Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
AUTOIMMUNITY / RESEARCH PAPER
Outcomes of SARS-CoV-2 infection in patients under treatment with pharmacological immunosuppression. A Swiss cohort study.
1
Gastroenterology and Hepatology, Ente Ospedaliero Cantonale, Università della Svizzera Italiana, Lugano, Switzerland, Switzerland
2
Epatocentro Ticino, Università della Svizzera Italiana, Lugano, Switzerland, Switzerland
3
King's College London Faculty of Life Sciences & Medicine, Institute of Liver Studies, MowatLabs, London, United Kingdom, United Kingdom
4
Intensive Care Unit, Ente Ospedaliero Cantonale, Lugano, Switzerland, Switzerland
5
Clinical Trial Unit, Ente Ospedaliero Cantonale, Lugano, Switzerland, Switzerland
6
Division of Pneumology, University Hospital of Geneva, Geneva, Switzerland, Switzerland
7
ICT (Information and Communication Technologies), Ente Ospedaliero Cantonale, Bellinzona, Switzerland, Switzerland
Submission date: 2022-04-15
Final revision date: 2022-06-30
Acceptance date: 2022-07-25
Online publication date: 2022-08-03
Corresponding author
Antonio Galante
Gastroenterology and Hepatology, Ente Ospedaliero Cantonale, Università della Svizzera Italiana, Lugano, Switzerland, Switzerland
Gastroenterology and Hepatology, Ente Ospedaliero Cantonale, Università della Svizzera Italiana, Lugano, Switzerland, Switzerland
KEYWORDS
cancerimmunosuppressionautoimmunityrheumatologychronic obstructive pulmonary diseaseliver diseaseCOVID-19SARS-CoV-2solid organ transplant
TOPICS
ABSTRACT
Introduction:
The impact of pharmacological immunosuppression (IS) on COVID-19 outcomes is unclear. This study aimed at investigating the outcomes of hospitalised patients undergoing IS and focussed on length of hospital stay, admission to intensive care unit (ICU) and mortality.
Material and methods:
Patients admitted to public hospitals in Southern Switzerland with SARS-CoV-2 infection (n = 442) were prospectively included, and their data were collected and analysed. Immunosuppressed patients were compared to patients from the same cohort but without any IS.
Results:
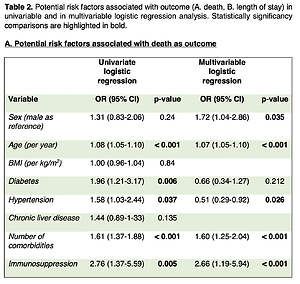
Thirty-five patients (7.9%, 65.7% male, median age 70.6 years) were treated with IS at the time of hospital admission. Compared with patients without IS, immunosuppressed patients showed higher mortality (n = 16 / 35, 45.7% vs n = 95 / 407, 23.3% p = 0.003) and longer hospital stay (median = 15.5 days vs median = 11, p = 0.0144). Moreover, in the univariate and multivariable logistic regression analysis, IS was independently associated with mortality (OR = 2.76 (95%-CI: 1.37-5.59) and 2.66 -95%-CI: 1.19-5.94 -) and in the linear univariate and multivariable regression analysis with the length of stay (p = 0.005 and p = 0.007). Furthermore, patients under IS were more often admitted to the ICU, although the association was not significant (p = 0.069).
Conclusions:
Patients under IS were at a significantly higher risk of severe and prolonged COVID-19 disease, with higher mortality and more extended hospital stay than patients without IS.
The impact of pharmacological immunosuppression (IS) on COVID-19 outcomes is unclear. This study aimed at investigating the outcomes of hospitalised patients undergoing IS and focussed on length of hospital stay, admission to intensive care unit (ICU) and mortality.
Material and methods:
Patients admitted to public hospitals in Southern Switzerland with SARS-CoV-2 infection (n = 442) were prospectively included, and their data were collected and analysed. Immunosuppressed patients were compared to patients from the same cohort but without any IS.
Results:
Thirty-five patients (7.9%, 65.7% male, median age 70.6 years) were treated with IS at the time of hospital admission. Compared with patients without IS, immunosuppressed patients showed higher mortality (n = 16 / 35, 45.7% vs n = 95 / 407, 23.3% p = 0.003) and longer hospital stay (median = 15.5 days vs median = 11, p = 0.0144). Moreover, in the univariate and multivariable logistic regression analysis, IS was independently associated with mortality (OR = 2.76 (95%-CI: 1.37-5.59) and 2.66 -95%-CI: 1.19-5.94 -) and in the linear univariate and multivariable regression analysis with the length of stay (p = 0.005 and p = 0.007). Furthermore, patients under IS were more often admitted to the ICU, although the association was not significant (p = 0.069).
Conclusions:
Patients under IS were at a significantly higher risk of severe and prolonged COVID-19 disease, with higher mortality and more extended hospital stay than patients without IS.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.