Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
NEPHROLOGY / RESEARCH PAPER
Mesenchymal Stem Cells Suppress Kidney Injury molecule-1 Associated with Inhibition of Renal PKC/ NF-Kβ / STAT3 Fibrotic Signaling Pathway in Rats with Diabetic Nephropathy
1
Department of Basic Medical Sciences, College of Medicine , Princess Nourah bint Abdulrahman University, P.O. Box 84428,Riyadh 11671, Saudi Arabia., Saudi Arabia
2
Department of Child Health,
College of Medicine, King Khalid University, Abha, Saudi Arabia, Saudi Arabia
3
Department of Internal Medicine
College of Medicine, King Khalid University, Abha 61421, Saudi Arabia, Saudi Arabia
4
Department of clinical biochemistry, College of medicine, king Khalid university, Abha, Saudi Arabia, Saudi Arabia
5
Department of Physiology, Kasr Al-Aini Faculty of Medicine, Cairo University, Cairo, Egypt., Egypt
6
Department of Medical Histology, Kasr Al-Aini Faculty of Medicine, Cairo University, Cairo, Egypt., Egypt
Submission date: 2024-03-22
Final revision date: 2024-07-04
Acceptance date: 2024-07-07
Online publication date: 2024-07-28
Corresponding author
Amal Dawood
Department of Basic Medical Sciences, College of Medicine , Princess Nourah bint Abdulrahman University, P.O. Box 84428,Riyadh 11671, Saudi Arabia., Saudi Arabia
Department of Basic Medical Sciences, College of Medicine , Princess Nourah bint Abdulrahman University, P.O. Box 84428,Riyadh 11671, Saudi Arabia., Saudi Arabia
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Background: Diabetes stands as the predominant etiology behind end-stage kidney disease, commonly referred to as renal failure. The intricate interplay among oxidative stress, inflammation, and renal fibrotic changes in diabetes-induced nephropathy, particularly in instances involving and not involving the administration of mesenchymal stem cells (MSCs), remains a subject less explored in existing research.
Material and methods:
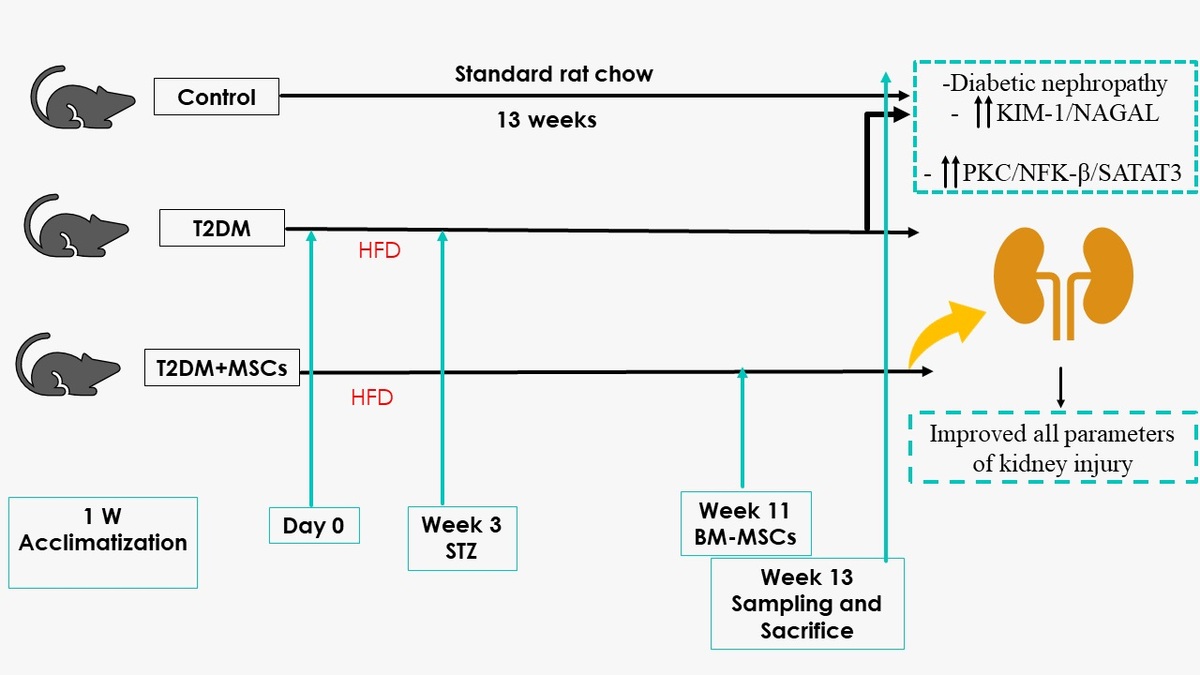
Methods: Twenty-four male Wistar rats (180 and 200 grams) were randomly assigned to one of three groups (n = 8). The control group received standard laboratory chow, and the groups with T2DM received a single dose of streptozotocin, 45 mg/kg, after three weeks of pretreatment with a high-fat diet (HFD). Rats with T2DM were split into the T2DM model group and Bone marrow (BM) mesenchymal stem cells (MSCs) treated group (T2DM+MSCs) eight weeks after DM was confirmed. BM-MSCs were injected systemically at 2 × 106 cells/rat doses.
Results:
Results: Diabetes significantly altered oxidative stress (MDA, SOD), inflammation (TNFα, IL-6), and kidney injury (KIM-1, NAGAL) biomarkers, a modulation that was mitigated by MSCs (p < 0.0001). Furthermore, diabetes-induced kidney fibrosis showed a noteworthy reduction in the presence of MSCs. A notable correlation emerged between body weight, systolic blood pressure (SBP), oxidative stress, inflammation, fibrosis, the PKC/NF-KB/STAT-3 axis, and hyperglycemia.
Conclusions:
Conclusions: Our results suggest that diabetes was associated with elevated oxidative stress, inflammation, biomarkers of kidney injury, upregulation of the renal PKC/NF-KB/STAT-3 pathway, and hypertension, all countered by MSCs intervention.
Background: Diabetes stands as the predominant etiology behind end-stage kidney disease, commonly referred to as renal failure. The intricate interplay among oxidative stress, inflammation, and renal fibrotic changes in diabetes-induced nephropathy, particularly in instances involving and not involving the administration of mesenchymal stem cells (MSCs), remains a subject less explored in existing research.
Material and methods:
Methods: Twenty-four male Wistar rats (180 and 200 grams) were randomly assigned to one of three groups (n = 8). The control group received standard laboratory chow, and the groups with T2DM received a single dose of streptozotocin, 45 mg/kg, after three weeks of pretreatment with a high-fat diet (HFD). Rats with T2DM were split into the T2DM model group and Bone marrow (BM) mesenchymal stem cells (MSCs) treated group (T2DM+MSCs) eight weeks after DM was confirmed. BM-MSCs were injected systemically at 2 × 106 cells/rat doses.
Results:
Results: Diabetes significantly altered oxidative stress (MDA, SOD), inflammation (TNFα, IL-6), and kidney injury (KIM-1, NAGAL) biomarkers, a modulation that was mitigated by MSCs (p < 0.0001). Furthermore, diabetes-induced kidney fibrosis showed a noteworthy reduction in the presence of MSCs. A notable correlation emerged between body weight, systolic blood pressure (SBP), oxidative stress, inflammation, fibrosis, the PKC/NF-KB/STAT-3 axis, and hyperglycemia.
Conclusions:
Conclusions: Our results suggest that diabetes was associated with elevated oxidative stress, inflammation, biomarkers of kidney injury, upregulation of the renal PKC/NF-KB/STAT-3 pathway, and hypertension, all countered by MSCs intervention.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.