Introduction
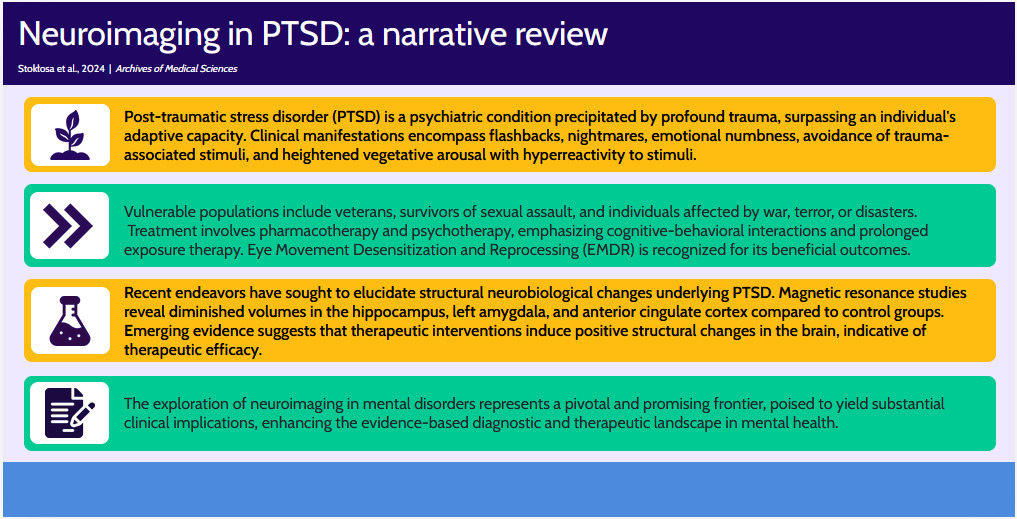
Post-traumatic stress disorder (PTSD) is a debilitating condition arising subsequent to exposure to trauma, resulting in multifaceted impairments in human functionality. Its correlation with concomitant illnesses and an escalated risk of mortality through injury or suicide attempts has been well documented [1]. The elucidation and exploration of PTSD hold paramount importance for myriad reasons. Enhanced comprehension facilitates clinical management, enabling precise identification and targeted treatment interventions. Augmented awareness fosters empathy, mitigating stigma and fostering a supportive societal milieu. In a broader public health framework, insights into PTSD inform preventative strategies, early interventions, and community support endeavors. Continuous investigation into the neurobiology and associated factors of PTSD propels innovation in therapeutic modalities and preventive measures. This comprehension is particularly pivotal in bolstering support for veterans and trauma survivors, ensuring superior post-deployment care and successful reintegration. Additionally, it is indispensable in professional and educational domains, guiding the implementation of supportive policies and resources. Ultimately, a holistic understanding of PTSD contributes to healthier familial dynamics, improved interpersonal relationships, and enhanced communal well-being. Neuroimaging methodologies have emerged as invaluable tools for delineating alterations in the human brain consequent to severe stressors. Distinct modifications in specific brain regions warrant attention from researchers, as these alterations may underlie symptomatic expressions of stress, such as re-experiencing trauma [2].
The aim of this review is to provide a comprehensive exploration of the epidemiology, symptoms, and ramifications of PTSD, supplemented by insights gleaned from neuroimaging investigations. Our review draws upon searches conducted in PubMed, Cochrane, and Medline databases utilizing keywords pertinent to PTSD characteristics, symptoms, comorbidity, complications, and neuroimaging. All authors participated in these searches, adhering to inclusion criteria encompassing articles from peer-reviewed English-language journals. The search methodology was iterative, involving screening based on titles and abstracts. Article selection was guided by the clinical expertise and theoretical acumen of the authors, who possess extensive backgrounds in psychiatry and neuroscience. No constraints were imposed based on the publication dates of the studies. Following article acquisition, a narrative and empirical synthesis was meticulously performed.
Diagnosis and clinical significance of PTSD
PTSD is a multifaceted condition encompassing cognitive, somatic, affective, and behavioral manifestations resulting from past psychological trauma. The development of PTSD can be influenced by various events, with some of the most common factors being sexual violence (e.g., rape), child abuse, sexual violence within relationships (approximately 33%), traumatic experiences related to interpersonal relationships (such as the sudden death of a spouse or traumatic events involving relatives or children – 30%), experiencing physical violence (physical assault or violence during childhood and adolescence – 12%), being a victim of organized violence (3%), participating in violent activities (e.g., war or witnessing war – 11%), and other events perceived as generally traumatic in a person’s life (11%) [3].
The overall prevalence of post-traumatic stress disorder is estimated to range from 6.1% to 9.2% in the general population of adults living in North America and Canada [4]. The prevalence of PTSD varies across populations and countries, with Africa, Spain, or Italy having an estimated prevalence of approximately 2%, Japan having a lower prevalence (around 1.3%), and Northern Ireland having a PTSD prevalence of approximately 8.8%. The occurrence of this disorder is influenced by country-specific sociopolitical and regional conditions [5].
Recent observations indicate the development of post-traumatic stress disorder in medical personnel due to the COVID-19 pandemic, with a meta-analysis revealing PTSD in approximately 21.5% of all respondents [6]. PTSD prevalence is twice as common in women following exposure to traumatic events, while accidents, the death of a loved one, or disasters lead to PTSD with comparable frequency in both sexes [7].
Symptoms of PTSD continue to be distressing for affected individuals, negatively impacting various aspects of their functioning. These symptoms include reliving the traumatic event, intrusive thoughts, and nightmares. Additionally, patients may experience symptoms related to dissociation, heightened emotional and physical reactions when recalling the trauma, sleep and concentration disturbances, irritability, excessive vigilance, an increased startle response, and actions aimed at avoiding traumatic stimuli [8].
According to the DSM-V, the criteria for the diagnosis of PTSD were divided into different categories, including:
– Criterion A: stressor – exposure to a real threat of death, injury, or sexual violence in one of the following ways: direct exposure to or witnessing the trauma, knowledge of the traumatic event by close persons, or indirect exposure to the details of the trauma experienced.
– Criterion B: intrusion symptoms – recurrent, intrusive thoughts and nightmares related to the past event, dissociative reactions in which symptoms of re-experiencing the traumatic situation may occur, persistent and intense psychological distress following a difficult experience, and physiological reactions (tachycardia, increase in blood pressure) following recollection of trauma exposure.
– Criterion C: avoidance of stimuli that may recall serious events, both in the form of memories and thoughts of the person, but also attempts to avoid external stimuli, such as people, places, specific situations that may evoke associations with the trauma.
– Criterion D: negative mood changes that begin or intensify after a traumatic event – these include inability to remember important aspects of the event, distorted beliefs and expectations about self and the world, blaming self or others for the trauma experience, persistent negative emotional states (fear, anger, shame), loss of interest, feeling alienated, and increasing difficulty feeling positive emotions.
– Criterion E: changes in arousal and reactivity – difficulty controlling emotions, reckless or self-destructive behavior, hypervigilance, excessive startle response, concentration problems, and sleep disturbances.
– Criterion F: duration – persistence of symptoms of Criteria B-E for more than 1 month.
– Criterion G: the disorder causes functional impairment in various life domains, including social and occupational domains.
– Criterion H: the disorder is not due to substance use, medication, or other illness [9].
Posttraumatic stress disorder may also be associated with the development of other comorbidities such as obesity, cardiovascular disease, autoimmune disease, or irritable bowel syndrome [10–13]. Studies have also shown that middle-aged women with co-occurring PTSD and depression are four times more likely to die from diabetes, cardiovascular disease, and unintentional injury compared to women in the healthy population, and have a higher risk of committing suicide [14]. PTSD not only contributes to a worsening somatic condition, but can also affect interpersonal relationships, education and employment, and social support [15, 16].
There are several medical factors that can help a clinician in diagnosis. First of all, neuroimaging techniques appear to be useful in the diagnosis of PTSD, which will be elaborated on further [17]. In addition, increased central norepinephrine levels with decreased regulation of central adrenergic receptors and chronically decreased glucocorticoid levels with increased regulation of their receptors were observed in these patients [18, 19]. In the treatment of post-traumatic stress disorder, according to guidelines, drugs from the group of serotonin reuptake inhibitors (SSRIs) such as sertraline, paroxetine, fluoxetine, and venlafaxine, as well as cognitive-behavioral therapy, remain the first-line therapy [20, 21]. Treatment of nightmares with prazosin is still under discussion, and there are no specific recommendations for its use [20]. Studies have also shown that effective pharmacological agents in the treatment of PTSD include risperidone and topiramate, in addition to those already mentioned [22]. In addition to pharmacological methods, cognitive behavioral therapy (CBT), cognitive therapy, eye movement desensitization and reprocessing (EMDR), and long-term psychotherapy remain interventions with proven efficacy, as positive results are observed not only in the acute phase of treatment, but in a few cases there is also the prospect of further improvements after the completion of treatment [23]. A meta-analysis showed significant effects of group psychotherapy in reducing PTSD symptoms compared to control groups, particularly in the area of cognitive behavioral therapy, also noting that age and type of trauma were predictors of effects in treating PTSD symptoms [24]. In addition, individuals unrelated to the military industry have been reported to benefit significantly more from psychotherapy than veterans and soldiers. In these populations, which are among the most vulnerable groups to developing PTSD, exposure and cognitive processing therapies are thought to have greater benefit compared to EMDR and stress management-focused therapies. Interestingly, this study also showed a correlation between lower treatment benefit at low and high levels of PTSD compared to intermediate levels of PTSD [25].
Treatment methods for PTSD include desensitization, which consists of creating realistic beliefs about the stressful stimulus, unlearning negative associations with the stressor or a particular situation, and desensitizing participants through repeated exposure to stress-inducing stimuli [26]. One of the therapies recommended by the Veterans Affairs/Department of Defense (VA-DOD) is stress management therapy, which focuses on techniques and strategies to reduce stress levels as well as coping skills for situations that may cause escalation of stress [27].
Focal brain simulation may be a promising method for treating PTSD symptoms. Studies do not provide a clear answer as to the full efficacy of this method, but downregulation of fear learning, salience, and threat detection circuits (i.e., areas for which structures such as the insula, amygdala, and anterior cingulate cortex are responsible) and concurrent upregulation of emotion and executive functions and contextual processing (structures of the hippocampus and prefrontal cortex) may be indirectly useful in responding to the treatment of patients’ stressful symptoms [28].
Neuroimaging techniques and neuroimaging in psychiatric disorders
The development of advanced imaging techniques has made it possible to study in great detail not only the structure but also the function of the brain. Magnetic resonance imaging (MRI) appears to be an ideal technique for assessing the anatomy of the brain because the images are of high quality and this procedure is noninvasive. MRI methods can be used to determine the size or shape of various structures in the brain and detect neuroanatomical abnormalities, particularly applying volumetric techniques [29]. MRI-based diffusion tensor imaging (DTI) can be used to assess the integrity of white matter tracts. In addition, DTI assesses in detail anatomical microstructures and pathological dysregulation in the white matter area, and with this technique it is possible to observe altered diffusion patterns in the brain that may occur in response to trauma [30]. Functional neuroimaging techniques use regional cerebral blood flow based on changes in the concentration of oxygen content in the blood using MRI contrast dependent on blood oxygen content (BOLD) in functional MRI (fMRI) [31]. It allows dynamic measurement of brain activity at rest or during a cognitive, emotional, or pharmacological challenge. In addition to the above techniques, there are also methods that use radioactive tracers (radiolabeled water, oxygen, or glucose), such as positron emission tomography (PET) or single photon emission tomography (SPECT) [32]. Magnetic resonance spectroscopy (MRS) is used to assess biochemical metabolites and their changes from the brain, and can also indicate subtle changes that are not visible when using the standard magnetic resonance imaging technique. This tool has the potential to elucidate the basis of PTSD and unravel the role of biomarkers used for risk monitoring, diagnosis or treatment [33].
Despite significant advancements in neuroimaging techniques for psychiatric disorders, excluding neurocognitive disorders, the impact of neuroimaging on the diagnosis and treatment of individual patients has not been substantial. This limitation may arise from imaging studies lacking the requisite specificity and sensitivity to identify individual disease entities effectively [34]. For instance, neuroimaging tests do not meet the criteria for useful diagnostic biomarkers, requiring at least 80% sensitivity and specificity in detecting mental disorders, distinguishing between different disorders. Additionally, the biomarker should be reliable, reproducible, non-invasive, cost-effective, and validated by independent research groups, with results published in peer-reviewed journals [35].
Conversely, neuroimaging in mental illness can prove beneficial in implementing therapies by detecting blood-brain barrier penetration and evaluating whether the potential study subjects will experience the expected therapeutic effects and benefits from specific compounds [36].
Recent studies have revealed that neuroimaging in schizophrenia can identify differences in brain structure and functioning as a response to treatment [37]. Notably, a stronger response to antipsychotics in treating paranoid syndrome correlates with higher baseline brain activation in the anterior cingulate cortex, superior temporal gyrus, and temporoparietal junction. Conversely, lower gray matter volume is associated with a weaker response to antipsychotic treatment [38, 39]. Analysis of imaging studies in individuals with schizophrenia indicates that cortical reserve has cognitive and clinical implications for those using behavioral therapy to enhance social cognition and memory strategies [40].
In anxiety disorders, brain function studies indicate heightened amygdala activity in individuals experiencing anxiety after exposure to certain stimuli [41]. Furthermore, other brain regions such as the anterior cingulate cortex and the insula, collectively referred to as the “web of fear”, are implicated in fear perception across all anxiety disorders (phobias, post-traumatic stress disorder) [42]. SPECT has demonstrated decreased metabolism in the left inferior parietal lobe during panic attacks, along with altered cerebral blood flow patterns, including higher glucose uptake in specific regions (amygdala, hippocampus, thalamus, pons, medulla, cerebellum, and midbrain). Cerebral blood flow asymmetry and a right hemisphere shift correlate with symptom severity [43]. MRS in panic disorder patients with panic attacks indicates decreased γ-aminobutyric acid (GABA) concentrations in the occipital cortex, with low baseline GABA levels correlating with poor therapeutic responses to alprazolam and imipramine (from the tricyclic antidepressant group) [44].
MRI studies in individuals with bipolar disorder suggest that illness expression may relate to hyperconnectivity between affect-processing regions, hyperactivation, decreased sensorimotor network connectivity, and reduced regulatory input from prefrontal cortex regions involved in cognitive control. Consequently, hyperconnectivity between specific brain regions may serve as a diagnostic feature of treatment resistance in patients with bipolar affective disorder [45].
The field of neuroimaging has witnessed significant advancements, enabling detailed exploration of both the structure and function of the brain. Among the various techniques available, MRI stands out as an ideal method for assessing brain anatomy due to its noninvasive nature and high-quality imaging. Volumetric techniques, applied within MRI, allow for the determination of the size and shape of different brain structures, aiding in the detection of neuroanatomical abnormalities [29].
Furthermore, MRI-based diffusion tensor imaging (DTI) offers insights into white matter tracts and their integrity, facilitating the assessment of anatomical microstructures and pathological dysregulation in response to trauma [30]. Functional neuroimaging techniques, such as fMRI, utilize regional cerebral blood flow changes, measured through blood oxygen content (BOLD) contrast in MRI, to dynamically capture brain activity during various states, including rest or cognitive, emotional, or pharmacological challenges [31].
In addition to MRI-based techniques, radioactive tracers are employed in such methods as PET or SPECT [32]. MRS adds another dimension by assessing biochemical metabolites and detecting subtle changes not visible in standard MRI, offering potential insights into the basis of PTSD and the role of biomarkers in risk monitoring, diagnosis, or treatment [33].
Despite substantial progress in neuroimaging techniques for psychiatric disorders, excluding neurocognitive disorders, their impact on individual patient diagnosis and treatment has been limited. Challenges arise from the lack of specificity and sensitivity in imaging studies to effectively indicate individual disease entities [34]. Diagnostic biomarkers, meeting criteria such as at least 80% sensitivity and specificity, reliability, reproducibility, non-invasiveness, cost-effectiveness, and validation by independent research groups, remain elusive [35].
Conversely, neuroimaging in mental illness proves valuable in implementing therapies, such as assessing blood-brain barrier penetration and predicting therapeutic effects [36].
Recent studies in schizophrenia highlight neuroimaging’s potential to identify differences in brain structure and functioning in response to treatment [37]. A stronger response to antipsychotics is associated with higher baseline brain activation in specific regions, while lower gray matter volume correlates with a weaker response [38, 39]. Imaging studies in individuals with schizophrenia underscore the cognitive and clinical implications of cortical reserve in those using behavioral therapy to enhance social cognition and memory strategies [40].
In anxiety disorders, neuroimaging reveals heightened amygdala activity after exposure to certain stimuli, with the “web of fear” involving the anterior cingulate cortex and insula [41, 42]. SPECT in panic disorder indicates altered cerebral blood flow patterns, with specific regions showing higher glucose uptake. Cerebral blood flow asymmetry and right hemisphere shift correlate with symptom severity [43]. MRS in panic disorder patients points to decreased GABA concentrations in the occipital cortex, impacting therapeutic responses [44].
For bipolar disorder, magnetic resonance imaging studies suggest hyperconnectivity between affect-processing regions, hyperactivation, decreased sensorimotor network connectivity, and reduced regulatory input from prefrontal cortex regions involved in cognitive control. This hyperconnectivity may serve as a diagnostic feature of treatment resistance [45].
Neuroimaging insights into PTSD
Neuroimaging studies have shed light on structural changes in the brain associated with PTSD, focusing on key regions such as the amygdala, hippocampus, and prefrontal cortex [46]. Commonly employed techniques include computed tomography (CT) and MRI, encompassing MRI volumetry for structural assessment and functional MRI for task-related brain activation [47].
The amygdala, a limbic system component located in the temporal lobe, comprises distinct nuclei with various functions, including fear regulation, aggression, and social behaviors [48]. Studies have demonstrated hyperactivity of the amygdala in association with anxiety disorders, positively correlating with PTSD symptom severity. Magnetic resonance imaging has revealed a significant decrease in amygdala volume among PTSD patients compared to controls, with no correlation found between volume and chronicity of the disorder [49–52]. Inconsistent reports exist regarding amygdala volume in PTSD, although meta-analysis results show no significant differences [53, 54]. Both the amygdala and the hippocampus play crucial roles in maintaining traumatic memories. Notably, volumetric changes in the amygdala associated with PTSD development can be reversed with effective pharmacological treatment, particularly serotonin reuptake inhibitors (SSRIs) [55]. Detailed studies indicate that decreased volumes in specific amygdala nuclei, including central and medial nuclei, as well as basolateral nuclei, correlate with PTSD symptom severity 24–36 months after injury [56]. Furthermore, emotional numbness and reduced reactivity to pain in PTSD may be linked to decreased amygdala reactivity in veterans exposed to traumatic stimuli [57].
PTSD also affects the hippocampus, contributing to memory deficits and challenges in fear learning [58]. Heterogeneous reports exist regarding hippocampal volume, with evidence suggesting a reduction associated with PTSD [59]. Long-term stress exposure may lead to hippocampal damage through elevated glucocorticoid levels, though it remains unclear whether reduced hippocampal volume is a cause or consequence of PTSD [46]. Childhood trauma studies, however, do not consistently support lower hippocampal volumes [60].
The resting-state network, central executive network, and salience network are implicated in PTSD symptomatology. Dysfunctions in these networks may contribute to avoidance, dissociation, cognitive deficits, and emotional control difficulties observed in PTSD [61–64]. Few studies have explored volumetry of the anterior insula, a component of the salience network [65].
Gender differences in brain structure changes have been identified, with males experiencing loss of gray matter in limbic regions, including the prefrontal cortex, and reduced hippocampal and amygdala volumes [66]. In contrast, females may exhibit amygdala hyperactivity and enlargement, as well as decreased connectivity between vital centers [67]. Functional MRI studies suggest that resting-state network connectivity variability correlates with PTSD symptom severity after trauma exposure [68].
Additionally, SPECT studies indicate potential diagnostic utility, distinguishing PTSD from traumatic brain injury based on cerebral perfusion patterns [69, 70].
Discussion
To date, there have been very few studies examining cerebellar function in PTSD. Recent reports describe that veterans suffering from PTSD show reduced cortical thickness, especially in the frontal and temporal lobes, with no tendency to lateralization. In addition, a decreased volume of the caudate nucleus and right hippocampus relative to the total volume of the brain was found, and, what seems to be a relatively new finding, an enlargement of several cerebellar lobes relative to their total volume [71].
In the group of adolescents presenting with PTSD, a tendency for abnormal development of the anterior limbic lobe was noted compared to adolescents not presenting with symptoms of PTSD. In addition, a decrease in the volume of the hippocampus, an increase in the reactivity of the amygdala, and a decrease in the coupling of the amygdala with the prefrontal body were found with increasing age [72].
It is also interesting to note that methylation of the SKA2 gene has been identified as a promising biomarker of suicide attempt risk, which may also be associated with the experienced symptoms of posttraumatic stress. Neuroimaging studies conducted on a group of white males who had participated in armed conflicts in Iraq and Afghanistan demonstrated that an association between PTSD symptom severity and SK2adj DNA methylation that was negatively correlated with cortex thickness in the anterior pole and superior frontal gyrus regions, as well as the right orbitofrontal cortex and the right inferior frontal gyrus [73].
Stress coping mechanisms can be distinguished from resilience, which is defined as a process of adaptation in the context of significant life difficulties. The number of studies describing neuroimaging of immunity is still small, but the implications of the existing reports seem promising [31]. Neuroimaging allows the correlation of adaptive and non-adaptive behaviors and enables the assignment of correlates to biological factors and their interaction with environmental and psychological factors, but also facilitates the study of mechanisms that influence the emergence of these interactions [74]. To identify the phenomenon of immunity and return to normal functioning after stress exposure, a study conducted in 2010 used magnetic resonance technology to investigate the consequences of experimentally induced stress in healthy individuals. In patients exposed to moderate stress induced by watching aversive movies, prolonged activation of the amygdala communication network was observed, which could be responsible for the heightened state of hypervigilance that impairs memory processing of stimuli after the experienced stress [75]. Despite the fact that resilience can be an interesting mechanism in the context of stress management, even after traumas suffered in the past, there are very few studies in which researchers evaluate the integrity of the white matter or the volume and thickness of the gray matter, since the existing reports focus on the analysis of the structure and its changes mainly in the case of the hippocampus and the amygdala [31]. Studies in animal models have shown that interventions aimed at reducing the stress response contribute to an increase in the volume of the ventral medial prefrontal cortex (mPFC) and to an increase in hippocampal neurogenesis [76]. In the assessment of white matter using DTI, it was found that changes in this structure in the limbic system occur mainly with an adaptive background, e.g. in personnel exposed to stress during surgery, while changes specifically related to PTSD were not observed [30].
Another important aspect where neuroimaging can provide interesting results and therapeutic benefits is the evaluation of brain structures in imaging studies in relation to the pharmacotherapy and/or psychotherapy applied. The studies conducted have attempted to detect changes in the brain in individuals taking medications from the serotonin reuptake inhibitor (SSRI) group and benzodiazepines, which seems to be particularly important in the case of PTSD, since these substances are often used in patients struggling with this disorder due to the symptoms they produce [77]. Published reports have shown that long-term treatment with escitalopram reduced amygdala activation in the assessment of emotional expression of faces presented to study participants [78]. On the other hand, a 20 mg dose of paroxetine given to study participants for 1 month resulted in hypoactivation of the left prefrontal lobe and the right frontal lobe of the medial premotor cortex [79]. The results of these studies suggest that the use of antidepressants may affect the processing of emotions in specific brain regions in the early phase of treatment. The observed increase in hippocampal volume following the use of appropriate pharmacotherapy in patients with PTSD correlated with the reduction in symptoms they experienced [77]. The literature reports that SSRIs contribute to the modulation of neurogenesis and are able to reverse the negative effects of stress on hippocampal atrophy [80].
Another study that demonstrated the effectiveness of psychotherapy in patients with PTSD symptoms used electroencephalography (EEG) [81]. Greater activation of the right hemisphere was observed when viewing images related to trauma, not only in patients suffering from PTSD but also in healthy control participants. After applying cognitive behavioral therapy (CBT), a reduction in right hemisphere activation in the frontal areas was observed, resulting in a reduction in symptoms [82]. Similarly, in another study using the EEG technique, subjects suffering from post-traumatic stress disorder initially showed a tendency toward increased activation of the orbitofrontal and anterior cingulate cortex, bilateral parahippocampal gyrus, and bilateral posterior cingulate cortex when listening to a trauma replay scenario. After successful treatment with eye movement desensitization (EMDR) and reprocessing therapy, EEG analysis showed increased cortical activity and decreased connectivity between the left visual cortex and right fusiform gyrus [83]. Therefore, it was hypothesized that successful treatment would normalize processing [81].
Recent randomized, multicenter, double-blind, placebo-controlled clinical trials have shown that therapy with 3,4-methylenedioxymethamphetamine (MDMA) is highly effective in severe PTSD patients, while the treatment itself is well tolerated and not associated with significant side effects, even in patients with severe PTSD and comorbidities [84]. Recent reports have shown that MDMA likely reduces the fear response by enhancing the sense of extinction, and also modulates brain regions such as the hippocampus, insula, and amygdala that are involved in the hyperactive fear response in post-traumatic stress disorder. In neuroimaging studies, this is reflected in increased connectivity between the amygdala and the hippocampus and insula, as well as in the left amygdala-left posterior cingulate cortex, left amygdala-right posterior cingulate cortex, left amygdala-left insula, and left cingulate isthmus-left posterior hippocampus connections [85].
The integration of neuroimaging techniques in research on PTSD continues to produce intriguing insights. Beyond the well-established alterations in cortical thickness and subcortical volumes observed in individuals with PTSD, a noteworthy observation emerges from recent investigations into cerebellar function. Surprisingly, an enlargement of several cerebellar lobes relative to their total volume has been identified, adding a novel dimension to our understanding of the neural correlates of PTSD [71]. This uncharted territory in cerebellar involvement prompts further exploration, as it underscores the complexity of the disorder and suggests potential connections between the cerebellum and established structures implicated in PTSD pathology. The expanding scope of neuroimaging not only clarifies existing structural abnormalities but also encourages researchers to investigate unexplored neural territories, potentially paving the way for more targeted therapeutic interventions and a comprehensive understanding of the disorder’s neurobiological underpinnings. Clinicians must remember that PTSD is a real issue that can affect people from all walks of life, and can be linked to decreases in quality of life. Therefore, thorough exploration of diagnostic and treatment options is crucial [86, 87].
Limitations
As narrative reviews rely heavily on the author’s interpretation and subjective judgment, the selection of studies, data extraction, and synthesis of findings are influenced by the author’s biases, preferences, or preconceived notions. Also, unlike systematic reviews or meta-analyses, this type of study does not follow a predefined protocol or rigorous methodology for study selection or data extraction. Narrative reviews often lack a standardized quality assessment of included studies and may be more susceptible to publication bias, as they often rely on published studies. Another potential limitation is that whereas neuroimaging in PTSD can be described in very specific ways, in this narrative review we tried to provide a broad overview of the topic, which might have resulted in a lack of depth and detail compared to more focused or specialized reviews. However, despite these limitations, this narrative review about neuroimaging in PTSD is useful for generating hypotheses as well as summarizing existing knowledge.
Conclusions
Neuroimaging emerges as an indispensable tool for diagnosing and correlating PTSD symptoms with discernible alterations in specific brain regions. There has been a notable focus on critical areas such as the hippocampus, amygdala, insula, anterior cingulate cortex, and prefrontal cortex, while also considering interconnected brain networks including the central executive network, salience network, and resting state network. However, interpretations stemming from the conducted research exhibit some inconsistency, highlighting the need for further exploration.
The observed reduction in hippocampal volume may signify a potential predisposing factor for PTSD onset or a consequence of trauma exposure, although the simultaneous existence of both scenarios cannot be definitively excluded. Alterations in amygdala structure suggest a complex interplay of factors during PTSD symptom manifestation, involving heightened amygdalar activity and increased functional connectivity within the salience network. The reduced activity in the prefrontal cortex may indicate heightened sensitivity to stimuli, a disruptive symptom characteristic of individuals with PTSD.
Moreover, the inconclusive nature of current findings serves as a catalyst for additional research aimed at refining our comprehension of the intricate neurobiological mechanisms underpinning PTSD. Despite the existing limitations, neuroimaging studies show promise in predicting responses to PTSD treatment, particularly with cognitive behavioral therapy. Future endeavors should strive to address prevailing gaps, bolster methodological rigor, and contribute to the establishment of more robust conclusions in the domain of neuroimaging and PTSD research.