Migraine is one of the most prevalent conditions associated with headaches. It is reported that, worldwide, 8.6% of men and 17.0% of women (over one billion people in total) suffer from migraine [1]. The International Classification of Headache Disorders, 3rd Edition (ICHD-3) distinguishes 3 main types of migraine: migraine without aura (MO), migraine with aura (MA), and chronic migraine [2]. Migraine, especially MA, responsible for approximately one-third of migraine cases, is often identified as one of the risk factors for cerebral infarction [3]. According to the study conducted by Schürks et al., the relative risk (RR) for ischaemic stroke in MA was increased over twofold (RR = 2.16). Moreover, vascular complications were more common among women (RR = 2.08), but the risk among men with migraine was also increased (RR = 1.37). The ICHD-3 presents 4 different migraine complications, including status migrainosus, persistent aura without infarction, migrainous infarction, and migraine aura-triggered seizures [2]. The third mentioned is a specific kind of cerebral infarction in which one or more aura symptoms persist for more than 60 min [4]. It can be distinguished from the other, persistent aura without infarction by neuroimaging, demonstrating ischaemic lesions in the relevant area. It occurs rarely, in less than one person per 100 thousand per year, and represents approximately 1% of all ischaemic strokes [4, 5]. The most affected group is young adults, and among them, under the age of 50 years, the percentage of all ischaemic strokes can reach as much as 20% [6]. Notably, the incidence is twice as high in women as in men [4]. Migrainous infarction is not often considered a common condition, especially among men. However, due to the high prevalence of migraine, clinicians should never forget this potential diagnosis in all young patients presenting with stroke.
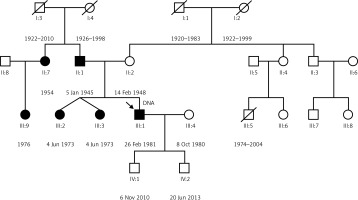
Herein, we present a case of a 34-year-old male patient admitted to the emergency department. Among the symptoms, the patient reported a severe headache (different and much more intense than ever before), numbness and weakness of the left extremities, and visual abnormality. As it was diagnosed during the following hospitalisation, the patient had suffered from similar attacks of hemiplegic migraine aura since the age of 15 years; however, he had never been diagnosed or treated prior. The previous migraine attack symptoms were less severe but also included non-visual aura manifesting as limb numbness and speech disturbances. Similar attacks were reported to happen to the patient’s 2 sisters, the father, and the father’s sister (Figure 1).
During the admission to the Neurological Department, the patient’s speech was normal. He suffered from non-specific visual disturbances, more severe on the left side, and mild sensory disturbances in the left hand and foot without asymmetry of muscle strength or reflexes. No pathological symptoms and no apparent cerebellar dysfunction were found in the neurological examination. Brain computed tomography conducted in the Emergency Room did not show any abnormalities. Other tests showed only elevated levels of cholesterol and triglycerides. The blood pressure was monitored, and elevated diastolic blood pressure was detected; however, ambulatory blood pressure measurements performed to monitor the patient’s blood pressure for 24 h showed no hypertension; therefore, no such diagnosis was made. Also, no signs of hypertensive angiopathy or retinopathy were found. In the heart ultrasound, there was no evidence of any abnormalities, especially patent foramen ovale (PFO). Consistently, in an examination with a contrast medium and transcranial Doppler ultrasound, no faults were found, and the carotid and vertebral arteries were healthy.
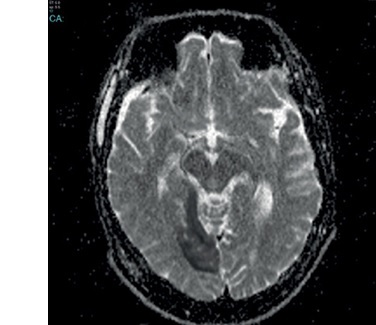
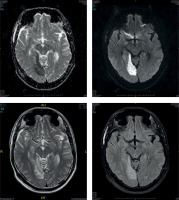
Initially, because there were no presumptions based on performed diagnostics to suspect a stroke, a familial hemiplegic migraine attack was diagnosed. However, the visual abnormality persisted. Therefore, brain magnetic resonance imaging (MRI) (Figure 2) was conducted, showing changes in the right temporal and occipital lobes. More precisely, neuroimaging presented a typical view of ischaemic lesions found in the right temporal lobe and right occipital lobe, but without a correlation with migraine aura symptoms in the left cerebellum. Thus, another diagnosis appeared to be highly probable: migrainous ischaemic stroke.
Considering MR images, it is worth mentioning that patients with a typical migraine course are likely to present some alterations from the typical radiological presentation of the healthy brain. Namely, lesions called white matter hyperintensities (WMHs) are more common in migraineurs than in healthy controls, especially in those having attacks with aura, being older, or suffering from chronic disorders, such as hypertension or diabetes mellitus [7]. Those observations remain consistent with the more frequent presence of WMHs in general in older patients or those suffering from hypertension [8]. Therefore, the analysis of WMHs in migraine patients requires caution, because other causes are more common. In migraine patients, WMHs tend to cumulate mostly in the infratentorial area and posterior circulation territory [9]. However, data about their presence in hemiplegic migraine are very limited, and possible differences with typical migraine patients are not sufficiently studied. One study performed on sporadic hemiplegic migraine patients showed no significant differences in the percentage of patients with WMHs in comparison to non-hemiplegic migraine patients, with a prevalence of approximately 50% in both groups [10]. However, compared to typical migraine changes, the hemiplegic migraine group presented more WMHs in the parietal lobe. Nevertheless, although interesting, these observations are insufficient to draw certain conclusions, and more research is needed. In our patient’s MR, WMHs were not described.
The patient was also consulted by an internal medicine specialist. Ophthalmological control, including field of view, was recommended. Other possible diagnoses were excluded. The clinical features, neuroimaging, additional tests, and further investigation were consistent with the diagnosis of migrainous infarction. The patient was discharged home under the continued care of the Neurology Department.
The association between migraine and stroke definitely is not a novel topic, as it has already been reported almost 50 years ago [11]. Since then, migraine has been repeatedly listed as one of the factors that elevate the risk of stroke, especially MA. Migrainous infarction is not considered a common complication; therefore, it can potentially be missed while diagnosing a young patient, especially a male with a stroke.
Differentiation between a stroke and prolonged aura, especially in the acute phase, may cause many difficulties on the clinical ground. It is essential to confirm the diagnosis by performing a brain MRI [12], which was performed in this case. The patient presented relevant neuroimaging changes consistent with the presented prolonged aura symptoms. Moreover, the ischaemic lesions were found during the migraine attack, which strongly supports migrainous infarction diagnosis in comparison to non-migrainous infarction. Also, what is worth emphasising that this diagnosis is promoted by the consistency between the location of lesions and aura symptoms, which is not typical for non-migrainous infarction. However, even when radiological findings correspond with clinical presentation, alternative causes of the observed signs and symptoms should be considered, such as mitochondrial encephalopathy and young-onset stroke of other causes. Therefore, electromyography was performed, and since no abnormalities were found, a muscle biopsy was waived. The electroencephalography showed mild changes in the right frontal and temporal lobes; however, they were not significant in this case. Blood samples for antinuclear antibodies (ANA), antineutrophil cytoplasmic antibodies (ANCA), and coagulation parameters were measured, and no significant changes were observed, suggesting no systemic disease. These findings reinforced the diagnosis of migrainous infarction.
The patient has been observed for 5 years. The exact frequency of attacks before the hospitalisation was not known; however, due to the significant number of attacks per month reported by the patient, prophylactic treatment was recommended, and he regularly took cinnarizine. Although more effective medications with fewer adverse events are currently the first choice in migraine prophylaxis [13], this case happened several years ago when such possibilities were not broadly available. Because of high lipid levels and as secondary prevention for the stroke, atorvastatin and acetylsalicylic acid were administered. Although hypertension was not diagnosed, propranolol has been proposed additionally because of its value in migraine prevention and bearing in mind an episode of very high blood pressure during the admission. The patient also continued his regular medication for depressive anxiety disorder, duloxetine. During the 5 years of observation, he suffered from only one attack, which probably happened because he stopped taking medication for one and a half months. No further complications were observed.
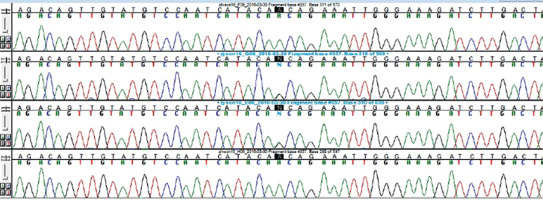
Although the understanding of migraine is still incomplete, it has been advancing rapidly in recent years [14]. The clinical presentation may be the result of an interaction of several different factors, including genetics, environment, and lifestyle [15]. Also, the link between migraine and stroke needs to be fully comprehended. Several mechanisms and theories have been suggested, including cortical spreading depression, vasoconstriction, shared genetic defects, vascular and cardiac abnormalities such as PFO and endovascular dysfunction, neurogenic inflammation, and hypercoagulability [16]. While none of the mentioned disorders was detected in the patient, the migrainous stroke diagnosis was confirmed. Genetic tests are not necessary for the diagnosis and are mainly used to verify the presence of mutations in other family members to detect disease risk. However, they were conducted in the presented case as part of a clinical trial and confirmed the mutation in the SCN1A gene (Figure 3). The diagnosis of familial hemiplegic migraine, type 3, according to the ICHD-3, was justified.
Figure 3
A1067T mutation in SCN1A. Exon 16 with flanking intronic regions of the SCN1A gene were analysed in the presented patient. The missense variant at chr2:166892788, g.37362G>A, c.3199 G>A, rs2298771 resulting in amino acid change A1067T was found
There is still much discussion around migraine and its complications. The presented case report shows the importance of family history and thorough anamnesis, as well as the crucial part of neuroimaging in differentiation between complications. Also, it highlights the multidimensionality of migraine with its genetic and familial intricacies. More and more genes associated with migraine, both in a monogenic and polygenic manner, are constantly being discovered. Possible linkages require further research. Notably, migraineurs are reported to have a lower quality of life [17], which also underlines another crucial issue in terms of the correct migraine treatment together with effective prevention and early diagnosis of its complications. It is important to remember the possible complications of migraine, such as migrainous infarction, because it can easily be mistaken for prolonged aura, while it can create long-lasting deficiencies. Finally, this case underlines the importance of prevention and control of stroke risk factors other than migraine, such as smoking, obesity, or oral contraceptive use, also among young patients suffering from migraine.