Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
NEPHROLOGY / RESEARCH PAPER
Inflammation response index (SIRI) is associated with all-cause and cardiovascular mortality in maintenance hemodialysis patients
1
Department of Nephrology, The Second Affiliated Hospital of Soochow University, China
2
Department of Pharmacy, The Second Affiliated Hospital of Soochow University, China
These authors had equal contribution to this work
Submission date: 2024-05-24
Final revision date: 2024-09-19
Acceptance date: 2024-10-12
Online publication date: 2024-10-26
Corresponding author
KEYWORDS
TOPICS
ABSTRACT
Introduction:
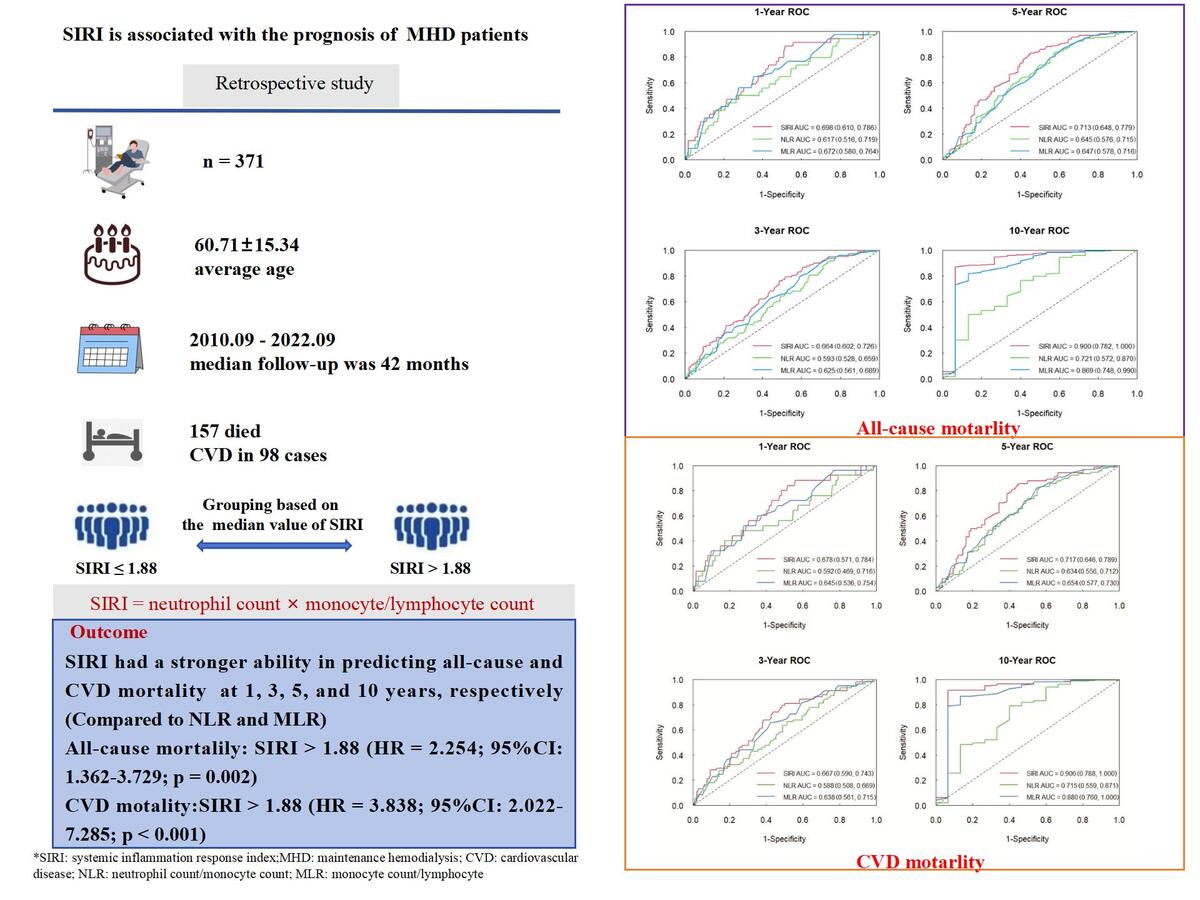
The aim of this study was to investigate the association between inflammation response index (SIRI) on all-cause and cardiovascular (CVD) mortality in maintenance hemodialysis (MHD) patients.
Material and methods:
371 MHD patients were included in this retrospective study. Time-dependent receiver operating characteristic (ROC) curve analysis was used to evaluate the predictive value of SIRI. Patients were categorized into two groups based on the median value of SIRI. Kaplan-Meier survival analysis was used to compare the difference in survival rate. Cox regression analysis was used to analyze all-cause and CVD mortality risk factors, and nomograms were established.
Results:
The average age of the patients was (60.71±15.34), and the median follow-up was 42 months. 157 patients died. SIRI had a predictive value for all-cause and CVD mortality. The AUC of the SIRI to predict the all-cause mortality was 0.698, 0.664, 0.713, and 0.900 at 1, 3, 5, and 10 years, respectively. For CVD mortality, the AUC of the SIRI was 0.678, 0.667, 0.717, and 0.906 at 1, 3, 5, and 10 years, respectively. Kaplan-Meier survival analysis showed that patients with high SIRI levels show a significantly lower survival rate. Multivariate Cox regression analysis showed that SIRI > 1.88 was an independent risk factor for all-cause and CVD mortality.
Conclusions:
SIRI can independently predict all-cause and CVD mortality in MHD patients, which has important value for prognosis.
The aim of this study was to investigate the association between inflammation response index (SIRI) on all-cause and cardiovascular (CVD) mortality in maintenance hemodialysis (MHD) patients.
Material and methods:
371 MHD patients were included in this retrospective study. Time-dependent receiver operating characteristic (ROC) curve analysis was used to evaluate the predictive value of SIRI. Patients were categorized into two groups based on the median value of SIRI. Kaplan-Meier survival analysis was used to compare the difference in survival rate. Cox regression analysis was used to analyze all-cause and CVD mortality risk factors, and nomograms were established.
Results:
The average age of the patients was (60.71±15.34), and the median follow-up was 42 months. 157 patients died. SIRI had a predictive value for all-cause and CVD mortality. The AUC of the SIRI to predict the all-cause mortality was 0.698, 0.664, 0.713, and 0.900 at 1, 3, 5, and 10 years, respectively. For CVD mortality, the AUC of the SIRI was 0.678, 0.667, 0.717, and 0.906 at 1, 3, 5, and 10 years, respectively. Kaplan-Meier survival analysis showed that patients with high SIRI levels show a significantly lower survival rate. Multivariate Cox regression analysis showed that SIRI > 1.88 was an independent risk factor for all-cause and CVD mortality.
Conclusions:
SIRI can independently predict all-cause and CVD mortality in MHD patients, which has important value for prognosis.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.