxygen supplementation might be critical to patient recovery. These preliminary data suggest the requirement of precise timing in initiation of the treatment with tocilizumab.
A single-center retrospective matched cohort analysis was performed in 47 consecutive patients treated with intravenous tocilizumab (IV infusion of 400 or 600 mg within 1 h, followed by 400 mg at 12 h) for severe COVID-19 pneumonia [105]. No apparent benefit of tocilizumab was observed compared to a matched retrospective cohort (standard of care).
A retrospective multicenter study was conducted in 121 subjects treated with tocilizumab (8 mg/kg intravenously single dose) for severe progressive COVID-19 [106]. Older age and high serum lactate dehydrogenase (LDH) levels were found to be predictors of mortality in tocilizumab-treated severe COVID-19 patients. Hypoxia levels, LDH, and central pulmonary involvement radiologically were associated with intubation and non-invasive ventilation.
Two systematic reviews and a network meta-analysis provide a comprehensive overview of the effectiveness of IL-6 receptor blockers when given alone or in combination with corticosteroids in patients with COVID-19 [107, 108]. The more recent review [108] included data from 45 randomized trials and 20,650 patients. The results of the study add to the evidence base, showing the potential of IL-6 receptor blockers in reducing mortality when added to a standard care regimen that includes corticosteroids. The findings are consistent with those from a prospective pairwise meta-analysis [99] and the largest trials on IL-6 receptor blockers, RECOVERY and REMAP-CAP [103, 109]. The information supports the WHO recommendation for using either tocilizumab or sarilumab in combination with corticosteroids for patients with severe or critical COVID-19. Whether IL-6 receptor blockers have any impact on mortality without concomitant use of corticosteroids remains to be investigated. While RECOVERY and REMAP-CAP reported tocilizumab and sarilumab to be effective, the observed effect could be attributed to concomitant treatment with corticosteroids in 82% of the patients [103, 109]. Further subgroup analysis of RECOVERY based on baseline corticosteroids, however, showed that the combination of tocilizumab and dexamethasone improves mortality, especially in patients requiring non-invasive ventilation and high-flow oxygen, but the reduction in mortality was not observed in patients who did not receive corticosteroids [109]. Evidence of a benefit with tocilizumab was not observed in several smaller trials (31% vs. 35%, RR = 0.85 (95% CI: 0.76–0.94, p = 0.0028) as smaller individual trials were underpowered to detect such a modest reduction in mortality. A recent prospective meta-analysis demonstrated that IL-6 antagonists were associated with lower all-cause mortality in hospitalized patients with COVID-19, compared with usual care or placebo [110]. The association was not dependent on the choice of interleukin-6 receptor antagonist. The discordant results across the studies could be due to differences in the degree of respiratory dysfunction in the patients enrolled in each trial, ethnicity of the populations studied, and frequency of glucocorticoid use.
The WHO recommends the use of IL 6 receptor blockers (tocilizumab or sarilumab) for patients with severe or critical COVID-19. The limitation of clinical usage of tocilizumab for COVID-19 treatment is due to the high cost and limited access to medication, as the drug is not available in most settings [111]. Further, corticosteroids are already being recommended for patients with severe or critical COVID-19 [107]. Whether the IL-6 receptor blockers tocilizumab and sarilumab offer any incremental benefits over corticosteroids needs to be investigated. Additional data from ongoing RCTs are required to correctly assess the benefits of using IL-6 inhibitors to manage COVID-19, including the timing and route of administration and different patient populations.
Andrographolide. Andrographolide is a major active component of the Andrographis paniculata extract. It has been used extensively in China and Thailand for upper respiratory infections based on the results of clinical trials [112–117]. Andrographolide has the potential to be an effective anti-COVID-19 drug considering its antiviral, anti-inflammatory, and immunomodulatory [118, 119] activities, as well as its safety profile [120, 121]. Recent in vitro studies provided evidence to support the development of this drug for COVID-19 treatment [5, 6]. Nevertheless, there are very limited clinical studies of andrographolide in COVID-19 despite being recommended under the China National Health Commission treatment guidelines for COVID-19 based on traditional Chinese medicine (TCM) principles [122] and under the Thai National Essential Drug List for COVID-19 treatment [123, 124]. The available clinical evidence is based on two studies that suggest the potential of andrographolide for COVID-19 treatment. The first study was a multicenter, retrospective cohort study [125]. A total of 835 Thai patients with COVID-19 were included in the study; 309 patients received oral andrographolide at the dose of 180 mg daily for 5 days together with the standard of care. Five hundred twenty-six patients in the control group received only the standard of care. It was found that only 3 patients in the andrographolide group developed pneumonia, while 77 patients in the control group developed severe disease progression to pneumonia or required intubations. The quality evidence was, however, rated as very low certainty due to serious concerns related to the risk of bias in the study design.
In another study, 130 Chinese patients with mild to moderate COVID-19 were recruited [126]. The study design was an open, randomized trial. Sixty-five patients received andrographolide intravenously (IV) at the dose of 10 mg/kg/day (maximum of 500 mg) for 7–14 days combined with standard of care, while those in the controlled group received only standard of care. The complete symptom resolution time was shown to be shorter in the treatment group (8.33 vs. 11.86 days, p = 0.008). Andrographolide significantly reduced the virus clearance time (7.97 vs. 12.23 days, p < 0.001). Six patients in the control group developed severe symptoms during the study period, while none in the treatment group developed severe symptoms. The quality evidence of this study was rated as low certainty due to the concern about the risk of bias related to study design and small sample size.
It should be noted that there is a marked difference in the dosage of andrographolide used in these two studies. Acute kidney injury was reported with the use of high doses (100–750 mg daily) of andrographolide in other diseases [127]. A dose-finding study may be needed to clarify the optimal dosage regimen for mild, moderate, and severe COVID-19 disease. Furthermore, a high-quality RCT with a sufficient sample size is required in order to confirm the findings of these two studies. Future studies should provide evidence to support the effect of andrographolide on the key outcome parameters that significantly impact COVID-19 patients. Andrographolide is a major active component of A. paniculata, which is widely available, cheap, and relatively safe; however, this should not mandate the use of andrographolide while the benefit is still uncertain due to very limited clinical data in COVID-19 patients.
Conclusions. Repurposing existing drugs requires significantly less capital and time and diminishes the clinical risks as the drugs have been tested for toxicity, pharmacokinetics, pharmacodynamics, dosing, etc., for their primary indications. For repurposing of clinically approved drugs to be viable, there must be sufficient evidence that confirms the improvement of the significant outcome parameters that impact COVID-19 patients, including faster time to clinical improvement and viral clearance, and reduction of the duration of hospitalization, severe disease progression, the requirement of mechanical ventilation, and mortality rate. The urgent need for treatment during an outbreak can mislead the interpretation of research results if there is no control arm. During the early phase of the illness, a randomized placebo-control trial may be the study design of choice, as up to 80% of COVID-19 cases are self-limiting. It may not be possible to conclusively determine the efficacy of the drug without placebo control. The quality of research on repurposed drug development should be the same as that on any new drug development. The data should demonstrate evidence of efficacy and safety. As such, the scientific and ethical validity of clinical research is necessary. High-quality RCTs with sufficient power and conducted in accordance with good clinical practice and ethical standards are essential. There is an urgent need to effectively prioritize among the proposed repurposed approaches and to effectively study them in order to guide clinical practice. Due to the small number of published studies, some outcomes were borderline. Subgroup meta-analyses were not possible for different severities, different doses, and nonhospitalized patients. Another issue with the included reports was that the definition of chest radiological imaging and clinical improvement statuses differed according to the protocol that each country followed. These caused higher heterogeneity and increased the 95% CI in some analyses.
Apart from monotherapy, combination therapy of repurposed drugs that simultaneously target virus replication enzymes and host human kinases could be a promising approach for COVID-19 prevention and treatment. The remdesivir-baricitinib combination encouraged combinatorial drug strategies, opening an important avenue in COVID-19 therapeutics. The combination of repurposed drugs may reduce the adverse effects, recovery time, and hospitalization stay and improve patient clinical status for non-invasive ventilation.
Short-term repurposing of existing drugs might not provide a successful outcome for COVID-19 patients and more clinical trials should be initiated to search for better therapeutics for COVID-19 patients using potential antiviral molecules, being evaluated in different phases of clinical trials. Multiple repurposed drugs are currently being studied for COVID-19 in clinical trials, and many more are being investigated in preclinical models.