Introduction
Nutritional deficiencies remain a severe public health burden worldwide [1]. They include deficiencies in iron, iodine, and vitamin A, among other nutrients, and can lead to protein-energy malnutrition [2]. Recently, it was found that from 2010 to 2019, the age-standardized disability-adjusted life-year (DALY) rates due to nutritional deficiencies increased in high-income North America and Western Sub-Saharan Africa [3].
Nutritional deficiencies have substantial adverse effects on the health of children and pregnant women [1]. That is, during childhood, nutritional deficiencies can decrease short-term survival and affect long-term health and development [4], and during pregnancy, they are associated with all-cause maternal mortality [5] and adverse birth outcomes, such as low birth weight, preterm birth, and small for gestational age [6, 7].
Insufficient nutrient intake during adolescence, when growth spurts occur, results in a failure to meet the increased nutrient demands to support rapid growth, sexual maturity, and menstruation, and ultimately, results in malnutrition [8–10]. Similarly, poverty, climate change, habitat destruction, human immunodeficiency virus infection, parasitic infections, and changes due to urbanization affect the food security of women of reproductive age in South Africa and Western Sub-Saharan Africa [11, 12]. Consequently, decreasing the global burden of nutritional deficiencies is a top priority of public health organizations and governments worldwide. One approach to decreasing this burden involves the production of fortified foods and the implementation of national food-fortification programs, which have substantially lowered the prevalence of micronutrient deficiencies in many developed countries [13]. Furthermore, the World Health Organization has addressed the problem of malnutrition by setting a global nutrition target that consists of the following six goals to be achieved by 2025: (i) a 40% reduction in the global number of children aged under 5 whose growth is stunted; (ii) a 50% reduction in the global incidence of anemia in women of reproductive age; (iii) a 30% reduction in the global incidence of low birth weight; (iv) no increase in the global incidence of childhood overweight; (v) a global increase of at least 50% in the rate of exclusive breastfeeding of babies aged 0–6 months; and (vi) a reduction in the global incidence of childhood wasting to less than 5% [14, 15]. Moreover, one of the United Nations’ Sustainable Development Goals is to eliminate malnutrition by 2030 [16], and the United Nations has proclaimed that 2016–2025 is the “Decade for Action on Nutrition” to support international collaborative efforts to decrease malnutrition on a global scale.
The Global Burden of Disease Study (GBD) 2019 was a comprehensive international study that evaluated the burden of 369 injuries and diseases, including malnutrition, in 204 countries and territories, from 1990 to 2019 [2]. Therefore, an analysis of data from GBD 2019 should reveal the distribution of and trends in the burden of nutritional deficiencies in 204 countries and territories during this period. This would help researchers, physicians, and governments worldwide to optimize the distribution of scientific and medical resources to effectively improve the prevention and treatment of nutritional deficiencies.
In the present study, we determined the incidence rate of and DALYs due to nutritional deficiencies in 204 countries and territories, and examined how these parameters varied by country, region, sociodemographic index (SDI), age, and sex.
Material and methods
Data source
We used the Global Health Data Exchange query tool (http://ghdx.healthdata.org/gbd-results-tool) to collect publicly available data on nutritional deficiencies from 1990 to 2019 from the GBD database, using the keywords “nutritional deficiencies” , “incidence” , “DALYs” , and “estimated annual percentage change (EAPC)” according to the GBD’s operational guidelines [17]. Data collection was performed from August to December 2022.
The GBD database contains published studies, surveys, and epidemiological data collated by teams of researchers on more than 360 diseases in 204 countries and territories, including each disease’s prevalence and associated morbidity and mortality [2]. The GBD database does not include studies with incomplete data, those that are of low quality, or those that are inconsistent with the GBD study’s purpose. The data sources of the GBD database undergo strict quality control and validation, such that the authoritativeness of the GBD study is recognized by many scholars and research institutions. Moreover, to reflect dynamic changes in the global disease burden and ensure accuracy, GBD study data are updated annually.
GBD 2019 comprehensively analyzed and estimated the prevalence of 369 diseases and injuries and 87 risk factors in 204 countries and territories from 1990 to 2019 [2]. As we only used data from publicly available GBD 2019 databases, we did not require clinical ethical approval for this study.
The SDI is a composite indicator of a country’s level of socioeconomic advancement based on the fertility rate, income per capita, and education level [17]. We extracted the SDI for each country and then classified countries into SDI regions, namely high-SDI (0.805–1.00), high-middle-SDI (0.690–0.805), middle-SDI (0.698–0.690), low-middle-SDI (0.455–0.608), and low-SDI (0.00–0.455) regions [17].
DALYs represent the overall number of years of healthy life lost from morbidity to mortality, namely the healthy life years lost due to mortality from disease, disability, and illness. The number of DALYs of a specific population can be calculated to determine the population-wide number of years of life lost due to death from disease and the effects of disability. Subsequently, the relative value of life years (an age weight) and the relative value of time (a discount ratio) are used to make weighted adjustments.
Statistical analysis
We calculated 95% uncertainty intervals (UIs) for each of the estimated incidences, numbers, and rates of DALYs. Specifically, each estimate (e.g., such as the age-standardized incidence) was computed 1,000 times, with each computation sampled from distributions of data inputs, data transformations, and model choices, and 95% UIs were then determined from the 25th and 975th values arranged in ascending order. The annual age-standardized incidence rates and DALY rates, and their corresponding EAPCs, were analyzed to evaluate the burden of nutritional deficiencies.
Age standardization aims to eliminate the effect of population age composition and thereby ensure comparability of research indicators. The age-standardized rates in the GBD database were estimated using the world-population age standard. Direct standardization generates standardized or age-adjusted rates, which are weighted averages of specific age rates for each population being compared. The weight (standard) is used to represent the relative age distribution of an external population and serves as a summary rate for each population. This rate reflects the number of events that can be expected to occur if the populations being compared have the same age distribution.
EAPC is a widely accepted parameter used for quantitatively describing trends in age-standardized incidence rates over specific time intervals. It was calculated from a regression model fitted to the natural logarithm of the incidence rate. The regression model was y = b 0 + βx + c, y = ln(age – standardized rate), where x is the calendar year, b 0 is a constant term, c is a false term, and β is the negative or positive tendency of the selected age-standardized rate. The EAPC was calculated using the following formula: EAPC = 100 × (exp [β] – 1), where exp is an exponential function in advanced mathematics based on the natural constant e. Exp (x) represents the x power of e, and x can be a function. The 95% confidence interval (CI) of the EAPC was obtained from the linear regression model.
The age-standardized rate was regarded as increasing if its EAPC and the lower bound of its 95% CI were positive, whereas it was regarded as decreasing if its EAPC and the higher bound of its 95% CI were negative. Otherwise, it was regarded as being unchanged. All statistical analyses were performed using R software, and p < 0.05 was considered as indicating statistical significance.
Results
Trends in the age-standardized incidence rates of nutritional deficiencies
From 1990 to 2019, the global age-standardized incidence rate of nutritional deficiencies remained stable, as the EAPC was –-0.05 (95% CI: –0.20 to 0.09; Table I, Figure 1 A, Supplementary Figure S1 A). However, during this period, the age-standardized incidence rate of nutritional deficiencies increased in men (EAPC = 0.10), but decreased in women (EAPC = –0.23; Table I, Figure 1 A, Supplementary Figure S1 A). Moreover, in 1990 and 2019, the age-standardized incidence rates of nutritional deficiencies were higher in men than in women, with male-to-female ratios for these rates of 1.10 and 1.17, respectively (Table I).
Table I
The age-standardized incidence rate (ASIR) of nutritional deficiencies in 1990 and 2019 and its temporal trends
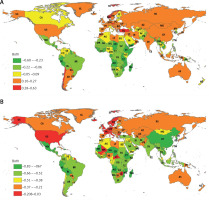
Figure 1
The EAPC of age-standardized rates of nutritional deficiencies from 1990 to 2019 by sex and region. A – The EAPC of ASIR. B – The EAPC of age-standardized DALY rate

Globally, the female-to-male ratios of the incidence rate of nutritional deficiencies by age group followed a bimodal distribution, with the highest rate in those aged 80–84 (Supplementary Figure S2 A). An analysis by SDI region revealed that the female-to-male ratio of the incidence rate of nutritional deficiencies was the highest in those aged 30–34 in high-SDI regions, those aged 80–84 in middl-high-SDI regions, those aged 65–69 in middle-SDI regions, and those aged 40–44 in low-middle- and low-SDI regions (Supplementary Figures S2 B–F).
In 2019, the age-standardized incidence rates of nutritional deficiencies were higher in middle- and low-middle-SDI regions than in other regions (Table I), and were the highest in low-middle-SDI regions, followed by middle-SDI regions. From 1990 to 2019, the age-standardized incidence rate increased the least in high-SDI regions (EAPC = 0.19) and increased the most in high-middle-SDI regions (EAPC = 0.76), followed by middle-SDI regions (EAPC = 0.23; Table I, Figure 1 A, Supplementary Figure 1 A).
Furthermore, the EAPC in the age-standardized incidence rate of nutritional deficiencies was negatively related to the age-standardized incidence rate (ρ = –0.371, p = 0.001; Supplementary Figure S3 A) and SDI (ρ = –0.587, p = 0.001; Supplementary Figure S3 B). For example, from 1990 to 2019, low-SDI regions had a higher incidence of nutritional deficiency in young people than in older people. In contrast, from 1990 to 2019, high-SDI regions had a higher incidence of nutritional deficiency in people aged over 70 than in younger people (Supplementary Figures S4 A, B). Moreover, the annual incidence of nutritional deficiencies in older adults increased from 1990 to 2019 (Supplementary Figure 5 A). Furthermore, from 1990 to 2019, in all but the high-SDI regions, the incidence rate of nutritional deficiencies was substantially higher in those aged 1–4 than in other age groups (Supplementary Figures 7 A–F).
At the region level, in 2019, the age-standardized incidence rates of nutritional deficiencies were the highest in South Asia, Southeast Asia, and East Asia, whereas they were the lowest in Andean Latin America (Table I; Supplementary Table SII). From 1990 to 2019, the age-standardized incidence rate increased the most in Australasia (EAPC = 0.61), followed by East Asia (EAPC = 0.50) and Central Europe (EAPC = 0.44; Table I; Figure 1 A; Supplementary Table SII).
At the country level, in 2019, age-standardized incidence rates of nutritional deficiencies were the highest in Sri Lanka, the Maldives, and India, whereas they were the lowest in Peru, Mongolia, and the Dominican Republic (Supplementary Tables SI, SIII). From 1990 to 2019, the age-standardized incidence rate increased the most in Czechia (EAPC = 1.81), followed by Turkey (EAPC = 1.45) and Bhutan (EAPC = 1.10). From 1990 to 2019, in women, the age-standardized incidence rate of nutritional deficiencies increased the most in Czechia (EAPC = 1.83), followed by Turkey (EAPC = 1.41) and Qatar (EAPC = 1.33), whereas in men, the age-standardized incidence rate of nutritional deficiencies increased the most in Bhutan (EAPC = 2.44), followed by Czechia (EAPC = 1.78) and Turkey (EAPC = 1.49; Figure 2 A, Supplementary Tables SI, SIII). Age distribution of incidence rate for nutrientional deficiencies in different countries in 2019 is shown in Supplementary Table SV.
Figure 2
The EAPC of age-standardized rates of nutritional deficiencies from 1990 to 2019 by country. A – The EAPC of ASIR. B – The EAPC of age-standardized DALY rate
US – United States, CA – Canada, GL – Greenland, MX – Mexico, CO – Colombia, BR – Brazil, EC – Ecuador, PE – Peru, BL – Bolivia, PA – Paraguay, AR – Argentina, CI – Chile, IC – Iceland, AG – Algeria, MR – Mauritania, ML – Mali, NG – Niger, CD – Chad, EG – Egypt, SU – Sudan, CT – Central African Republic, TZ – Tanzania – United Republic of, OG – Zaire, AO – Angola, WA – Namibia, SF – South Africa, MA – Madagascar, MZ – Mozambique, ZI – Zimbabwe, ZA – Zambia, ET – Ethiopia, KE – Kenya, SP – Spain, PO – Portugal, FR – France, GM – Germany, PL – Poland, UP – Ukraine, NO – Norway, SW – Sweden, FI – Finland, BO – Belarus, RO – Romania, UK – United Kingdom, TU – Turkey, SY – Syria, IZ – Iraq, SA – Saudi Arabia, YM – Yemen, MU – Oman, TC – United Arab Emirates, IR – Iran, AF – Afghanistan, TX – Turkmenistan, PK – Pakistan, IN – India, UZ – Uzbekistan, TI – Tajikistan, KG – Kyrgyzstan, KZ – Kazakhstan, RS – Russia, MG – Mongolia, CH – China, NP – Nepal, BM – Myanmar (Burma), TH – Thailand, CB – Cambodia, VM – Vietnam, ID – Indonesia, AS – Australia, PP – Papua New Guinea, NZ – New Zealand, TW – Taiwan, KM – North Korea, KS – South Korea, JA – Japan, CE – Sri Lanka.
Changes in DALY rates due to nutritional deficiencies
From 1990 to 2019, there was a decrease in the global age-standardized DALY rate due to nutritional deficiencies (EAPC = –2.91; Table II, Figure 1 B, Supplementary Figure S1 B), and this decrease occurred in both men (EAPC = –3.18) and women (EAPC =–2.69) (Table II, Figure 1 B, Supplementary Figure S1 B). Moreover, during this period, the age-standardized DALY rate was lower in men than in women (Table II).
Table II
The age-standardized DALY rate of nutritional deficiencies in 1990 and 2019 and its temporal trends
From 1990 to 2019, the age-standardized DALY rate due to nutritional deficiencies decreased in all SDI regions, with the largest decrease occurring in low-middle SDI regions (EAPC = –3.98; Table II). Additionally, the EAPC in the age-standardized DALY rate due to nutritional deficiencies was negatively related to the age-standardized DALY rate (ρ = –0. 510, p = 0.001; Supplementary Figure S3 C) and SDI (ρ = –0.394, p = 0.001; Supplementary Figure S3 D). Moreover, in 1990 and 2019, high-SDI regions had higher numbers of DALYs due to nutritional deficiencies in young people than in older people, whereas low-SDI regions had higher numbers of DALYs due to nutritional deficiencies in people aged over 70 (Supplementary Figures S4 C, D). However, from 1990 to 2019, in older adults, the annual number of DALYs due to nutritional deficiencies decreased (Supplementary Figure S5 B). In addition, in all regions (regardless of SDI), the number of DALYs due to nutritional deficiencies was the highest in those aged 1–4 (Supplementary Figure S8). Worldwide, the female-to-male ratio in the number of DALYs due to nutritional deficiencies was the highest in those aged 90–94 (Supplementary Figure S6 A). Furthermore, the female-to-male ratio in the number of DALYs due to nutritional deficiencies was the highest in those aged 85–89 in low-middle, middle-, high-middle-, and high-SDI regions, and in those aged 90–94 in low-SDI regions (Supplementary Figures S6 B–F).
In 2019, the regions with the highest age-standardized DALY rates due to nutritional deficiencies were Eastern Sub-Saharan Africa, South Asia, and Central Sub-Saharan Africa (Table II, Supplementary Table SII). From 1990 to 2019, the largest decrease in the age-standardized DALY rate due to nutritional deficiencies occurred in East Asia (EAPC = –6.20), followed by Andean Latin America (EAPC = –4.91) and Eastern sub-Saharan Africa (EAPC = –4.13; Table II, Figure 1 B, Supplementary Table SII).
In 2019, the countries with the highest age-standardized DALY rates due to nutritional deficiencies were Mali, Somalia, and the Central African Republic, whereas those with the lowest age-standardized DALY rates due to nutritional deficiencies were Canada, Greece, and Australia. From 1990 to 2019, the age-standardized DALY rate due to nutritional deficiencies decreased the most in the Democratic People’s Republic of Korea (EAPC = –9.28) and increased the most in Zimbabwe (EAPC = 1.35). From 1990 to 2019, in both men and women worldwide, the age-standardized DALY rate due to nutritional deficiencies decreased the most in the Democratic People’s Republic of Korea (EAPC women = –8.34; EAPC men = –10.38) and increased the most in Zimbabwe (EAPC women = 1.86; EAPC men = 0.97; Figure 2 B, Supplementary Tables SI, SIV). Age distribution of DALYs rate for nutrientional deficiencies in different countries in 2019 is shown in Supplementary Table SVI.
Discussion
From 1990 to 2019, the global age-standardized DALY rates due to nutritional deficiencies decreased, although the global age-standardized incidence rate of nutritional deficiencies increased (Figure 1). Moreover, the global burden of nutritional deficiencies varied significantly with different SDI region, as the quality of medical facilities and healthcare systems differs markedly between countries with different SDIs. In 2019, the age-standardized incidence rate of nutritional deficiencies was higher in low-middle-SDI regions than in other regions. In addition, from 1990 to 2019, the age-standardized DALY rate due to nutritional deficiencies was the highest in low-SDI regions, and decreased the most in low-middle- and low-SDI regions (Table I).
Compared with other SDI regions, low-SDI regions have lower-quality healthcare services that cannot perform early screening or continuous monitoring interventions. In addition, in low-SDI regions, over-processed and high-calorie foods are more readily available and cheaper than other foods. Consequently, people in low-SDI regions consume low-fiber, high-saturated-fat, high-calorie, high-salt, high-sugar, highly processed foods, rather than high-fiber, low-saturated-fat, low-calorie, low-salt, low-sugar, lightly processed foods [18]. Furthermore, decreasing incomes, due to increasing unemployment, coupled with the high cost of nutritious foods, place added pressure on people in low socioeconomic groups, such that their diets are largely based on a limited number of inexpensive and non-nutritious forms of staple foods [19].
The high rates of nutritional deficiencies in middle- and low-SDI regions may be partly due to factors such as environmental degradation, climate variability, economic recession [20], and food supplies being insufficient to meet basic energy demands. Rapid urbanization in these countries has also caused changes in dietary patterns. For example, overconsumption of energy-intensive, but poorly nutritious fast foods available in cities generates a “double burden”: malnutrition and overweight [21]. Food-borne diseases are also rampant in middle- and low-income countries because climate change has caused contamination of the water used to clean and cook food [21]. Additionally, the aging of populations worldwide has exacerbated malnutrition-related diseases [20], and unhealthy habits (e.g., smoking, alcohol abuse, and drug abuse) and diseases (e.g. acquired immunodeficiency syndrome) may exacerbate nutritional deficiencies or their incidence [22]. For example, adults with certain infectious and non-fatal diseases have to reduce their number of work hours, meaning that their ability to buy healthy food is decreased. This situation is worsened by the costs of health care and supporting a family [23].
In 2019, the age-standardized incidence rate of nutritional deficiencies was the highest in South Asia, as this rate was the highest in the countries in this region, such as Sri Lanka, the Maldives, and India. In 2019, the highest age-standardized DALY rates due to nutritional deficiencies occurred in Eastern South Asia and Sub-Saharan Africa. In the latter region, these high rates are partly attributable to deficiencies in selenium and vitamin A in the diets of people in countries such as the Central African Republic, Somalia, and Mali [24, 25]. Thus, women, infants, and children in these countries are more vulnerable to malnutrition than those in other countries, and approximately 45% of fatalities in children aged under 5 worldwide are associated with malnutrition [24, 25]. In addition, childhood overweight and obesity rates are increasing in the Central African Republic, Somalia, and Mali [15], and the incidences of numerous noncommunicable illnesses, such as diabetes, several malignancies, and cardiovascular diseases, have increased in such countries. Effective ways of ameliorating nutritional deficiencies include the use of supplements and food fortification, and increasing dietary variety. An ample cadre of community health workers must also be trained to identify and promptly respond to initial indications of malnutrition and thereby decrease the incidence of severe malnutrition [26].
However, there are many obstacles to the successful implementation of policies to alleviate nutritional deficiencies in middle- and low-income countries. For instance, policymaking is not integrated with national development agendas, policies are implemented too slowly, and development is imbalanced across areas. There is also inadequate inspection, testing, multi-sectoral joint action, financial support, legislation, and enforcement [27, 28]. Additionally, various cultural and social factors are common causes of malnutrition in middle- and low-income countries [29].
The findings of this study reveal that the age-standardized DALY rates due to nutritional deficiencies in developed countries and regions are generally lower than those in developing countries and regions. In 2019, the countries with the lowest DALY rates due to nutritional deficiencies were Canada and Greece. This may be because compared with developing countries, developed countries possess more human and financial resources to promote food diversity, conduct food testing, and employ experts to monitor the nutrition of the national population.
We also found that, from 1990 and 2019, the age-standardized incidence rate of nutritional deficiencies was lower in women than in men. This is consistent with a previous finding that the age-standardized incidence rate of vitamin A insufficiency is higher in men than in women, and that male sex is a risk factor for vitamin A insufficiency [29]. In addition, we found that, from 1990 and 2019, there was an increase in the incidence rate of all nutritional deficiencies and protein-energy malnutrition in men [30]. The reduction in the age-standardized incidence rate of nutritional deficiencies in women may be caused by several factors, such as an increased emphasis on the health of mothers and children in health awareness campaigns. However, we also found that the age-standardized DALY rates due to nutritional deficiencies were lower in men than women.
There are some limitations to this study. First, the quantity and quality of data in the GBD database dictated the accuracy of our findings and are limited for several underdeveloped regions, such as Africa and Latin America, as many countries in these regions do not have reliable information systems. Second, GBD 2019 used countries as the basic units in its analyses and did not account for the potential influence of race on health. Third, before the European Society for Parenteral and Enteral Nutrition issued a consensus on the diagnosis of malnutrition in 2018, there was no agreed definition of nutritional deficiency. Coupled with heterogeneous nutritional screening practices, this lack of an agreed definition greatly hindered accurate evaluation of the extent of nutritional deficiencies prior to 2018 [31]. Thus, a lack of comprehensive data for several underdeveloped countries might have decreased the robustness of our results for low-SDI regions. In addition, the absence of a consistent definition for nutritional deficiency may have affected comparisons of nutritional deficiency rates and DALY rates between regions and countries. This highlights the need for more studies based on updated databases to reveal the true global burden of nutritional deficiencies.
In conclusion, we found that the age-standardized incidence rates of and DALY rates due to nutritional deficiencies remained high in low-middle- and low-SDI regions from 1990 to 2019. Southeast Asia was the region with the greatest burden of nutritional deficiencies, and Czechia and Turkey were the two countries with the greatest burden of nutritional deficiencies. These and other findings of this study may be used to help identify trends in the distribution of burdens of nutritional deficiencies worldwide, thereby facilitating the development of regional and national strategies to alleviate this problem. They may also assist health-related decision-making and contribute to improvements in the prevention, treatment, and management of nutritional deficiencies worldwide.



