Introduction
Due to the outbreak of the pandemic caused by the SARS-CoV-2 virus, there have been fundamental changes to the operation of healthcare facilities across the world [1–3]. The rapid increase in patient admissions due to COVID-19 forced a restructuring of hospital services and the redeployment of staff to ensure the delivery of optimal clinical care [4–7]. In many countries, non-urgent elective treatments were been postponed, due to staff and infrastructure constraints, and concerns about exposing potentially vulnerable patients to infection [8]. In Poland, according to the recommendations in force during the COVID-19 pandemic, services in the fields of cardiology, oncology, and other clinical areas where the delay of implementation of treatment could have a negative impact on prognosis, should be provided without interruption. In order to minimize the risk of transmission of COVID-19 infection and to provide additional hospital beds for patients requiring urgent hospital admission due to COVID-19 infection, the Polish National Health Fund (NFZ) recommended the limiting of clinical services to the minimum required or the temporary suspension of the provision of planned services [9, 10]. Due to concerns about contracting COVID-19, it is noted that in Poland, patients with cardiovascular diseases (CVD), irrespective of their symptoms, often did not call emergency teams and exhibited reduced reporting of symptoms to medical facilities, which was particularly noticeable in the case of myocardial infarction [11].
In 2020, according to the estimates of the Polish Cardiac Society (PTK), only 12–18% of patients with ACS were eligible for the coordinated care programme for patients after ACS (KOS-Zawal), as confirmed by the analyses of the present study. Delivery of treatment and care, including cardiac rehabilitation, under the KOS-Zawal programme has become increasingly difficult, as confirmed by our study [12]. KOS-Zawal provides both medical care (diagnostics and interventional treatment) and cardiac rehabilitation for up to 12 months after an ACS. The primary aim of developing and implementing new models of coordinated medical care was to improve its quality, increase patient satisfaction and reduce the risk of future cardiovascular events. A key objective was to improve mortality and morbidity after myocardial infarction, and this was enabled by the increased frequency and time of complete myocardial revascularisation, improvement in access to services and, where appropriate, implantable devices, increasing access to cardiac rehabilitation programmes, particularly those performed on an outpatient basis, facilitating access to consultations with a cardiologist and reducing delays in the performance of individual procedures [13, 14]. Studies conducted in 2017 and 2020, following the introduction of the KOS-Zawal programme, have shown a favourable trend in terms of reduced mortality in this group of patients [13]. Research by Kubielas et al. showed that a comprehensive and multidisciplinary KOS-Zawal managed care programme reduced the risk of death in post-ACS patients by approximately 29–30% [13]. In addition, it is important to emphasize that the results of the programme have also increased the sense of safety among patients covered by the KOS heart attack programme [15]. As a priority action, the NFZ recommends strengthening preventive measures for modifiable factors of ischaemic heart disease and increasing access to early cardiac rehabilitation [16].
This favourable trend was disrupted by the SARS-CoV-2 virus; therefore, the aim of this study was to assess the impact of the COVID-19 pandemic on patient management and cardiovascular disease outcomes including acute coronary syndrome, for patients treated within the KOS-Zawal programme and a group of patients treated outside of the programme between 2017 and 2022.
Material and methods
Study design and participants
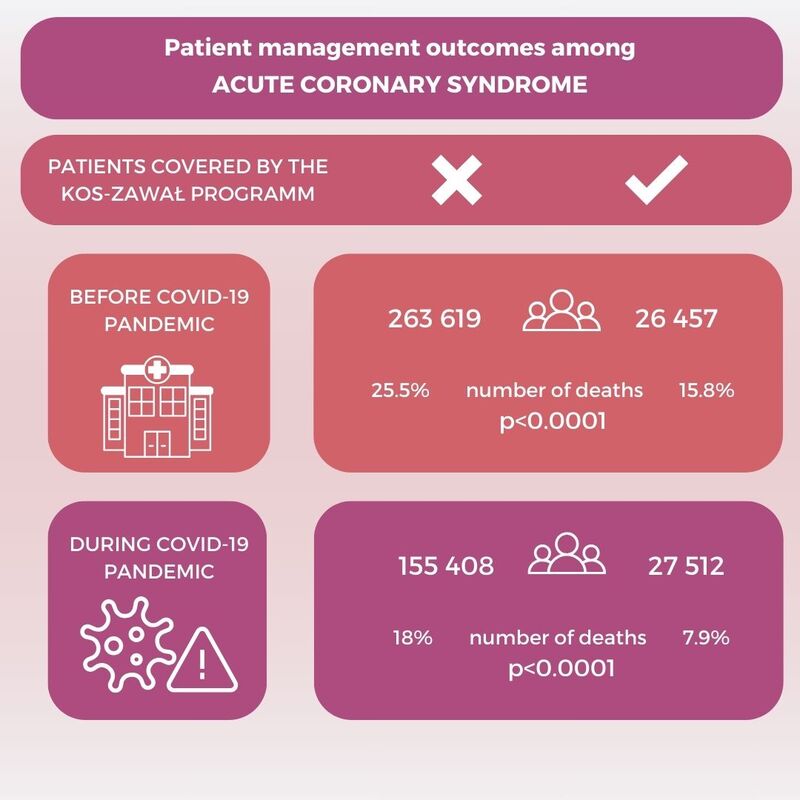
This study analysed patient data from two distinct periods to assess the impact of the COVID-19 pandemic on outcomes for patients with and without coverage under the KOS-Zawal programme. The pre-pandemic period, from October 1, 2017, to March 31, 2020, included 263,619 patients not covered by the KOS-Zawal programme and 26,457 patients covered by the programme with myocardial infarction. The pandemic period, from April 1, 2020, to March 31, 2022, included 155,408 patients not covered and 27,512 patients covered by the KOS-Zawal programme. Participants included in this comparative study were diagnosed with acute coronary syndrome (ACS). Eligibility required that participants be adults aged 18 years or older with comprehensive medical records and adequate follow-up data available for the entire study duration. Patients with incomplete medical records or insufficient follow-up data were excluded to ensure the accuracy of mortality rates and the effectiveness of assessment of the KOS-Zawal programme.
Ethical statement
All methods were carried out in accordance with the relevant guidelines and regulations. Ethical review and approval for the study were waived because we did not collect personal data and did not involve laboratory tests or medical interviews; therefore, we did not require the consent of a bioethical committee according to Polish national legislation.
Statistical analysis
Descriptive data were presented as the number of observations and percentage or as mean and standard deviation (x ± SD). The χ2 test and Student’s t test were performed for statistical comparisons. Data were analysed using Microsoft Excel Professional 2016 (Microsoft, Redmond, WA, USA), R software version 3.6.1 (R Foundation, Vienna, Austria) and Statistica v.13.3 (Tibco Software Inc., Palo Alto, CA, USA).
Results
In the pre-pandemic period (October 2017-March 2020), the mean age in the two groups was between 66 and 68 years, with the majority being male (61.0% and 68.4%, respectively). In the pandemic period (April 2020–March 2022 period), men made up a significant majority of patients in the two study groups (62.7% and 69.7%, respectively), and the mean age was in the 73–75 years range. The described data were collected and reported by the NFZ. Data related to the comprehensive care after MI (KOS-Zawal) were collected and reported from October 2017. Table I shows the demographic characteristics of the two groups of patients in the two time periods.
Table I
Characteristics of patients not covered and covered by KOS-Zawal in the following time periods: 1st October 2017 to 31st March 2020 and 1st April 2020 to 31st March 2022
Mortality among patients from 1 October 2017 to 31 March 2020
During the pre-pandemic period from October 1, 2017, to March 31, 2020, the mortality rate was observed to be significantly higher in the group of patients not covered by the KOS-Zawal programme compared to those who were covered. Specifically, the mortality rate in the non-covered group was 25.5% versus 15.8% in the covered group, a statistically significant difference (p < 0.0001). This disparity highlights the potential impact of the comprehensive care provided under the KOS-Zawal programme. Table II shows data on patient deaths in the groups of patients covered and not covered by KOS-Zawal.
Table II
Number of deaths within 365 days of the first hospitalisation in the patients not covered and covered by KOS-Zawal from 1 October 2017 to 31 March 2020
Mortality among patients from 1 April 2020 to 31 March 2022
During the COVID-19 pandemic, between 2020 and 2022, the number of patients not covered by KOS-Zawal decreased to 155,408 people, of whom 28,018 (18.0%) died (Table III). Over the same period, the number of patients covered by KOS-Zawal increased to 27,512 people, of whom 2,177 (7.9%) died. Similar to the earlier time interval, there was a statistically significant higher incidence of death in the group of patients not covered by KOS-Zawal compared with covered patients (p < 0.0001). Compared to the earlier time interval of 1st October 2017 to 31st March 2020, in the period 1st April 2020 to 31st March 2022 the number of deaths among patients not covered by KOS-Zawal decreased significantly by a factor of 0.7, and among patients with KOS-Zawal, the number of deaths decreased significantly by a factor of 0.5 (p < 0.0001 for both patient groups). Mortality among patients not covered by KOS-Zawal was significantly higher than among covered patients, in both the male and female subgroups (p < 0.0001 for both subgroups) (Table III).
Table III
Number of deaths within 365 days of the first hospitalisation in the patients not covered and covered by KOS-Zawal in time period 1 April 2020 to 31 March 2022
Comparative analysis of mortality of patients in two time periods: from 1 October 2017 to 31 March 2020 and from 1 April 2020 to 31 March 2022
The data comparison between the two distinct periods – before and during the COVID-19 pandemic – reveals significant changes in mortality rates across both groups of patients. Specifically, the mortality rate in the group not covered by the KOS-Zawal programme showed a reduction from 25.5% in the pre-pandemic period to 18% during the pandemic (Table IV). Similarly, the mortality rate for patients covered by the KOS-Zawal programme decreased from 15.8% to 7.9% over the same periods (Table V). These changes reflect a reduction in the absolute mortality rates by 7.5% and 7.9% for the non-covered and covered groups, respectively, indicating substantial improvements in survival rates during the pandemic period.
Table IV
Comparative analysis of mortality of patients not covered by KOS-Zawal programme in time periods: 1 October 2017 to 31 March 2020 and 1 April 2020 to 31 March 2022
Table V
Comparative analysis of mortality of patients covered by KOS-Zawal programme in time periods: 1 October 2017 to 31 March 2020 and 1 April 2020 to 31 March 2022
The statistical significance of these reductions is high (p < 0.0001 for both comparisons), suggesting that both groups experienced improvements, but the extent of mortality reduction was notably greater in the group receiving coordinated care under the KOS-Zawal programme. Data detailing these shifts in mortality rates are comprehensively tabulated in Tables IV and V, which provide a detailed breakdown of the mortality figures for each time frame and patient group.
Discussion
Survival analysis of patients receiving comprehensive cardiac care during the pandemic period is extremely important to assess the effectiveness of interventions and identify potential areas for improvement.
The study focuses on a critically important area of health care delivery during the COVID-19 pandemic – cardiac care for patients with ACS. Given the substantial restructuring of healthcare services to accommodate COVID-19 patients, understanding the impacts on other urgent medical conditions such as ACS is crucial. The research emphasizes the effect of continuous and coordinated cardiac care on mortality rates during such disruptive times [14, 17]. The unmet needs in Polish cardiology during the COVID-19 pandemic, especially in its early phase (2020–2021), primarily stem from the patients’ fear of contacting the healthcare system due to concerns about becoming infected with SARS-CoV-2. Due to the pandemic, healthcare systems were required to undertake extensive reorganization, including that of hospital wards, units, and medical staff, as well as reallocating equipment and supplies from other departments to care for COVID-19 patients [1]. Decisions made by patients to delay seeking help or contacting a doctor, particularly in the context of acute coronary syndromes, deprive them of opportunities for a full recovery. The observed trend of a significant decrease in the incidence of acute coronary syndromes during the period 2020–2022 confirms researchers’ concerns. An essential factor from the perspective of public health management appears to be the substantial burden on the system due to symptomatic COVID-19 patients requiring intensive care in anaesthesia and intensive care units. The logistical burden, not only on hospital services but also on limited access to primary healthcare and virtually minimal access to ambulatory specialist care, shapes the unmet needs in this area [10, 18]. This study stands out by specifically examining the differences in outcomes between patients enrolled in the KOS-Zawal programme and those who are not, during the pandemic. While other studies have generally addressed the broad impacts of COVID-19 on healthcare systems or on cardiac care, this study provides a direct comparison of survival rates within a well-defined patient population before and during the pandemic, offering insights into the effectiveness of the KOS-Zawal care model under crisis conditions [19–23]. The overwhelming focus on handling COVID-19 cases led to reduced attention and capacity for other essential medical services, including cardiology care [20]. Reports from the USA, China, Spain, Italy, and Germany indicate that the COVID-19 pandemic has resulted in a substantial decline in the number of interventional cardiology procedures being performed [19, 21–23].
Recently published research assessing the impact of the COVID-19 pandemic on non-COVID-19 cardiovascular care and outcomes showed a decrease in hospital admissions, diagnostic tests and procedures related to cardiovascular disease treatment, as confirmed by the results of our study [24]. As a consequence of these challenges, addressing the unmet needs in Polish cardiology after COVID-19 should be a priority in healthcare planning and resource allocation. This is also consistent with a meta-analysis which demonstrated a 20% decrease in STEMI hospitalisations across the world at the time of the pandemic [25].
The resilience of the KOS-Zawal programme during the COVID-19 pandemic highlights its essential role in managing ACS under crisis conditions. The notable decrease in mortality among patients within the programme, contrasted with those outside it, underscores the protective impact of structured and continuous care, particularly during health emergencies. These observations reinforce the value of comprehensive care programmes in significantly enhancing patient outcomes.
As global health systems face the dual challenges of the ongoing pandemic response and the need for routine medical care, the insights from this study underscore the importance of maintaining and expanding coordinated care frameworks [26–28]. Such systems not only mitigate the immediate impacts of health crises but also strengthen overall healthcare delivery, proving critical in sustaining patient care during and beyond such events.
The analysis relies on the availability and accuracy of the data collected during the pandemic. Any missing or incomplete data could potentially affect the robustness of the findings. The analysis covers a specific period during the COVID-19 pandemic. The findings may not reflect the long-term effects of the pandemic on patients with acute coronary syndrome. The study might be subject to selection bias, as it may only include patients who sought medical attention during the pandemic. Patients who did not seek care or were unable to access healthcare services during this period may not be adequately represented.
In conclusion, The COVID-19 pandemic greatly affected the KOS-Zawal programme, resulting in fewer patients being enrolled and higher death rates, which indicates serious problems in receiving cardiac care. Patients not covered by KOS-Zawal had even higher death rates, which shows the importance of the programme for protecting them during challenging times. Despite these difficulties, the programme managed to improve survival rates during the pandemic compared to before, suggesting that the programme’s improved strategies were effective. These findings highlight how greatly the pandemic impacted the management and outcomes of heart diseases, proving how crucial programmes like KOS-Zawal are during health crises. This study demonstrates the need for healthcare systems to develop and strengthen such programmes to better handle future global health emergencies.