Introduction
There is a high rate for middle cerebral artery (MCA) lesions to cause stenosis or occlusion in stroke patients. MCA occlusions (MCAO) occur far more than other artery occlusions in ischaemic cerebrovascular diseases and occupy a very important position [1]. A recent study reported a recurrent stroke risk of 12.5% during 12 months among patients with symptoms of middle cerebral artery stenosis or occlusion [2]. The prognosis of patients with large artery occlusion disease of the middle cerebral artery is relatively poor, with fatality rates up to 80% [3]. Earlier studies on intracranial artery lesions have focused on the risk factors of middle cerebral artery disease, clinical characteristics, imaging, treatment effect comparison, and the short-term prognosis. Long-term prognosis and recurrent stroke rates among patients with MCAO have not attracted much attention [4]. This paper documents a clinical trial of long-term prognosis and risk of recurrent stroke in patients with MCAO in a single centre using CT angiography (CTA) or magnetic resonance angiography (MRA), widely used in the world.
The main purpose of this article is to observe a long-term prognosis of MCAO patients and add information for potential real world studies.
Material and methods
Patient eligibility
Data were retrospectively collected among patients with middle cerebral ischaemia, including ischaemic stroke and transient ischaemic attack (TIA) diagnosis, evidenced by CTA or MRA in patients from January 2006 to December 2013. The inclusion criteria were: 1) patients hospitalised due to TIA or acute cerebrovascular diseases; 2) cerebral infarction diagnosed according to the criteria established at the Fourth Academic Conference of National Cerebral Vascular Disease in 1995 [5], confirmed by CTA or MRA on admission; 3) head CT scans excluded post-infarction haemorrhage during aggravation of the disease; and 4) patients received standard treatment such as antiplatelet, volume expansion, hypoglycaemic antihypertensive, and neuro-protective therapies. Exclusion criteria are: 1) severe renal or hepatic function deficiency, autoimmune diseases, cancer, haematological diseases, and rheumatic diseases; 2) severe trauma, surgery, or any kind of infection within 2 weeks of disease onset; 3) congenital absence of MCA; and 4) severe stroke: a score higher than 20 points according to the National Institutes of Health Stroke Scale (NIHSS).
Patients took aspirin 300 mg for 3 days and 100 mg daily afterwards. Anti-lipaemic and hypoglycaemic treatment were taken after the diagnosis of hyperlipaemia or hyperglycaemia. Informed consent was obtained from all subjects according to the guidelines of the Ethics Committee.
Definition of risk factors
Information on age, sex, hypertension (defined as a history of hypertension, being treated with an antihypertensive agent before admission, or systolic blood pressure ≥ 140 mm Hg and/or diastolic blood pressure ≥ 90 mm Hg), diabetes mellitus (defined as a history of diabetes mellitus, or being treated for diabetes mellitus or glycosylated haemoglobin ≥ 7% or random venous blood glucose ≥ 11.1 mmol/l and/or fasting blood-glucose ≥ 7.0 mmol/l and/or 2 h after glucose load ≥ 11.1) and hyperlipidaemia (defined as low-density lipoprotein cholesterol 2.6 mmol/l at admission or a history of hyperlipidaemia or receiving lipid-lowering treatment), a history of cerebral ischaemia (including a history of ischaemic stroke and TIA), a history of atrial fibrillation, and a history of coronary heart disease (including a history of myocardial infarction and angina pectoris) were collected. In addition, current smoking (defined as a patient who had smoked continuously ≥ 1 cigarette per day for 6 months), history of alcohol drinking (drinking > 2 units per day on average for men or > 1 unit per day on average for women), and homocysteine (serum level of total homocysteine ≥ 15 μmol/l) status were noted.
Other intracranial arterial occlusions included the intracranial internal carotid artery, anterior cerebral artery, middle cerebral artery, posterior cerebral artery, and basilar artery. Extracranial arterial occlusions included the extracranial internal carotid artery and vertebral artery confirmed by CTA or MRA. The medication compliance (aspirin, clopidogrel, and statins) was followed up by phone or medical records after discharge.
Follow-up and assessment of end points
Trained researchers at Beijing Friendship Hospital use standard scripts to collect data at discharge, 6, and 12 months and once a year until 8 years after stroke onset. The enrolled patients filled out questionnaires for the follow-up study. When it was impossible to reach the patients directly or the information provided by the patients was unreliable, the information was obtained from caregivers. Fatality was confirmed either by a death certificate from the citizen registry or the hospital records. End points and safety events included: stroke, TIA, or death.
Disability was measured by the modified Rankin Scale (mRS) score, ranging from 0 to 5, with death rated as 6. Stroke recurrence was defined as sudden functional deterioration in neurological status with a NIHSS score of 4 or higher, or a new focal neurological deficit of vascular origin lasting > 24 h.
Blood sampling
Blood samples were collected in polystyrene tubes between 08:30 and 10:00 a.m. by venepuncture of the antecubital vein on the third day after admission. Serum glucose (GLU), triglyceride (TG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), cholesterol (CHOL), uric acid (UA), aspartate transaminase (AST), alanine transaminase (ALT), blood urea nitrogen (BUN), albumin (ALB), or creatinine (Cr) concentrations were measured by enzymatic colourimetric methods with commercially available kits on an AU5821 or 7600 Series Automatic Analyzer (Hitachi, Japan). High-sensitivity C-reactive protein (hs-CRP) in the serum was analysed by an immune turbidimetric assay on a MODULAR-P800 analyser (Roche Diagnostics, Germany) with the manufacturer’s reagents. Fibrinogen (Fbg) and prothrombin temporal activity (PTA) concentrations were measured by freezing method while D-dimer by latex immunoturbidimetry with commercially available kits on the CS5100 automatic coagulation analyser. Homocysteine (HCY) in the serum was analysed by a circulating enzymatic with the commercially available kits on an AU5821. White blood cells (WBC) were measured by flow cytology, haemoglobin (Hb) by colorimetric determination, haematocrit (HCT) was obtained by calculation, and blood platelet (PLT) by impedance method with the commercially available kits on an XN-3000 Sysmex. Erythrocyte sedimentation rate (ESR) concentrations were measured by natural settling on VACUETTE SRS100/II, as directed, in the laboratory at Beijing Friendship Hospital of Capital Medical University.
Statistical analysis
Statistical analysis was performed using SPSS 13.0 (SPSS Inc., Chicago, IL, USA). Continuous variables were reported in terms of their means, standard deviations, and Student’s t-test statistics. Numerical data not following normal distributions are characterized by their median (interquartile range (IQR)) values and the Wilcoxon test statistics. Categorical variables were reported as proportions and the χ2 test statistics. Univariate and multivariate logistic regression analysis were used to evaluate the relationships between risk factors and the prognosis of MCAO. A favorable clinical outcome was defined as having an mRS score of 2 or lower after follow-up. Statistical significance was set as p < 0.05. This study was approved by the Ethics Committee of Beijing Friendship Hospital, Capital Medical University, Beijing, China.
Results
A total of 119 participating patients from January 2006 to December 2013 were included for the followed-up study with an average of 46.8 months (6–97 months), and a lost rate of 14.28% (17 patients). There were 78 (76%) males and 24 (24%) females, among whom 20 (19.6%) patients died, and 14 (13.7%) patients suffered from recurrent stroke. According to my original data, 3 patients were followed up within 6 months, 8 patients for 1 year, 14 patients for 2 years, 15 patients for 3 years, 10 patients for 4 years, 28 patients for 5 years, 26 patients for 6 years, 9 patients for 7 years, and 6 patients for 8 years or more. Six patients died within the half year, 3 patients died at 1 year, 2 patients died at 2 years, 5 patients died at 3 years, 1 patient died at 4 years, and 2 patients died at 5 years. There was 1 patient with recurrent stroke within the half year, 2 patients at 1 year, 4 patients at 2 years, 1 patient at 3 years, 4 patients at 4 years, 1 patient at 5 years, and 1 patient at 6 years. We did not distinguish between re-current stroke and recurrent TIA.
Modified Rankin Scale as an outcome index of influencing factors
The MCAO patients were divided into two groups according to mRS scoring: favorable group (mRS ≤ 2) and unfavorable group (mRS > 2). Demographic characteristics, and risk and biochemical factors are presented in Table I. Patients of the unfavorable group were older and with more severe stroke, higher hs-CRP, FBg, D-Dimer, and AST and lower TG level compared to those of the favorable group (median NIHSS score 3 vs. 9, p < 0.01). There were no significant differences in hypertension, hyperlipidaemia, diabetes mellitus, and historical stroke or current smokers between the two groups. Logistic multivariate regression analysis of risk factors indicated that age and NIHSS score were independent predictors of prognosis (statistical results) (Table II).
Table I
Comparisons of favourable and unfavourable outcome associated with MCAO
| Parameter | Unfavourable outcome (mRS > 2) n = 48 | Favourable outcome (mRS ≤ 2) n = 54 | P-value |
|---|---|---|---|
| Gender (%) | 79.17 | 74.07 | 0.545 |
| Age [years] | 67.6 ±10.96 | 58.56 ±13.37 | 0.000† |
| Current smoking (%) | 64.58 | 57.41 | 0.459 |
| Alcohol (%) | 50.00 | 37.04 | 0.187 |
| Hypertension (%) | 72.92 | 74.07 | 0.895 |
| Diabetes mellitus (%) | 37.5 | 35.19 | 0.808 |
| Atrial fibrillation (%) | 4.17 | 0.00 | 0.219 |
| History of coronary artery disease (%) | 27.10 | 18.52 | 0.302 |
| History of stroke (%) | 20.83 | 29.63 | 0.309 |
| Antiplatelet (%) | 77.08 | 64.81 | 0.175 |
| Statin (%) | 62.50 | 61.11 | 0.885 |
| Antiplatelet and statin (%) | 58.33 | 51.85 | 0.511 |
| With other intracranial artery occlusion (%) | 16.67 | 18.52 | 0.807 |
| NIHSS score at admission | 9 (4–13) | 3 (1–12) | 0.002† |
| ESR [mm/h] | 28.23 ±25.63 | 19.15 ±14.87 | 0.111 |
| hs-CRP [mg/dl] | 4.56 (2.15–11.13) | 2.12 (1.00–4.15) | 0.002† |
| WBC [×109/l] | 7.375 (5.79–8.53) | 6.77 (5.85–8.70) | 0.447 |
| Hb [mg/l] | 137.13 ±18.62 | 139.40 ±14.80 | 0.414 |
| HCT (%) | 40.53 ±5.19 | 40.95 ±4.44 | 0.669 |
| PLT [×109/l] | 228.30 ±74.46 | 225.45 ±56.56 | 0.829 |
| HCY [μmol/l] | 19.60 (13.70–26.90) | 16.70 (13.75–22.00) | 0.217 |
| CHOL [mmol/l] | 4.51 ±1.37 | 4.75 ±1.33 | 0.384 |
| TG [mmol/l] | 1.36 ±0.58 | 1.89 ±1.25 | 0.008† |
| HDL-C [mmol/l] | 0.99 (0.81–1.24) | 0.93 (0.71–1.07) | 0.366 |
| LDL-C [mmol/l] | 2.65 ±0.86 | 2.80 ±0.73 | 0.361 |
| GLU [mmol/l] | 5.53 (4.89–6.48) | 5.62 (4.56–7.57) | 0.733 |
| ALT [U/l] | 22.70 ±17.04 | 18.85 ±10.84 | 0.173 |
| AST [U/l] | 21.00 (17.00–31.00) | 16.50 (14.00–20.25) | 0.000† |
| ALB [g/l] | 37.45 ±3.92 | 38.32 ±3.66 | 0.279 |
| UA [μmol/l] | 256.51 ±80.46 | 272.57 ±112.71 | 0.420 |
| Cr [μmol/l] | 79.00 (67.00–89.00) | 83.00 (73.00–90.50) | 0.423 |
| BUN [mmol/l] | 4.97 (3.77–5.88) | 4.40 (3.65–5.31) | 0.053 |
| Fbg [g/l] | 4.68 (3.35–15.00) | 3.32 (2.38–4.68) | 0.001† |
| D-dimer [mg/l] | 0.50 (0.17–1.50) | 0.38 (0.10–0.68) | 0.039* |
| PTA (%) | 70.67 ±25.87 | 73.10 ±31.47 | 0.090 |
MCAO – middle cerebral artery occlusions, mRS – modified Rankin scale, NIHSS – the National Institutes of Health Stroke Scale, ESR – erythrocyte sedimentation rate, hs-CRP – C-reactive protein, WBC – white blood cells, Hb – haemoglobin, HCT – haematocrit, PLT – blood platelet, HCY – homocysteine, CHOL – cholesterol, TG – triglyceride, HDL-C – high-density lipoprotein cholesterol, LDL-C – low-density lipoprotein cholesterol, GLU – serum glucose, ALT – alanine transaminase, AST – aspartate transaminase, ALB – albumin, UA – uric acid, Cr – creatinine, BUN – blood urea nitrogen, Fbg – fibrinogen, PTA – prothrombin temporal activity.
Factors influencing stroke recurrence
MCAO patients were divided into two groups based on stroke recurrence. Demographic characteristics, and risk and biochemical factors are presented in Table III. Patients with stroke recurrence often had other intracranial or extracranial artery occlusions. Their levels of D-Dimer, CHOL, LDL-C, and UA were lower. There were no significant differences in hypertension, diabetes mellitus and historical stroke or current smoking between the two groups. Logistic multivariate regression analysis indicates that other coexisting intracranial or extracranial artery occlusions were independent predictors of recurrent stroke (Table IV).
Table III
Comparisons between patients with or without recurrent stroke
| Parameter | With stroke recurrence (n = 14) | Without stroke recurrence (n = 88) | P-value |
|---|---|---|---|
| Gender (%) | 64.29 | 78.41 | 0.247 |
| Age [years] | 67.6 ±10.96 | 58.56 ±13.37 | 0.000† |
| Current smoking (%) | 71.43 | 59.09 | 0.560 |
| Alcohol (%) | 35.71 | 44.32 | 0.546 |
| Hypertension (%) | 71.43 | 73.86 | 1.000 |
| Diabetes mellitus (%) | 42.86 | 35.23 | 0.581 |
| Atrial fibrillation (%) | 0.00 | 2.27 | 1.000 |
| History of coronary artery disease (%) | 21.43 | 21.59 | 1.000 |
| History of stroke (%) | 7.14 | 28.41 | 0.113 |
| Antiplatelet (%) | 64.29 | 69.32 | 0.834 |
| Statin (%) | 62.50 | 61.36 | 0.885 |
| Antiplatelet and statin (%) | 50.00 | 55.68 | 0.691 |
| With other intracranial artery occlusion (%) | 42.86 | 13.64 | 0.008† |
| NIHSS score at admission | 7.36 ±5.26 | 6.89 ±5.50 | 0.766 |
| ESR [mm/h] | 19.44 ±13.65 | 24.84 ±22.79 | 0.496 |
| hs-CRP [mg/dl] | 2.96 (1.56–5.66) | 3.60 (1.50–9.90) | 0.736 |
| WBC [×109/l] | 7.01 (5.71–8.36) | 6.97 (5.85–8.70) | 0.810 |
| Hb [mg/l] | 140.64 ±11.80 | 137.96 ±17.32 | 0.579 |
| HCT (%) | 41.25 ±2.91 | 40.67 ±5.03 | 0.547 |
| PLT [×109/l] | 229.00 ±64.59 | 226.41 ±65.62 | 0.891 |
| HCY [μmol/l] | 16.46 ±6.81 | 20.43 ±10.14 | 0.233 |
| CHOL [mmol/l] | 3.83 ±1.38 | 4.77 ±1.30 | 0.015* |
| TG [mmol/l] | 1.38 (1.03–1.61) | 1.39 (1.11–1.99) | 0.619 |
| HDL-C [mmol/l] | 1.14 (0.73–5.09) | 0.93 (0.80–1.14) | 0.116 |
| LDL-C [mmol/l] | 2.29 ±0.81 | 2.81 ±0.77 | 0.024* |
| GLU [mmol/l] | 4.60 ±3.31 | 6.06 ±2.33 | 0.134 |
| ALT [U/l] | 14.50 (10.00–24.00) | 17.00 (12.00–26.00) | 0.482 |
| AST [U/l] | 19.00 (14.75–24.50) | 19.00 (15.00–25.00) | 0.704 |
| ALB [g/l] | 39.02 ±2.96 | 37.66 ±3.92 | 0.219 |
| UA [μmol/l] | 211.81 ±52.74 | 273.69 ±101.90 | 0.029* |
| BUN [mmol/l] | 4.31 ±1.42 | 4.84 ±1.66 | 0.266 |
| Cr [μmol/l] | 78.07 ±17.26 | 82.80 ±25.47 | 0.639 |
| Fbg [g/l] | 4.86 (3.70–10.00) | 3.70 (2.69–5.78) | 0.160 |
| D-dimer [mg/l] | 0.13 (0.07–0.77) | 0.43 (0.15–1.00) | 0.043* |
| PTA (%) | 64.54 ±33.58 | 73.00 ±28.31 | 0.365 |
Abbreviations: see Table I.
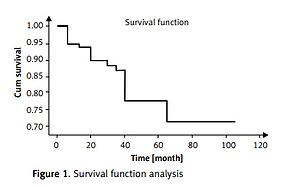
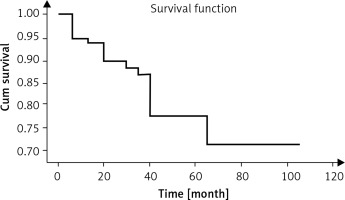
Death as an outcome index of risk factors
The analysis of survival rate using the Life Table Method gives: a 1-year survival rate of 90%, a two-year survival rate of 88%, a 3-year survival rate of 78%, and a 5-year survival rate of 71%. The median survival time was 8 years (Table V, Figure 1).
Table V
Survival rate analysis
Based on survival and death information, the MCAO patients at the end point of the study were divided accordingly with the corresponding demographic characteristics, and risk and biochemical factors shown in Table VI. Significant risk factors were identified in patients with a history of coronary heart disease, and/or HCY. High serum levels of hs-CRP, ESR, Fbg, DDimer, AST, and BUN were detected in these patients, as well as lower proportion of alcohol consumption history, TG, and ALB levels. There were no significant differences in hypertension, hyperlipidaemia, diabetes mellitus, NIHSS and historical stroke or current smoking status between the two groups. Logistic multivariate re-gression analysis revealed that the age was an inde-pendent predictor of death outcome, and a drinking history was a protective factor of death (statistical results) (Table VII).
Table VI
Comparison between the death and survival groups associated with MCAO
| Parameter | The death group (n = 20) | The survival group (n = 82) | P-value |
|---|---|---|---|
| Gender (%) | 90.00 | 73.17 | 0.195 |
| Age [years] | 74.15 ±5.36 | 59.94 ±12.89 | 0.000† |
| Antiplatelet therapy (%) | 75.00 | 69.51 | 0.834 |
| Statins (%) | 65.00 | 60.98 | 0.740 |
| Antiplatelet and statin (%) | 60.00 | 52.44 | 0.543 |
| Current smoking (%) | 80.00 | 56.10 | 0.088 |
| Alcohol (%) | 35.00 | 62.20 | 0.028* |
| Hypertension (%) | 65.00 | 75.6 | 0.335 |
| Diabetes mellitus (%) | 55.00 | 31.70 | 0.052 |
| Atrial fibrillation (%) | 0.00 | 2.44 | 0.645 |
| History of coronary artery disease (%) | 45.00 | 15.85 | 0.004† |
| History of stroke (%) | 25.00 | 25.61 | 0.955 |
| Coexisting other intracranial or extracranial artery occlusion (%) | 10.00 | 19.51 | 0.501 |
| NIHSS | 6.00 (2.25–11.75) | 5.5 (2.00–12.00) | 0.852 |
| ESR [mm/h] | 37.60 ±30.42 | 19.26 ±15.39 | 0.039* |
| h-CRP [mg/dl] | 7.00 (2.55–11.35) | 2.73 (1.18–8.91) | 0.031* |
| WBC [×109/l] | 9.14 ±6.42 | 7.48 ±2.50 | 0.271 |
| HB [mg/l] | 132.20 ±19.47 | 139.90 ±15.59 | 0.064 |
| HCT (%) | 39.81 ±1.19 | 40.99 ±0.52 | 0.326 |
| PLT [×109/l] | 244.60 ±94.26 | 222.26 ±55.38 | 0.320 |
| PTA (%) | 69.77 ±24.60 | 72.46 ±29.87 | 0.737 |
| Fbg [g/l] | 8.90 (4.49–27.75) | 3.46 (2.56–5.33) | 0.000† |
| D-dimer [mg/l] | 0.49 (0.20–2.00) | 0.38 (0.13–1.00) | 0.031* |
| HCY [μmol/l] | 25.00 (14.20–31.60) | 17.40 (13.63–23.00) | 0.037* |
| TG [mmol/l] | 1.12 (0.77–1.31) | 1.45 (1.15–2.01) | 0.001† |
| CHOL [mmol/l] | 4.25 ±1.09 | 4.73 ±1.39 | 0.160 |
| LDL-C [mmol/l] | 2.53 ±0.80 | 2.78 ±0.79 | 0.227 |
| HDL-C [mmol/l] | 1.02 (0.74–1.20) | 0.93 (0.79–1.19) | 0.776 |
| GLU [mmol/l] | 5.60 ±2.55 | 5.92 ±2.52 | 0.619 |
| ALT [U/l] | 20.50 (11.25–28.50) | 16.00 (12.00–24.50) | 0.5681 |
| AST [U/l] | 22.50 (18.25–29.75) | 18.00, (15.00–21.50) | 0.008† |
| ALB [g/l] | 35.78 ±3.70 | 38.46 ±3.64 | 0.005† |
| Cr [μmol/l] | 103.00 ±53.72 | 78.92 ±14.81 | 0.282 |
| BUN [mmol/l] | 5.44 ±2.44 | 4.60 ±1.33 | 0.038* |
| UA [μmol/l] | 257.62 ±97.83 | 266.76 ±99.45 | 0.718 |
Abbreviation: see Table I.
Table VII
Multivariate regression analysis of MCAO patients death group and survival group
| Factor | B | SE | Wald | P-value | Exp (B) | OR (95% CI) |
|---|---|---|---|---|---|---|
| Age | 0.142 | 0.045 | 9.818 | 0.002 | 1.153 | 1.055–1.260 |
| Alcohol | –2.003 | 0.763 | 6.884 | 0.009 | 0.135 | 0.030–0.602 |
| Constant | –7.943 | 2.956 | 7.222 | 0.007 | 0.000 |
[i] Abbreviation: see Table II.
Discussion
Stroke has become one of the most common causes of death in China [6, 7]. The current study investigated long-term outcomes, mortality rate, and influence factors of MCAO patients. We also attempted to identify potential biomarkers of MCAO as partial evidences of prognosis for MCAO.
Our analysis suggested that the age is an independent predictor of death outcome. The risk of death increased with age, and the clinical prognosis of the surviving patients worsened with higher NIHSSscore. In our results, factors including ESR, h-CRP, HCY, Fbg, D-dimer, AST, BUN, and history of coronary heart disease were not independent predictors. Age could increase the risk of death among patients with cerebrovascular diseases and affect the functional prognosis among the surviving patients. Zemtsovskaia et al. [8] also found that aging showed the strongest association with cardiovascular (CV) risk levels, indicative of increased arterial stiffness. The increase in NIHSS score was not positively correlated with the risk of death, but with the rate of disability. In other words, as long as the MCAO patients received prompt and effective treatment during the acute stage of cerebral infarction, the risk of death did not vary with the severity of cerebrovascular disease. Wehave shown that age and NIHSS affect prognosis, which is consistent with the findings from earlier studies [9–13]. Tian et al. [14] investigated 232 MCAO patients with the average follow-up time of 17.65 months, and stroke recurrence or death as the end point event (15.09% incidence of endpoint events, resulting in annual rate of 10.26%). It was concluded that patients with symptomatic M1-segment occlusion of the middle cerebral artery had a good long-term prognosis. The factors influencing the prognosis of patients are gender, diabetes mellitus and concomitant intracranial arterial disease. Similar to the rate of endpoint events in this study, the risk of recurrent stroke and death rate of the MCAO patients were 13.7% and 19.6% in our cohort. The analysis of the recurrence of stroke as an independent endpoint event in this study suggested that patients with other intracranial or extracranial vascular occlusion had higher risk of recurrence of stroke, consistent with the previous studies.
C-reactive protein, an indicator of inflammation and a marker of atherosclerosis [15–17], is associated with ischaemic attacks among patients with ischaemic stroke [18–23]. In a controlled case study of 600 ischaemic stroke patients and 600 matched controls, serum CRP levels were significantly higher for all ischaemic subtypes than controls, both in the acute phase and at 3-month follow-up [24]. Rost et al. found that elevated serum CRP levels could be used for predicting the risk of ischaemic stroke in elderly patients [19]. Xie et al. [25] found that ischaemic stroke patients with ICAO had significantly higher hs-CRP levels than controls, further confirming hs-CRP being a sensitive inflammation marker for the presence of ICAO in ischaemic stroke patients. In this study, we found that h-CRP in MCAO patients with functionally poor prognosis or death was significantly increased, but there was no significant difference in h-CRP between the MCAO recurrence group and non-recurrence group.
Oh et al. [26] followed 141 patients with symptomatic isolated middle cerebral artery lesions (including more than 50% stenosis and occlusion) for long-term prognosis (mean follow-up time was 27.7 months) and found that diabetes is an independent risk factor for predicting stroke recurrence and mortality. There was no difference in mortality and recurrence rate between MCAO patients and patients with middle cerebral artery stenosis. Contrary to the above studies, this study found no correlation between diabetes mellitus and prognosis among the participating patients. Because the control level of blood glucose in diabetic patients was not specified in our study, it is unclear whether blood glucose level is correlated with the prognosis. A meta-analysis showed that CHOL levels in patients with a 40-to-59-year age were associated with stroke and mortality, but the correlation is not strong (statistical results needed). For patients over 60 years old, there was no correlation [27]. In this study, the patients age of death group was 74.15 ±5.36 and that of the stroke recurrence group was 67.6 ±10.96. It is also evident that the mean age of the two groups was about 57 years, and the level of blood lipid was not correlated with the prognosis. Kang et al. [28] divided 48 MCAO patients into asymptomatic and symptomatic groups, with an averaged follow-up period of 2.8 years. Their results showed that the proportion of smokers with symptomatic MCAO was higher. Hypertension, diabetes, hyperlipidaemia, smoking history, and family history have been identified as common risk factors for cerebrovascular disease. Yet this study found that the above factors have no significant correlation with the prognosis of patients with MCAO.
The patients involved in this study were not completely isolated MCAO. Some patients had occlusion of other carotid artery or the vertebral basilar artery vessels. It was found that recurrent stroke among the patients with other vascular occlusions increased, while the mortality and mRS did not increase with it, possibly due to the fact that the posterior circulation stroke has less impact on the mRS score. On the other hand, the middle cerebral artery infarction area in the carotid artery system plays a major role in mRS. Several end-point events will include Bathel index, NIHSS score, etc. in future research. One limitation of this study is its relatively small sample size, not including asymptomatic MCAO patients, and the study was conducted as a single hospital. In addition, this study may be biased in patient selection as patients who are allergic to contrast media, are older, or seriously ill, and patients who are not suitable for CTA or MRA examination were not included. Further confirmation of our findings requires a larger sample size. Nonetheless, the findings from this study may better help guide post-stroke treatment and care, and expected to benefit stroke patients.
In conclusion, our finding show that most cases of middle cerebral artery occlusion are associated with better prognosis, especially when associated with lower age at onset and less severe NIHSS score. Recurrent strokes in patients with middle cerebral artery occlusion are linked to the presence of other intra- or extracranial atherosclerotic occlusions.