Cardiovascular disease (CVD) is a common clinical disease threatening human health, particularly among middle-aged and older individuals. It is characterized by high morbidity, high disability, and high mortality. CVD is a significant contributor to mortality, ranking among the leading causes of death [1]. In low- and middle-income countries, the average month-to-month treatment cost of stroke and coronary heart disease is between $300 and $1000 [2]. Therefore, formulating effective public health strategies to reduce the prevalence of cardiovascular diseases is of great significance for reducing the social and economic burden.
Visceral fat content is widely documented to be significantly linked to the advancement of cardiovascular disease [3]. Metabolic score for visceral fat (METS-VF) is a new visceral fat prediction index created by Mexican scholars in the past 2 years. It is constructed by indicators such as gender, age, height, weight, waist circumference, fast glucose, cholesterol: high-density lipoprotein cholesterol (HDL-c), etc. [4], and performs better than other synthetic visual fat indexes (VFI). Moreover, previous studies have confirmed that METS-VF has good prediction efficiency in predicting hypertension [5] and type 2 diabetes mellitus [6]. METS-VF may be strongly linked to cardiovascular events.
This study aims to establish a prospective cohort study using the China Health and Retirement Longitudinal Study (CHARLS) to examine the association between METS-VF and CVD, as well as the mediation role of triglycerides (TG) in the above relationship, and to visualize the results by building a decision tree model, ultimately providing insights for reducing the incidence of CVD.
Methods
Study population
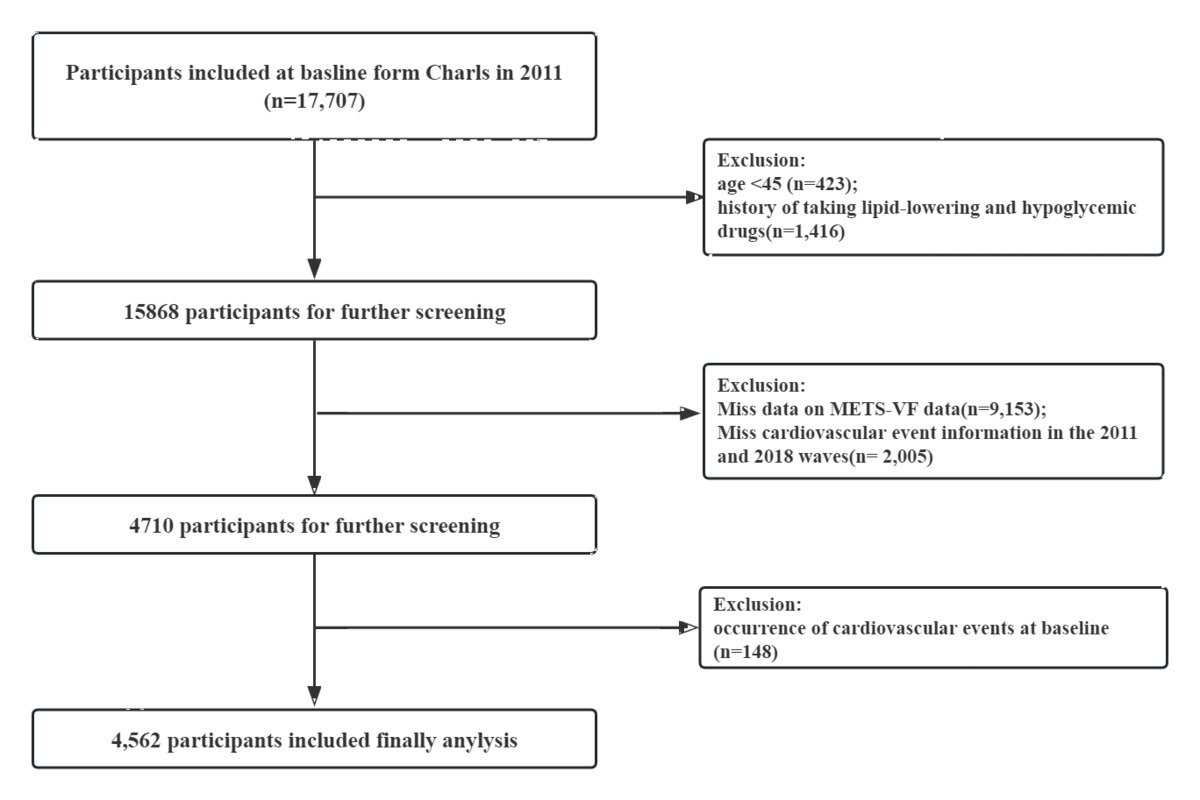
We used data from waves 1 to 4 (2011–2012 to 2018) of CHARLS survey, with wave 1 as the baseline. The survey covered 28 provinces (autonomous regions and municipalities) and 450 villages/communities, with a sample of 19,000 participants from 124,000 homes as of its completion in 2018. Of the 2011 baseline survey participants, 17,707 completed baseline physical examinations and questionnaire surveys. Among these participants, blood data were available for 11,847 individuals. A total of 13,145 participants were excluded based on the following specific criteria: age younger than 45 years old (n = 423), history of taking lipid-lowering and hypoglycemic drugs (n = 1,416), incomplete METS-VF data (n = 9,153), missing cardiovascular event information in the 2011 and 2018 waves (n = 2,005), and occurrence of cardiovascular events at baseline (n = 148).
Assessment of METS-VF
METS-VF = 4.466 + 0.011[(Ln(METS-IR))3] + 3.239[(Ln(WHtR))3] + 0.319(Sex) + 0.594(Ln(Age)). Age was represented in years, while gender was considered a binary response variable with a value of 1 for men and 0 for women. Body mass index (BMI) was calculated as BMI = weight (kg)/height2 (m2), waist to height ratio (WHtR) was calculated as WHtR = waist (cm)/height (cm), METS-IR and METS-VF were calculated as follows, METS-IR = (Ln((2 × Glu + TG) × BMI)]/Ln(HDL-c).
Assessment of incident stroke
Attendees reporting multiple heart disease or stroke episodes were recorded as having an incident CVD event (0 = no, 1 = yes). The secondary outcome includes heart disease and stroke as separate components of the primary result.
Assessment of covariates
Demographic characteristics (age, sex, educational level, marital status, and residential area) and health-related behaviors (smoking status, sleep time, and alcohol consumption frequency) were considered several potential factors that could influence residents’ CVD.
Statistical analysis
We evaluated various covariate combinations to control for confounding in the analysis with three models. Model 1 was the crude model, Model 2 was adjusted for age, gender, education, location, and marital status, while Model 3 further included sleep duration, smoking status, and alcohol consumption frequency. We then conducted a mediation analysis to assess METS-VF’s relationship with CVD, stroke, and heart disease, with TG as the mediator. We measured average direct effect, average causal mediation effect, and TG’s mediating impact. Decision trees identified high-risk CVD populations, and METS-VF’s incremental predictive value was calculated to evaluate its contribution to predicting CVD and related diseases. Statistical analyses were performed in R 4.1.3 using the “rms” package for restricted cubic splines and the “rpart” package for decision trees. Statistical significance was set at p < 0.05.
Results
Characteristics of population
4,562 participants were eventually included in this analysis (4,064 with non-CVD and 498 with CVD), and their characteristics were summarized by CVD status (Supplementary Table SI) and Q1~Q4 of METS-VF (Supplementary Table SII). CVD patients tended to be older, had less sleep, and higher levels of triglycerides, METS-IR, and METS-VF. Higher METS-VF levels were associated with increased risk of heart disease, stroke, and CVD, as well as higher levels of fasting glucose, triglycerides, LDL-c, and METS-IR, and lower HDL-C.
Association of METS-VF and risk of CVD
The relationship between baseline METS-VF and CVD risk was assessed by univariate and multivariate logistic regression (Supplementary Table SIII). For CVD, ORs in Model 3 were 1.48 (95% CI: 1.11–2.00), 1.59 (95% CI: 1.29–2.14), and 1.91 (95% CI: 1.44–2.55) for Q2, Q3, and Q4, respectively, compared to Q1, similar to Model 2. Each 1 IQR increase in METS-VF was associated with higher CVD risk (OR = 1.35; 95% CI: 1.17–1.55). Similar patterns were observed for stroke and heart disease, with significant risk increases in Q3 and Q4 compared to Q1. Figure 1 B shows the restrictive cubic spline (RCS) results for the dose-response association between METS-VF and incident CVD, stroke, and heart disease in a fully adjusted model. The findings indicate linear dose-response correlations (poverall < 0.05, pnon-linear > 0.05). The association between METS-VF and CVD, stroke, and heart disease can be represented as a, b, and c, respectively.
Figure 1
A – Forest plot of stratified analysis of the association of METS-VF and risk of incident CVD. B – Adjusted cubic spline models of the association between METS-VF and risk of incident CVD/stroke/heart disease. C – Decision analysis of METS-VF along with demographic and clinicopathologic characteristics

Stratified analysis
Stratified analysis (Figure 1 A) revealed that marital status (pinteraction = 0.013) and education (pinteraction = 0.048) modify the METS-VF-CVD relationship. For married individuals, each additional IQR of METS-VF was linked to a 43.4% (95% CI: 23.7–66.4) higher CVD risk, but no association was found for those living alone. For those with a college degree or higher, each IQR increase in METS-VF was associated with a 70.6% (95% CI: 6.4–173.7) higher CVD risk, but not for those with lower education levels.
Decision tree analysis
Figure 1 C shows the decision tree for incident CVD, influenced by METS-VF, age, and smoking status, with METS-VF as the root node. Three high-risk subgroups were identified: 1) METS-VF ≥ 6.2, age ≥ 57, and current smoking; 2) METS-VF ≥ 7.3 and age ≥ 57; 3) 6.2 ≤ METS-VF ≤ 7.3, non-current smoking, and age ≥ 66.
Discussion
Many studies have shown that the risk of cardiac metabolism is enhanced when visceral fat accumulates instead of subcutaneous fat [7]. The METS-VF index is a new prediction index of visceral fat content, covering multiple parameters such as age, sex, blood lipids, blood glucose, WHtR, etc. It may have more advantages in predicting insulin resistance and obesity metabolism than other indicators. Amato et al. found that elevated VAI levels increase the incidence of cardiovascular events [8]. Another study from CHARLS database [9] suggested a positive connection between VAI and stroke incidents. Our findings further confirmed that high visceral fat content may be one of the key danger signs for cardiovascular and cerebrovascular events.
Obesity is one of the leading causes of cardiovascular disease and stroke. On the one hand, obesity may induce changes in the structure and function of the cardiovascular system to adjust to being overweight [10]. On the other hand, excessive adipose tissue is closely related to inflammation, hypoxia, mitochondrial dysfunction, abnormal glucose, lipid metabolism, and endothelial dysfunction [11].
According to the results of the stratified analysis, married people and those with higher educational levels are more likely to be at risk from the high visceral fat content. Possible reasons include that married individuals, both women and men, tend to increased eating and less time for physical activity because of family commitments. Additionally, highly educated people may overeat and have less time for exercise due to heavy work pressures and better financial resources [12].
The decision tree results showed that the individuals with METS-VF ≥ 6.2, age ≥ 57 and currently smoking; individuals with METS-VF ≥ 7.3 and age ≥ 57; individuals with 6.2 ≤ METS-VF < 7.3, non-smoking, age ≥ 66 are high-risk subgroups of CVD. This indicates that compared with the harm caused by smoking, visceral fat content, and age may be two more important factors determining whether CVD occurs. This study found that TG mediates the relationship between METS-VF and CVD/stroke. Elevated METS-VF is associated with abnormal TG levels, which increases the risk of CVD/stroke.
Our study has notable advantages: it is the first study to link METS-VF with CVD, stroke, and heart disease, providing strong evidence of this association. Based on a nationwide, large sample of over 7 years, it clarifies the causal relationship and offers insights into reducing these incidents. The intermediary effect analysis also shows higher METS-VF increases TG levels, raising cardiovascular risk. However, limitations include reliance on self-reported CVD diagnoses, unadjusted eating habits and activities, and a focus on those over 45. Future research should involve a broader, younger cohort for more generalizable findings.
In conclusion, a high METS-VF index is a key risk factor for CVD, stroke, and heart disease, with TG as an intermediary. Our findings highlight the need for comprehensive care plans focusing on diet, exercise, and weight management to prevent these diseases. Reducing visceral fat and TG levels is crucial for prevention.