Introduction
The ongoing coronavirus diseases 2019 (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) viral infection, is a global health crisis of a scale reminiscent of the Spanish flu pandemic almost a century ago [1]. Studies have shown that elderly patients and those with pre-existing comorbidities such as cardiovascular disease, hypertension, obesity and diabetes are at increased risk of COVID-19 associated hospitalization, critical illness and mortality [2–7]. Several studies have demonstrated that obesity is associated with an increased risk of COVID-19 associated hospitalization and/or critical illness [4, 6, 8–17]. A recent meta-analysis found a strong association between obesity and adverse outcomes in COVID-19 patients [18], indicating the role of higher body mass index (BMI) in prognostication [19, 20]. A study from a French hospital on 124 intensive care patients found an association between the need for invasive mechanical ventilation and severe obesity [16]. Another recent study on 393 cases from New York found higher rates of obesity in patients receiving mechanical ventilation [9]. It was also found that obese individuals younger than 50 are more likely to die due to COVID-19 than those who are not obese [21].
Studies have also demonstrated the association of visceral adiposity with COVID-19 severity or critical illness [22–24]. Obesity, and especially diabetes, might also be predictors of long-COVID complications, including myocarditis, arrhythmias, thromboembolism, and heart failure, as indicated in the preliminary results of the Late-COVID study [5, 25]. The impact of obesity on population demography during COVID-19 and their link to reported COVID-19 case and death rates have not been reported so far.
The current study aims to assess the association between the gender stratified average BMI, life expectancy and gross domestic product (GDP) per capita with the population-adjusted COVID-19 case rate and death rate.
Material and methods
Data sources
We used data from the Worldometer, a real-time tracking website (www.worldinfometers.info), to extract data on country-wise COVID-19 confirmed cases including population-adjusted cases and mortality rates (data accessed on 29th June 2020). Our World in Data was used to acquire data on GDP per capita, life expectancy data, average male – and female – BMI, and nationwide obesity rates. The data on Our World in Data is sourced from the official government websites or social media accounts. Based on the unanimous expert decision, only countries with a minimum of 15,000 total COVID-19 cases, as of 29th June 2020, were included in our analysis [26]. This was done to ensure that a minimum sample size within each country was reached to improve the reliability of the results and minimize any crowding due to a disproportionate number of countries with relatively lower case counts. All data procured and analyzed were sourced from publicly available databases and are available in Supplementary Table SI.
Statistical analysis
All statistical analyses were performed using STATA software (Version 11, 2001; College Station, TX, USA). The data used in this study are publicly available. The curated dataset used in this study is provided in the Supplementary Table SI. COVID-19 confirmed cases and deaths per million population (total number of COVID-19 associated deaths divided by each respective region’s population) and 95% confidence intervals (CIs) were calculated. Groupwise comparison was performed using STATA version 13 to demonstrate the distribution of baseline characteristics between countries based on the nationwide obesity rates (subgroups: < 20% vs. 20–30% vs. > 30%) and between average BMI subgroups of < 25 kg/m2 vs. > 25 kg/m2 for males and females. Subsequently, univariate and multivariate logistic regression analyses were performed to determine the association between average male and female BMI, life expectancy and GDP per capita with the population-adjusted COVID-19 case rates (for cases: ≥ 3000, ≥ 4000, ≥ 5000 per 1 million population) and death rates (for deaths: ≥ 100, ≥ 150 and ≥ 200 per 1 million population). The thresholds for various groups of caseloads per million were used based on the closest approximation of median cases/million for the 20–30% nationwide obesity rate group. This translates to 3000 cases per million. Given that the majority of countries belong to the 20–30% obese group (n = 33), the threshold was chosen to reflect the overall spread. We also selected the caseloads of 4000 and 5000 to investigate any putative linear relationship. For deaths per million population, we chose the mortality threshold based on the nearest median for the 20–30% obesity rate group – which translated to 100 deaths per million. We also chose two more points, 150 and 200, to investigate linear trends in mortality. The receiver operating characteristic curve (ROC) for the final multivariate regression model (obtained by backwards regression with variables p < 0.1) was plotted and the area under the curve computed to evaluate the predictive ability of the regression model.
Results
A correlation matrix of the investigated variables is shown in Figure 1. Male BMI shows a strong correlation with the female BMI (0.6274; p ≤ 0.0001), obesity rate (0.72; p < 0.00001), GDP per capita (0.486; p = 0.0001), and life expectancy (0.49; p = 0.0001). Though weaker, male BMI was also significantly correlated with the total number of COVID-19 associated deaths per million (R2 = 0.3261; p = 0.0125) and the total number of cases per million (0.3757; p = 0.0037). Female BMI was not correlated with deaths per million (–0.0276; p = 0.8370), whereas the correlation of female BMI with the total number of cases per million was significant (0.3191; p = 0.0146). There was a strong correlation of female BMI with nationwide obesity rate (0.8405; p ≤ 0.000001). Female BMI was not correlated with GDP per capita (0.1756; p = 0.1874) or life expectancy (–0.0492; p = 0.7136).
Group-wise comparison of various metrics stratified by countries with obesity rates of < 20%, 20–30% and > 30% are shown in Table I. The highest caseload is demonstrated in the >30% group. The highest mortality was demonstrated in the 20–30% group, while it was the least pronounced in the > 30% group. GDP per capita in the > 30% obesity rate group is more than twice as high as the GDP per capita in the 20–30% group. There is a statistically significant difference in the median population-adjusted COVID-19 cases, COVID-19 deaths, average male BMI, average female BMI, GDP per capita and prevalence of obesity between at least two of the three groups. From the data, although countries with a higher prevalence of obesity have more COVID-19 cases, the mortality is bell-shaped with the greatest mortality being in the 20-30% obesity rate group. A paired t-test revealed a statistically significant difference between average male and female BMIs in these countries overall (p = 0.0130) (Table II).
Table I
Description of ecological variables stratified by nationwide obesity rates of < 20%, 20–30% and > 30%
Table II
Description of ecological variables stratified by average body mass index
Population-adjusted case rate univariate and multivariate logistic regression
The univariate associations with population-adjusted COVID-19 cases per 1 million population were examined for average male BMI, average female BMI, life expectancy, GDP per capita, and nationwide obesity rate. COVID-19 cases per 1 million population were further stratified into ≥ 3000 per million, ≥ 4000 per million, and ≥ 5000 per million.
In population-adjusted case rate univariate logistic regression, all variables except average female BMI were significantly associated with each of the COVID-19 cases per 1 million population group (Table III). Average male BMI, GDP per capita, life expectancy, and nationwide obesity rate were included in the multivariate logistic regression model; however, no variable was a significant predictor in the multivariate model. The analyzed variables provided a poor predictive model for COVID-19 cases per 1 million population (area under the ROC curve for each stratum: 0.7867, 0.7614, and 0.7547, respectively) (Table IV).
Table III
Univariate logistic regression for association with population-adjusted case rate
Table IV
Multivariate logistic regression for association with case load per million population
| Variable | Cases ≥ 3000 per 1 million population | Cases ≥ 4000 per 1 million population | Cases ≥ 5000 per 1 million population | |||
|---|---|---|---|---|---|---|
| OR | P-value | OR | P-value | OR | P-value | |
| Average male BMI | 1.41 (0.90–2.22) | 0.137 | 1.42 (0.91–2.23) | 0.127 | 1.31 (0.82–2.08) | 0.261 |
| Life expectancy | 1.04 (0.87–1.24) | 0.650 | 0.99 (0.84–1.17) | 0.888 | 1.04 (0.87–1.23) | 0.689 |
| GDP per capita | 1.00 (1.00–1.00) | 0.129 | 1.00 (1.00–1.00) | 0.199 | 1.00 (1.00–1.00) | 0.164 |
| ROC of the multivariate regression model | 0.7867** | 0.7614** | 0.7547** | |||
Population-adjusted mortality rate univariate and multivariate logistic regression
The univariate associations with population-adjusted COVID-19 deaths per 1 million population were examined for average male BMI, average female BMI, life expectancy, GDP per capita, and nationwide obesity rate. COVID-19 deaths per 1 million population were stratified into ≥ 100 per 1 million, ≥ 150 per 1 million, and ≥ 200 per 1 million (Table V). Only average male BMI and life expectancy were found to be statistically significant in the univariate regression analysis for each of the COVID-19 deaths per 1 million population group. Average male BMI and life expectancy were thus included in the multivariate logistic regression model. While not found to be statistically significant in the univariate logistic regression analysis, we included GDP per capita in the multivariate logistic regression model as a socially important variable (Table VI). In the multivariate analysis, average male BMI (odds ratio (OR) 1.99, 95% CI: 1.02–3.88, p = 0.043; OR = 2.67, 95% CI: 1.16–6.15, p = 0.021; and OR = 2.60, 95% CI: 1.14–5.91, p = 0.022) and life expectancy (OR = 1.62, 95% CI: 1.21–2.15, p = 0.001; OR = 1.85, 95% CI: 1.28–2.67, p = 0.001; and OR = 1.71, 95% CI: 1.23–2.36, p = 0.001) were found to have significant associations in each of the stratified groups.
Table V
Univariate logistic regression for association with population-adjusted cause-specific death rates due to COVID-19
Table VI
Multivariate logistic regression for association with population-adjusted mortality rates due to COVID-19
| Variable | Cause-specific deaths ≥ 100 per 1 million population | Cause-specific deaths ≥ 150 per 1 million population | Cause-specific deaths ≥ 200 per 1 million population | |||
|---|---|---|---|---|---|---|
| OR | P-value | OR | P-value | OR | P-value | |
| Average male BMI | 1.99 (1.02–3.88) | 0.043* | 2.67 (1.16–6.15) | 0.021* | 2.60 (1.14–5.91) | 0.022* |
| Life expectancy | 1.62 (1.21–2.15) | 0.001* | 1.85 (1.28–2.67) | 0.001* | 1.71 (1.23–2.36) | 0.001* |
| GDP per capita | 0.9999369 (0.9998788–0.999995) | 0.033* | 0.9999379 (0.9998717–1.000004) | 0.066 | 0.9999495 (0.9998923–1.000007) | 0.083 |
| ROC of the multivariate regression model | 0.8788** | 0.9168** | 0.9033** | |||
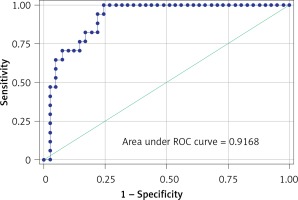
The model showed that GDP per capita was significantly associated with COVID-19 deaths but only in the deaths ≥ 100 per 1 million group. Importantly, the model demonstrated an excellent predictive ability (area under ROC curve ROC 0.8788, 0.9168, and 0.9033 across the analyzed group; Table VI). The model showed the best predictive ability in the deaths ≥ 150 per 1 million strata (sensitivity 70.6%; specificity 87.9%; positive predictive value 70.6%; negative predictive value 87.8%; correctly classified 82.76%). The final model consisting of average male BMI, life expectancy and GDP per capita predicted population-adjusted COVID-19 death rates globally (using a threshold of 150 deaths per million population) (Figure 2).
Discussion
The current study might have major public health implications with novel findings regarding the associations between COVID-19 and obesity. This builds on our previous work where we provided recommendations based on Intensive Care National Audit and Research Centre (ICNARC) United Kingdom (UK) data on COVID-19 critical care patients – that the BMI ≥ 30 was a significant predictor of mortality in this population [2], hence raising the need for targeted algorithm and risk-based management/triage approach [2, 27–29]. We found that male BMI and life expectancy were independent predictors of COVID-19 mortality and not the COVID-19 confirmed cases per million population.
Countries with a nationwide obesity rate of 20–30% (e.g., Brazil, Russia, the UK, Iran, Spain) [30] had a significantly higher (approximately double) number of deaths per million population compared to both those in < 20% and > 30% obesity rate slabs. We postulate that there may be a U-shaped paradoxical relationship between obesity and COVID-19 mortality burden more pronounced in the countries with 20–30% obesity rates. Our findings are relevant especially in the light of the recently released Public Health England (PHE) report on excess weight and COVID-19 [31]. The increased prevalence and disease burden due to excess weight in general, and obesity in particular, is a public health concern globally, with the burden being higher in western countries [32]. The PHE report highlights that the people belonging to Black, Asian and Minority Ethnic (BAME) communities, those living in deprived areas, and those aged 55–74 years are disproportionately affected by excess weight [31]. Moreover, it is well known that the health risks related to excess weight are more prevalent in BAME communities, even at a lower BMI than in those from Caucasian backgrounds. Given the disproportionate impact of COVID-19 on vulnerable communities [33], such as racial/ethnic minority groups, which are particularly vulnerable to increased prevalence and incidence of obesity and diabetes [34], targeted multilevel interventions against obesity may provide protection [35], and hence mitigate the impact of COVID-19.
Notably, the obesity paradox, i.e. the association of higher BMI with lower mortality, longer hospital stays and longer ventilation period, in ICU patients requiring mechanical ventilation, has also been a subject of debate [36, 37]. However, the hypothesis has been challenged [38]. The protective role of obesity, as proposed in this hypothesis, in reduced mortality may be due to lack of adjustment for comorbidities or potential confounders including a history of smoking, disease severity and socioeconomic variables [38]. Moreover, it has been suggested that BMI does not account for body composition, adiposity, and their variations due to gender and ethnicity [39]. It also fails to detect “normal obese subjects” [38]. Last, but not least, since severe infections in general and more specifically COVID-19 represent catabolic and high energy-consuming situations, obese patients may have a more favorable prognosis due to their augmented metabolic reserve [40]. This hypothesis holds also true in heart failure (HF) as the well-known catabolic state in which it seems that patients who are obese have better clinical outcomes compared to their leaner counterparts [40, 41]. Our findings are distinct, as it takes a population or systems-level approach to address the impact of COVID-19 on obese patients. We have included ecological variables such as GDP which are often not considered or adjusted for in clinical trials or case-controlled studies.
We hypothesized that countries with a nationwide obesity rate of > 30% may have better-developed health systems delivering a higher quality of care including tailored treatment options and/or have well-coordinated health services targeted toward obese people embedded within the system. One of the obesity programs’ strategies may have been strongly advising obese people to adhere to physical distancing and wearing masks whenever distancing of 6 feet cannot be ensured [31]. Better treatments and/or well-organized support programs for obese people are likely associated with higher GDP per capita as well. The values of GDP per capita are indeed much higher for countries with a nationwide obesity rate >30%: twice as high GDP per capita in countries with obesity rates of 20–30% (mean $52,818 (SD 42259.32); median $50,244.50 (IQR 16380–69041)) vs. mean $26,145.12 (SD14353.04); median $23,064 (IQR 14088–39162). Five countries in the > 30% stratum are countries with high GDP per capita, i.e. the US, Saudi Arabia, the UAE, Kuwait, and Qatar, presenting 62.5% of the population of the group. While GDP per capita in the > 30% obesity rate group is even higher compared to the < 20% group ($17,600.47 (SD 20265.77); median: $10,511 (IQR 5323–15296)), the latter has a significantly smaller proportion of obese people, which may be responsible for higher mortality being observed in both < 20% and > 30% obesity rate groups compared to the 20–30% group. The countries with nationwide obesity rates > 30% have significantly higher case rates (mean 8287.25 (SD 10780); median 5038 (IQR 1734–9246)) vs. < 20% obesity rate group with mean 2156.53 (SD2605.47); median 837 (IQR 324–3653) and 20-30% obesity rate group (mean 4215.73 (SD 3454.92); median 2736 (IQR 1826–6328)). The countries with higher GDP per capita may be testing more for COVID-19 and thus timely identifying the higher proportion of COVID-19 positive obese people who then receive appropriate care in a timelier manner.
Various mechanisms have been proposed to explain the association between obesity and increased disease severity in COVID-19 hospitalized patients. It is recognized that SARS-CoV-2 has a strong affinity for human angiotensin-converting enzyme 2 (ACE-2) [5]. Adipose tissue also has increased expression of ACE-2 receptors [42]. Moreover, obesity also exacerbates the hyper-inflammatory response (cytokine storm) causing deteriorating lung function capacity and increased need for mechanical ventilation [29]. Telemedicine could be a great enabler in implementing effective prophylactic strategies to reduce the morbidity and mortality burden in this subgroup of patients [43–45].
Our multivariate regression model did not account for cardiovascular disease and diabetes or other comorbidities associated with obesity. However, we believe that, since obesity and other comorbidities have a significant overlap, introducing these variables would introduce multicollinearity effects in the multivariate logistic regression model. BMI as a marker of obesity has been widely contested and is supposedly sub-optimal in elderly patients [46]. Despite the limited accuracy of BMI, it remains one of the most widely used tools to characterize excess weight or obesity around the world [47].
In conclusion, the findings reported in this study are novel, as is the methodological approach of conducting ecological analyses on country-wide data from publicly available sources. Our findings should be interpreted within the context of study design. We anticipate, in light of our findings, that appropriate targeted public health approaches or campaigns could be developed to minimize the risk of infection and morbidity burden due to COVID-19 in countries with a nationwide obesity rate of 20-30%, especially males, who may be more vulnerable to mortality due to COVID-19.
Author notes
The COVID-19 pandemic is causing an unprecedented public health crisis impacting healthcare systems, healthcare workers and communities. The COVID-19 Pandemic Health System REsilience PROGRAM (REPROGRAM) is a not-for-profit consortium of international healthcare physicians, researchers and policymakers formed to champion the safety of healthcare workers, policy development and advocacy for global pandemic preparedness and action.