Medical errors can cost lives and, in several situations, most likely are best viewed as a mistake of judgment. Up to 75% of medical errors are thought to be the consequence of cognitive errors [1]. The human brain employs shortcuts to make the quick decisions we need to get by. We are constantly forced to make decisions due to insufficient information. Any alternative course of action would cause paralysis. Two ways for people to make decisions are commonly known [2, 3]. The first, referred to as System 1, enables quick, spontaneous, and unconscious decision-making. Although it does not take much time or effort, it is prone to bias and systematic inaccuracy. It is practical and enables us to decide quickly, even with limited information. Driving a car or a bicycle are two good examples of actions that need no conscious thought or effort. System 1 is quick and straightforward. System 2 makes decisions slowly, deliberately, and under control. Without concentrated attention, it cannot function. It can be tiresome and requires work. Math tests and public speaking are two classic examples, and Daniel Kahneman’s contribution to decision-making has been recognized in medicine [4, 5].
Daniel Kahneman, an Israeli American author, psychologist, and economist, was born on March 5, 1934, and passed away on March 27, 2024. He is most known for his research on the psychology of judgment and decision-making. Along with Vernon L. Smith, he was given the 2002 Nobel Memorial Prize in Economic Sciences for his work in behavioral economics, which has gained him notoriety. In collaboration with Amos Tversky and others, Kahneman created prospect theory and provided a cognitive foundation for typical human errors that result from heuristics and biases. From 1970 until 1978, Kahneman was an instructor at Jerusalem’s Hebrew University. Later, he was employed as a lecturer at the University of British Columbia until 1986. He then spent 8 more years as an instructor at the University of California, Berkeley. After that, Kahneman served as an emeritus faculty member and senior scholar at Princeton University’s Princeton School of Public and International Affairs and Psychology Department. In addition, he was a Gallup Senior Scientist, and The Economist named him the eighth most influential economist in the world in 2015 [6].
Daniel Kahneman was among the first to observe that human cognitive capacity is finite and prone to error when overworked [5]. Documentation requirements can be overly stringent, demanding physical exam points, system reviews, and the assessment and recording of irrelevant past events. Though other forms of the error have subsequently been described, Daniel Kahneman and Amos Tversky recognized three frequent sources of error or heuristics. The first was referred to as availability, which is a cognitive shortcut that depends on current instances while assessing a choice. A physician encounters many young, anxious people in the Emergency Room yet hardly ever notices life-threatening illnesses. Commonly, more than 85% of patients arrive at the Emergency Room on their own, without the need for an ambulance or other emergency support, and less than 5% are discovered to be gravely sick [7].
Representativeness is a second heuristic or the mistake in estimating probability under uncertainty. This entails incorrectly calculating likelihood and classifying a decision with others that share similar features. French physicians Charles Lasegue and Jean-Pierre Falret first used the word “folie au deux”, which roughly translates to “double delusion”, in the 19th century to describe the spread of one person’s beliefs to another. It has come to characterize a mental illness where a person passes on a delusion or hallucination to another person.
The third heuristic is labeled anchoring. This happens when people base too much of their decision-making process on preliminary information. Several variables that lower the physician’s mental ability, including a constrained amount of time, multitasking, wearing out, and an increasing amount of documentation and unnecessary questions to make a diagnosis, have been introduced by well-meaning bureaucrats.
Dimidium facti, qui coepit, habet; sapere aude, incipe (“He who has begun is half done; dare to know, dare to begin”, Horace) [8]. Thus, if we dare to start with the right system and tools, we may be ahead in clinical reasoning. The patient’s evaluation needs to happen in a serene, quiet setting with the physician solely concentrating on them. Physicians are chosen for their resilience and receive their training in turbulent conditions. One of the most highly valued qualities that sets the best apart is the ability to function without food, sleep, or respite. Setting limits or saying no is a sign of weakness. It does not take long for a physician (medical doctor) to realize that. Rest and sleep are indulgences. In addition to entering data and making sensible decisions, today’s doctors are expected to make patients happy, exhibiting multi-task behavior, make accurate diagnoses, and suggest the best course of treatment. Despite the limitations of human intellect, healthcare systems demand that doctors perform numerous unrelated activities simultaneously with speed and efficiency. While processing information for multiple patients with various diseases, we also have to answer calls, pagers, texts, and emails, and occasionally suddenly may even knock on our office or exam room door. In this process, doctors manually enter data into computers while attempting to maintain empathy, not necessarily to avoid a decline in patient satisfaction ratings. The fact that mistakes are made is not surprising, but the fact that these are unusual is evidence of healthcare professionals’ commitment and hard work. More years of instruction, ongoing medical education, or state medical board oversight cannot resolve the issue. Medicine itself needs to be more personalized if cognitive error is to be eradicated. The rediscovery of the clinical autopsy may be critical to refresh the attention of physicians to the consequences of actions carried out in an emergency setting, and the autopsy should still be considered a crucial quality assurance parameter in a hospital.
Recently, medical errors have gained recognition as a significant public health issue, being identified as the third most common cause of mortality in the United States [9]. Nevertheless, due to several categories of failures (such as diagnostic or medication errors) that can lead to varied consequences (such as near-miss, injury, or no harm), the estimates of the occurrence of medical errors fluctuate significantly among research. An analysis revealed that almost 400,000 patients who are admitted to hospitals suffer avoidable injuries each year. At the same time, another study approximated that over 200,000 patient fatalities each year are caused by avoidable medical mistakes [10–12]. Furthermore, the documented financial impact of medical mistakes is extensive, with certain experts conservatively estimating $20 billion yearly and others calculating healthcare expenses ranging from $35.7 to $45 billion solely for hospital-acquired infections [10]. Due to the varying definitions of medical errors, it is challenging to analyze them using consistent criteria. Moreover, the absence of defined nomenclature has impeded assessing, synthesizing, and evaluating data. The Institute of Medicine (IOM) Committee on Quality of Health Care in the US, which conducted the initial comprehensive study on medical errors, provided a precise definition of a medical error as “the inability to successfully execute a planned action as intended or the utilization of an incorrect strategy to accomplish a goal”. An alternative interpretation characterizes medical errors as a breakdown in the provision of care that may or may not lead to injury to the patient. Regardless of its definition, the medical error is linked to significant morbidity, mortality, and economic cost. Furthermore, errors might adversely affect the patient, their family, participating clinical professionals and support personnel, the healthcare institution, and the community [13]. Healthcare practitioners may undergo significant psychological consequences (such as rage, guilt, inadequacy, sadness, and suicidal thoughts) as a result of real or perceived mistakes, which the possibility of imminent legal litigation may exacerbate. In addition to their duty to not harm, clinicians may connect errors with failure, a breach of public trust, and patient injury, resulting in diminished clinical confidence [14]. Some experts argue that “error” is unduly confrontational and sustains a blame culture. Given its negative connotation, it is advisable to use the term sparingly while recording patient records; some experts recommend that the term be completely avoided. Nevertheless, incidental side effects resulting from medical mistakes happen; ceasing the term will not probably prevent or decrease these errors [15]. Identifying the root cause of these errors and offering effective remedies to prevent their occurrence is a formidable challenge. Knowing the many categories of medical errors is essential for healthcare practitioners to gain a deeper understanding of the potential negative consequences that may arise. Key medical errors include surgical errors, diagnostic errors, drug problems, equipment malfunctions, patient falls, hospital-acquired infections, and breakdowns in communication. By identifying defects, failures, and risk factors that contribute to an undesirable event, it becomes possible to devise corrective actions to prevent repeated errors. Facilitating the participation of persons engaged in all facets of healthcare in reporting medical errors is crucial for this procedure. Use of confidential reporting options is essential for the identification of any shortcomings or problems that may exist inside a system. Implementing changes in workplace culture and establishing procedures for dealing with medical errors might promote the reporting of such errors. By embracing a patient safety culture and implementing corrective measures, institutions can enhance the safety of healthcare for both patients and healthcare personnel. Collaboration among healthcare experts can enhance patient safety by recognizing the underlying causes and occurrences that lead to medical mistakes, formulating comprehensive prevention protocols, and executing these measures at different levels of healthcare. Patient safety has traditionally been characterized by its dependence on outcomes, primarily emphasizing avoiding negative patient consequences. Nevertheless, numerous research have acknowledged the need of comprehending the organizational shortcomings that frequently result in medical mistakes in order to formulate efficient prevention measures. Healthcare practitioners must possess a thorough understanding of the commonly used terminology in order to precisely identify the specific kind of medical errors, evaluate their frequency, and ascertain possible triggering factors [15, 16]. An active error refers to a particular incident that results in injury to a patient and engages healthcare practitioners in the provision of patient care, such as performing ocular surgery on the incorrect eye. A latent error refers to inherent deficiencies in the patient care process, such as defective equipment, inefficient organizational structure, or inadequate system design. Several doctors are favored and receive equipment, offices or systems, which may be considered adequate. These aspects may also be evaluated in subsequent comprehensive surveys of wards and laboratories and can be avoided using cyclical evaluation of the structure and wellbeing of the physicians. These flaws may remain undetected for an extended period without causing any significant consequences. Latent errors might be described as “accidents waiting to happen”. A defective ventilator equipment or an inadequately maintained microscope can exemplify a pretty classic latent error. Nevertheless, the clinician’s omission to inspect the gadget before use remains probably according to different court proceedings an active mistake [9].
An IOM medical error is the failure to execute the planned course of action or execute an incorrect plan to reach the desired result. Other experts defined medical errors as departures from the established care protocol that may or may not lead to harm to the patient. Furthermore, medical mistakes can be classified as omission or commission errors. Errors of omission result in adverse outcomes when specific actions are not performed (e.g., failing to secure a patient in a wheelchair or not stabilizing a gurney before transferring a patient). In contrast, errors of commission arise as a consequence of a direct action by a healthcare team member (e.g., giving a medicine to a patient with a documented allergy or incorrectly labeling a laboratory sample with the unintended patient name) [9]. Some experts define adverse events as instances of omission or commission in the planning or execution of medical management that result in or have the potential to harm patients, as outlined in pediatric transplantation services [17]. The subcategories of medical errors encompass communication errors, diagnostic errors, surgical errors, and clinical suicide [10]. As defined by the IOM, an adverse event is a patient injury that leads to impairment or extended hospital stay due to medical or surgical treatment rather than the patient’s underlying illness. Furthermore, adverse events may encompass issues arising from extended hospital stays or fundamental characteristics of the healthcare system.
Nevertheless, not all negative consequences arise from a medical mistake. In contrast, a preventable adverse event is a patient injury resulting from a medical error [16, 18]. To further classify preventable adverse events, several groupings have been identified [9]. Legal negligence refers to the failure of a competent healthcare professional to provide the anticipated level of care for a patient in identical circumstances, such as failing to verify a pathology report leading to a missed cancer diagnosis. A classic example is when the consultant pathologist does sign out the histopathology report without perusing carefully and thoroughly the gross and microscopic findings, which may have been dictated by a trainee, resident or fellow. Furthermore, a negligent adverse event denotes inadequate medical or surgical care that meets the legal requirements for carelessness, resulting in injury to the patient.
A near-miss event refers to a medical mistake that could potentially cause harm to a patient but was prevented either by active intervention or random chance. Near misses are synonymous with adverse occurrences, except that they do not result in any injury to the patient. Hence, near misses present ideal circumstances for formulating preventative measures and should be subjected to the same level of examination as harmful incidents, and laboratory information systems, such as EPIC, are critical [13, 16, 19, 20].
A potentially compensable occurrence is an adverse event, such as disability and extended hospitalization, that has the potential to result in malpractice claims [18].
Never events refer to medical errors that are considered to be completely avoidable, such as the occurrence of pressure ulcers or unintended surgical procedures [18].
A noxious episode refers to diagnostic or treatment procedures that result in negative occurrences or complications. For example, opting to send a trauma patient with unstable hemodynamics for extended imaging examinations instead of the operating room, leads to traumatic arrest and subsequent death [18].
A root cause is a missing or omitted factor that, if rectified or prevented, would completely remove the negative outcome (Figure 1). A multitude of variables frequently contribute to an avoidable consequence of patient injury. The most prevalent root causes include human error (such as insufficient education, incomplete assessments, and misdiagnosis), communication problems (such as failure to disclose problems, inadequate patient counseling, and failure to obtain informed consent), and organizational process deficiencies (such as insufficient patient identification methods, equipment failures, lack of organizational protocols, or inadequate staffing and supervision, as well as misleading or retracted job plans) [21, 22]. Failure to address these aspects by the chief of staff may have serious consequences for the organization.
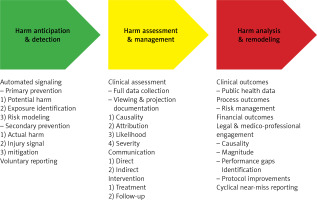
Figure 1
This photograph illustrates the process of harm anticipation, assessment, and remediation using three main categories. The first category includes automated signaling to catch medical errors. The prevention may be subclassified as primary with potential harm, the identification of exposure to harm, and a theoretical risk modeling. Secondary prevention entails the actual harm, the identification of injury, and its mitigation. A voluntary reporting harm is often included in this category. The category of harm assessment and management entails a thorough assessment with collection of data, viewing, interpretation, and projection. Documentation remains key in all these processes, but the second category is critical, because we aim to identify the causality, attribution, likelihood, and the degree of severity. Communication is key in healthcare and can be direct or indirect to the patient. This category also includes a potential treatment of the injury linked to the medical error and its follow-up. Finally, the third category gathers data for public health officials, data for the evaluation of the process and risk management, financial burden due to the medical error, legal and medico-professional consequences, which include a new assessment of the causality and magnitude of the medical error as well as the identification of performance gaps, and the improvement of healthcare protocols. The final step is a cyclical reporting of near-miss incidents, which ultimately has the goal to educate healthcare professionals to mitigate the errors in medicine
Moreover, the Joint Commission defines a sentinel event as any unforeseen negative occurrence specifically related to death, severe physical or psychological harm, or the potential for such damage. In the context of process variations, the term ‘or the danger thereof’ encompasses any variation that, if repeated, would have a substantial probability of causing a severe negative consequence. Sentinel occurrences clearly indicate the necessity for an urgent inquiry to identify the underlying cause and formulate appropriate remedial actions. Furthermore, the Joint Commission evaluates all sentinel incidents that have led to unforeseen death, substantial long-term damage, or serious, temporary damage necessitating medical intervention to maintain life. All member healthcare agencies are obligated to report these incidents [23]. The sentinel events encompass:
– Abduction of a patient.
– Unexpected mortality of a full-term newborn or any maternal death occurring during childbirth.
– Discharge of a child to an incorrect family.
– A hemolytic transfusion reaction occurs when blood or blood products with marked incompatibility are administered.
– Procedures performed on an incorrect patient or at a wrong location.
– Incidents of rape, assault, or homicide against any patient undergoing medical treatment.
– Severe maternal morbidity leading to either permanent or severe, transient complications.
– Neonatal severe hyperbilirubinemia above 30 mg/dl.
– Suicide of any patient receiving care in a staffed-around-the-clock care facility within 72 h after being discharged.
– Unintentional retention of an excised foreign item in a patient during surgical procedures [9].
The predominant approaches for reviewing and assessing the causes that contributed to a sentinel event or a medical error are root cause analysis (RCA) and failure mode effect analysis. The investigations above are crucial to detecting current and latent faults and formulating effective prevention measures [24].
RCA identifies the underlying causes that significantly contribute to harmful and hazardous events [22, 24]. The Joint Commission mandates that healthcare institutions conduct a root cause investigation following sentinel events to identify the underlying causes and contributing elements that led to a sentinel event. Determining these elements aids in the prevention of recurring mistakes by formulating an action plan for improvement. The primary focus of the RCA team members is on systems and processes rather than individual activities [22]. For example, when a hospital does a RCA of a patient who is allergic to erythromycin and experiences an acute anaphylactic reaction after being prescribed azithromycin, it may be necessary to create an action plan to educate the whole medical team about drug-drug interactions and similarities. Implementing an electronic medical record “stop alert” can effectively prevent the recurrence of this blunder. This report is subsequently submitted to the Joint Commission, where it is consolidated with all other reports from the RCA. Additionally, a risk-reduction approach is published in the “Sentinel Event Alert” weekly. Healthcare organizations who do not do an RCA are subject to an “accreditation watch” by the Joint Commission. This is a public announcement that indicates a sentinel incident occurred without properly implementing an appropriate action plan. When a sentinel occurrence poses a risk to the health and safety of patients, the Joint Commission initiates on-site evaluations [22].
Failure mode effect analysis is a method that promotes safety and accident avoidance by strategically detecting possible or present failures and their consequences. Failure mode effect analysis is a method that involves ongoing quality improvement to identify and rectify places where errors have happened or are likely to occur. The main objective of failure mode effect analysis is to establish redundancy that function as several safety measures to effectively avoid errors [25].
In conclusion, there is still a lot of work ahead to reduce harms for our patients and the importance of seminal work, such as that published by Professor Daniel Kahneman will be indispensable for the future of harm-preventing strategies in healthcare.