Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
NEPHROLOGY / CLINICAL RESEARCH
Is N-terminal pro-brain natriuretic peptide a reliable marker for body fluid status in children with chronic kidney disease?
1
Pediatric Nephrology Department, Faculty of Medicine, Ondokuz Mayıs University, Samsun, Turkey
2
Pediatric Cardiology Department, Faculty of Medicine, Ondokuz Mayis University, Samsun, Turkey
3
Medical Biochemistry Department, Faculty of Medicine, Ondokuz Mayis University, Samsun, Turkey
Submission date: 2017-11-08
Final revision date: 2017-11-21
Acceptance date: 2017-12-24
Online publication date: 2019-06-03
Publication date: 2020-05-26
Arch Med Sci 2020;16(4):802-810
KEYWORDS
chronic kidney diseasepediatricsbioimpedance analysisvolume statusN-terminal proBNPN-terminal pro-brain natriuretic peptide
TOPICS
ABSTRACT
Introduction:
Brain natriuretic peptides, released in response to left ventricular stress, have a strong prognostic value in dialysis patients. However, their role in detecting abnormalities of fluid status is under debate; the relationship between volume status and brain natriuretic peptides (BNPs) differs among various studies. The aim of our study was to evaluate the clinical utility of N-terminal proBNP in the assessment of fluid status and cardiovascular risk in this setting.
Material and methods:
The study included 65 children: 10 pre-dialysis, 13 hemodialysis, 12 peritoneal dialysis patients and 30 healthy controls. Volume status was determined by multifrequency bioimpedance and NT-pro-BNP, as well as echocardiography to estimate the left ventricle structure and function.
Results:
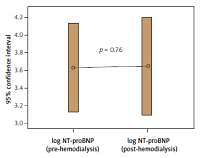
The median log NT-proBNP values of hemodialysis and peritoneal dialysis patients were 3.66 (2.05–4.90) and 3.57 (2.51–4.13) pg/ml, respectively, and significantly higher compared with the control group (p < 0.001, p < 0.001). On simple correlation, NT-proBNP was correlated with markers of volume overload and cardiac dysfunction. On multivariate regression analysis, only left ventricle mass index (β = 0.402, p = 0.003) and left atrium diameter (β = 0.263, p = 0.018) were independently associated with NT-proBNP (adjusted R2 of the model: 0.707, p < 0.001).
Conclusions:
Our research suggested that NT-proBNP, which was correlated with LV systolic and diastolic dysfunction and fluid overload as assessed by bioimpedance, can be used to evaluate cardiovascular states in a chronic kidney disease (CKD) population. From the early stages of CKD, periodic monitoring of NT-proBNP levels may be essential for early detection of patients with high risk of cardiovascular events, and for taking preventive intervention as soon as possible.
Brain natriuretic peptides, released in response to left ventricular stress, have a strong prognostic value in dialysis patients. However, their role in detecting abnormalities of fluid status is under debate; the relationship between volume status and brain natriuretic peptides (BNPs) differs among various studies. The aim of our study was to evaluate the clinical utility of N-terminal proBNP in the assessment of fluid status and cardiovascular risk in this setting.
Material and methods:
The study included 65 children: 10 pre-dialysis, 13 hemodialysis, 12 peritoneal dialysis patients and 30 healthy controls. Volume status was determined by multifrequency bioimpedance and NT-pro-BNP, as well as echocardiography to estimate the left ventricle structure and function.
Results:
The median log NT-proBNP values of hemodialysis and peritoneal dialysis patients were 3.66 (2.05–4.90) and 3.57 (2.51–4.13) pg/ml, respectively, and significantly higher compared with the control group (p < 0.001, p < 0.001). On simple correlation, NT-proBNP was correlated with markers of volume overload and cardiac dysfunction. On multivariate regression analysis, only left ventricle mass index (β = 0.402, p = 0.003) and left atrium diameter (β = 0.263, p = 0.018) were independently associated with NT-proBNP (adjusted R2 of the model: 0.707, p < 0.001).
Conclusions:
Our research suggested that NT-proBNP, which was correlated with LV systolic and diastolic dysfunction and fluid overload as assessed by bioimpedance, can be used to evaluate cardiovascular states in a chronic kidney disease (CKD) population. From the early stages of CKD, periodic monitoring of NT-proBNP levels may be essential for early detection of patients with high risk of cardiovascular events, and for taking preventive intervention as soon as possible.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.