Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
Editor's Choice
NUTRITION / STATE OF THE ART PAPER
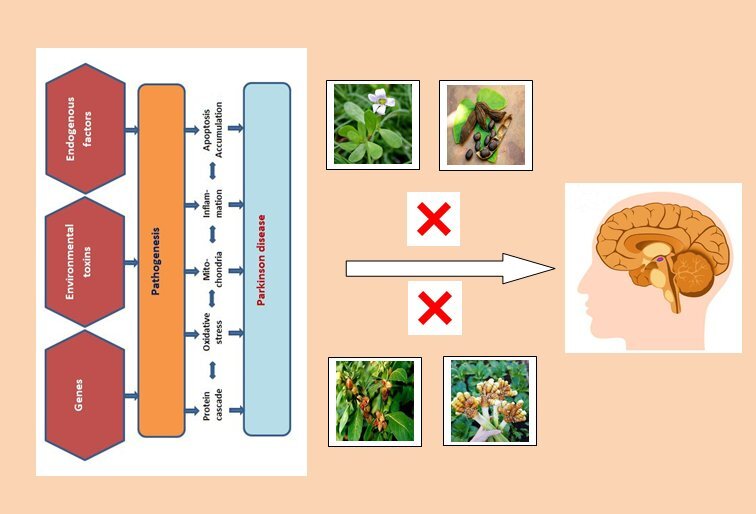
Implications for the role of natural products in Parkinson disease therapy
1
Department of Biological Science, Faculty of Science, King Abdulaziz University, Jeddah, Saudi Arabia
Submission date: 2024-05-10
Final revision date: 2024-08-19
Acceptance date: 2024-08-26
Online publication date: 2024-09-06
Corresponding author
Ashwaq H. Batawi
Department of Biological Science, Faculty of Science, King Abdulaziz University, Saudi Arabia
Department of Biological Science, Faculty of Science, King Abdulaziz University, Saudi Arabia
KEYWORDS
Parkinson’s diseasegenetic and environmental factorsgenetic variantsmitochondriaoxidative stressmedicinal plants
TOPICS
ABSTRACT
Humans still suffer from several nervous system diseases affecting perception and body movement, such as Alzheimer’s and Parkinson’s diseases. Parkinson’s disease is a globally common disease of the nervous system that is characterized by neurodegenerative movement disorders. Patients with Parkinson’s disease are characterized by the slow loss of dopaminergic (DA-ergic) neurons, especially in areas of brain tissue called the substantia nigra pars compacta. However, there is still no clear evidence regarding the factors responsible for development of the disease, which remains vague. There are some indications that oxidative stress and mitochondrial dysfunction are among the main causes of the disease. Parkinson’s patients are still dependent on taking levodopa as the recommended therapeutic drug. This drug, although it has many side effects, slows down the progression of the disease. Therefore, many scientists and pharmacologists are striving to find a potential drug that can halt the disease while minimizing side effects. Research is underway to find effective natural substances against Parkinson’s disease that can renew the vitality of mitochondria and activate their function, as well as diminish the oxidation process in the nerve cells. Therefore, the aim of this review was to highlight the potential role of some natural products from plant sources, such as natural medicinal herbs or marine sources, in protecting neurons and improving their biological functions in order to develop new therapeutic strategies against Parkinson’s disease.
REFERENCES (189)
1.
De Lau L, Breteler M. Epidemiology of Parkinson’s disease. Lancet Neurol 2006; 5: 525-35.
2.
Bostantjopoulou S, Katsarou Z, Karakasis C, Peitsidoue, Milioni D, Rossopoulos N. Evaluation of non-motor symptoms in Parkinson’s disease: an underestimated necessity. Hippokratia 2013; 17: 214-9.
3.
Johansen KK, Waro BJ, Aasly JO. Olfactory dysfunction in sporadic Parkinson’s disease and LRRK2 carriers. Acta Neurol Scand 2014; 129: 300-6.
4.
Koga S, Sekiya H, Kondru N, Ross OA, Dickson DW. Neuropathology and molecular diagnosis of synucleinopathies. Mol Neurodegener 2021; 16: 83.
5.
Jia F, Fellner A, Kumar KR. Monogenic Parkinson’s disease: genotype, phenotype, pathophysiology, and genetic testing. Genes (Basel) 2022; 13: 471.
6.
von Linstow CU, DeLano-Taylor M, Kordower JH, Brundin P. Does developmental variability in the number of midbrain dopamine neurons affect individual risk for sporadic Parkinson’s disease? J Parkinsons Dis 2020; 10: 405-11.
7.
Ascherio A, Schwarzschild MA. The epidemiology of Parkinson’s disease: risk factors and prevention. Lancet Neurol 2016; 15: 1257-72.
8.
Breckenridge CB, Berry C, Chang ET, Sielken RL, Mandel JS. Association between Parkinson’s disease and cigarette smoking, rural living, well-water consumption, farming and pesticide use: systematic review and meta-analysis. PLoS One 2016; 11: e0151841.
9.
Han Y, Wu D, Wang Y, Xie J, Zhang Z. Skin alpha-synuclein deposit patterns: a predictor of Parkinson’s disease subtypes. EBioMedicine 2022; 80: 104076.
10.
Liao Q, Li NN, Mao XY, et al. MTHFR C667T variant reduces risk of sporadic Parkinson’s disease in ethnic Chinese. Acta Neurol Scand 2014; 130: e30-4.
11.
Wang Z, Liu X, Yang BZ, Gelernter J. The role and challenges of exome sequencing in studies of human diseases. Front Genet 2013; 4: 160.
12.
Nalls MA, Blauwendraat C, Vallerga CL, et al. Identification of novel risk loci, causal insights, and heritable risk for Parkinson’s disease: a meta-analysis of genome-wide association studies. Lancet Neurol 2019; 18: 1091-102.
13.
Goldman SM, Marek K, Ottman R, et al. Concordance for Parkinson’s disease in twins: a 20-year update. Ann Neurol 2019; 85: 600-5.
14.
Day JO, Mullin S. The genetics of Parkinson’s disease and implications for clinical practice. Genes (Basel) 2021; 12: 1006.
15.
Correia Guedes L, Mestre T, Outeiro TF, Ferreira JJ. Are genetic and idiopathic forms of Parkinson’s disease the same disease? J Neurochem 2020; 152: 515-22.
16.
Jiang T, Sun Q, Chen S. Oxidative stress: a major pathogenesis and potential therapeutic target of antioxidative agents in Parkinson’s disease and Alzheimer’s disease. Prog Neurobiol 2016; 147: 1-19.
17.
Michel PP, Hirsch EC, Hunot SP. Understanding dopaminergic cell death pathways in Parkinson disease. Neuron 2016; 90: 675-91.
18.
Ye H, Robak LA, Yu M, Cykowski M, Shulman JM. Genetics and pathogenesis of Parkinson’s syndrome. Annu Rev Pathol 2023; 18: 95-121.
19.
Verstreken P, Ly CV, Venken KJT, Koh TW, Zhou Y, Bellen HJ. Synaptic mitochondria are critical for mobilization of reserve pool vesicles at Drosophila neuromuscular junctions. Neuron 2005; 47: 365-78.
20.
Yuan H, Zhang ZW, Liang LW, et al. Treatment strategies for Parkinson’s disease. Neurosci Bull 2010; 26: 66-76.
21.
LeWitt PA, Fahn S. Levodopa therapy for Parkinson disease a look backward and forward. Neurology 2016; 86: S3-12.
22.
Connolly BS, Lang AE. Pharmacological treatment of Parkinson disease: a review. JAMA 2014; 311: 1670-83.
23.
Sarrafchi A, Bahmani M, Shirzad H, Rafieian-Kopaei M. Oxidative stress and Parkinson’s disease: new hopes in treatment with herbal antioxidants. Curr Pharm Des 2016, 22: 238-46.
24.
Van der Merwe C, Van Dyk HC, Engelbrecht L, et al. Curcumin rescues a PINK1 knock down SH-SY5Y cellular model of Parkinson’s disease from mitochondrial dysfunction and cell death. Mol Neurobiol 2017; 54: 2752-62.
25.
Yadav SK, Rai SN, Singh SP. Mucuna pruriens reduces inducible nitric oxide synthase expression in Parkinsonian mice model. J Chem Neuroanat 2017; 80: 1-10.
26.
Schapira AH, Tolosa EJNRN. Molecular and clinical prodrome of Parkinson disease: implications for treatment. Nat Rev Neurol 2010; 6: 309-17.
27.
Schapira AJE. Challenges to the development of disease-modifying therapies in Parkinson’s disease. Eur J Neurol 2011; 18: 16-21.
28.
Sharma R, Martins N. Telomeres, DNA damage and ageing: potential leads from ayurvedic rasayana (Anti-Ageing) drugs. J Clin Med 2020; 9: 2544.
29.
Sharma R, Prajapati PK. Predictive, preventive and personalized medicine: leads from ayurvedic concept of prakriti (human constitution). Curr Pharmacol Rep 2020; 6: 441-45.
30.
Surmeier DJ, Guzman JN, Sanchez-Padilla JJC. Calcium, cellular aging, and selective neuronal vulnerability in Parkinson’s disease. Cell Calcium 2010; 47: 175-82.
31.
Tellier JM, Kalejs NI, Leonhardt BS, Cannon D, HÖÖk TO, Collingsworth PD. Widespread prevalence of hypoxia and the classification of hypoxic conditions in the Laurentian Great Lakes. J Gt Lakes Res 2022; 48: 13-23.
32.
Richardson JR, Shalat SL, Buckley B, et al. Elevated serum pesticide levels and risk of Parkinson disease. Arch Neurol 2009; 66: 870-5.
33.
Xiao XQ, Zhang HY, Tang XCJJ. Huperzine A attenuates amyloid -peptide fragment 25-35-induced apoptosis in rat cortical neurons via inhibiting reactive oxygen species formation and caspase-3 activation. J Neurosci Res 2002; 67: 30-6.
34.
Ascherio A, Zhang SM, Hernán MA, et al. Prospective study of caffeine consumption and risk of Parkinson’s disease in men and women. Ann Neurol 2001; 50: 56-63.
35.
Warner TT, Schapira AH. Genetic and environmental factors in the cause of Parkinson’s disease. Ann Neurol 2003; 53: S16-25.
36.
Luo C, Song W, Chen Q, et al. Reduced functional connectivity in early-stage drug-naive Parkinson’s disease: a resting state fMRI study. Neurobiol Aging 2014; 35: 431-41.
37.
Prodoehl J, Burciu RG, Vaillancourt DEJ. Resting state functional magnetic resonance imaging in Parkinson’s disease. Curr Neurol Neurosci Rep 2014; 14: 448.
38.
Jellinger KA. Formation and development of Lewy pathology: a critical update. J Neurol 2009; 256: 270-9.
39.
Wakabayashi K, Tanji K, Odagiri S, Miki Y, Mori F, Takahashi H. The Lewy body in Parkinson’s disease and related neurodegenerative disorders. Mol Neurobiol 2013; 47: 495-508.
40.
Reiman EM, Langbaum JB, Fleisher AS, et al. Alzheimer’s prevention initiative: a plan to accelerate the evaluation of presymptomatic treatments. J Alzheimer’s Dis 2011; 26: 321-9.
41.
Tarakad A, Jankovic J. Recent advances in understanding and treatment of Parkinson’s disease. Fac Rev 2020; 9: 6.
42.
Thenganatt MA, Jankovic J. Parkinson disease subtypes. JAMA Neurol 2014; 71: 499-504.
43.
Domingo A, Klein C. Genetics of Parkinson disease. Handb Clin Neurol 2018; 147: 211-27.
44.
Bandres-Ciga S, Diez-Fairen M, Kim JJ, et al. Genetics of Parkinson’s disease: an introspection of its journey towards precision medicine. Neurobiol Dis 2020; 137: 104782.
45.
Ysselstein D, Shulman JM, Krainc D. Emerging links between pediatric lysosomal storage diseases and adult parkinsonism. Mov Disord 2018; 34: 614-24.
46.
Shahmoradian SH, Lewis AJ, Genoud C, et al. Lewy pathology in Parkinson’s disease consists of crowded organelles and lipid membranes. Nat Neurosci 2019; 22: 1099-109.
47.
Obeso JA, Stamelou M, Goetz CG, et al. Past, present, and future of Parkinson’s disease: a special essay on the 200th anniversary of the shaking palsy. Mov Disord 2017; 32: 1264-310.
48.
Grieco M, Giorgi A, Gentile MC, et al. Glucagon-like peptide-1: a focus on neurodegenerative diseases. Front Neurosci 2019; 13: 1112.
49.
Golpich M, Amini E, Mohamed Z, Azman Ali R, Mohamed Ibrahim N, Ahmadiani A. Mitochondrial dysfunction and biogenesis in neurodegenerative diseases: pathogenesis and treatment. CNS Neurosci Ther 2017; 23: 5-22.
50.
Rahman MH, Bajgai J, Fadriquela A, et al. Redox effects of molecular hydrogen and its therapeutic efficacy in the treatment of neurodegenerative diseases. Processes 2021; 9: 308.
51.
Ullah R, Khan M, Shah SA, Saeed K, Kim MO. Natural antioxidant anthocyanins-a hidden therapeutic candidate in metabolic disorders with major focus in neurodegeneration. Nutrients 2019; 11: 1195.
52.
Singh A, Kukreti R, Saso L, Kukreti S. Oxidative stress: a key modulator in neurodegenerative diseases. Molecules 2019; 24: 1583.
53.
Buendia I, Michalska P, Navarro E, Gameiro I, Egea J, Leon R. Nrf2-are pathway: an emerging target against oxidative stress and neuroinflammation in neurodegenerative diseases. Pharmacol Ther 2016; 157: 84-104.
54.
Gelders G, Baekelandt V, Van der Perren A. Linking neuroinflammation and neurodegeneration in Parkinson’s disease. J Immunol Res 2018; 2018: 4784268.
55.
Leszek J, Barreto GE, Gasiorowski K, Koutsouraki E, Avila-Rodrigues M, Aliev G. Inflammatory mechanisms and oxidative stress as key factors responsible for progression of neurodegeneration: role of brain innate immune system. CNS Neurol. Disord Drug Targets 2016; 15: 329-36.
56.
Stephenson J, Nutma E, van der Valk P, Amor S. Inflammation in CNS neurodegenerative diseases. Immunology 2018; 154: 204-19.
57.
Thurgur H, Pinteaux E. Microglia in the neurovascular unit: blood-brain barrier-microglia interactions after central nervous system disorders. Neuroscience 2019; 405: 55-67.
58.
Voet S, Prinz M, van Loo G. Microglia in central nervous system inflammation and multiple sclerosis pathology. Trends Mol Med 2019; 25: 112-23.
59.
Cardenas C, Lovy A, Silva-Pavez E, et al. Cancer cells with defective oxidative phosphorylation require endoplasmic reticulum-to-mitochondria Ca2+ transfer for survival. Sci Signal 2020; 13: eaay1212.
60.
Panov A, Dikalov S, Shalbuyeva N, Hemendinger R, Greenamyre JT, Rosenfeld J. Species- and tissue-specific relationships between mitochondrial permeability transition and generation of ROS in brain and liver mitochondria of rats and mice. Am J Physiol Cell Physiol 2007; 292: C708-18.
61.
Kent JA, Patel V, Varela NA. Gender disparities in health care. Mt Sinai J Med 2012; 79: 555-9.
62.
RahmanH, Bajgai J, Fadriquela A, et al. Therapeutic potential of natural products in treating neurodegenerative disorders and their future prospects and challenges. Molecules 2021; 26: 5327.
63.
Mathur A, Verma SK, Purohit R, et al. Pharmacological investigation of Bacopa monnieri on the basis of antioxidant, antimicrobial and anti-inflammatory properties. J Chem Pharm Res 2010; 2: 191-8.
64.
Kumar S, Mondal AC. Neuroprotective, neurotrophic and anti-oxidative role of Bacopa monnieri on CUS induced model of depression in rat. Neurochem Res 2016; 41: 3083-94.
65.
Uabundit N, Wattanathorn J, Mucimapura S, Ingkaninan K. Cognitive enhancement and neuroprotective effects of Bacopa monnieri in Alzheimer’s disease model. J Ethnopharmacol 2010; 127: 26-31.
66.
Morgan A, Stevens J. Does Bacopa monnieri improve memory performance in older persons? Results of a randomized, placebo-controlled, double-blind trial. J Altern Complement Med 2010; 16: 753-9.
67.
Hazra S, Kumar S, Saha GK, Mondal AC. Reversion of BDNF, Akt and CREB in hippocampus of chronic unpredictable stress induced rats: effects of phytochemical. Bacopa Monnieri. Psychiatry Invest 2017; 14: 74-80.
68.
Singh B, Pandey S, Verma R, Ansari JA, Mahdi AA. Comparative evaluation of extract of Bacopa monnieri and Mucuna pruriens as neuroprotectant in MPTP model of Parkinson’s disease. Ind J Exp Biol 2016; 54: 758-66.
69.
Shinomol GK, Mythri RB, Bharath MMS. Bacopa monnieri extract offsets rotenone-induced cytotoxicity in dopaminergic cells and oxidative impairments in mice brain. Cell Mol Neurobiol 2012; 32: 455-65.
70.
Siddique YH, Mujtaba SF, Faisal M, Jyoti S, Naz F. The effect of Bacopa monnieri leaf extract on dietary supplementation in transgenic Drosophila model of Parkinson’s disease. Eur J Integr Med 2014; 6: 571-80.
71.
Concessao P, Bairy LK, Raghavendra AP. Protective effect of Mucuna pruriens against arsenic-induced liver and kidney dysfunction and neurobehavioral alterations in rats. Vet World 2020; 13: 1555-66.
72.
Soumyanath A, Denne T, Hiller A, Ramachandran S, Lynne Shinto L. Analysis of Levodopa content in commercial mucuna pruriens products using high-performance liquid chromatography with fluorescence detection. J Altern Complement Med 2018; 24: 182-6.
73.
Jansen RLM, Brogan B, Whitworth AJ, Okello EJ. Effects of five ayurvedic herbs on locomotor behaviour in a drosophila melanogaster parkinson’s disease model. Phytother Res 2014; 28: 1789-95.
74.
Poddighe S, De Rose F, Marotta R, et al. Mucuna pruriens (Velvet bean) rescues motor, olfactory, mitochondrial and synaptic impairment in PINK1 B9 Drosophila melanogaster genetic model of Parkinson’s disease. PLoS One 2014; 9: e110802.
75.
Singhal B, Lalkaka J, Sankhla C. Epidemiology and treatment of Parkinson’s disease in India. Parkinsonism Relat Disord 2003; 9: 105-9.
76.
Dhanasekaran M, Tharakan B, Manyam BV. Antiparkinson drug: mucuna pruriens shows antioxidant and metal chelating activity. Phytother Res 2008; 22: 6-11.
77.
Khalil WKB, Ahmed KA, Park MH, Kim YT, Park HH, Abdel-Wahhab MA. The inhibitory effects of garlic and Panax ginseng extract standardized with ginsenoside Rg3 on the genotoxicity, biochemical and histological changes induced by ethylenediaminetetraacetic acid in male rats. Arch Toxicol 2008; 82: 183-95.
79.
Sun GY, Li R, Cui J, et al. Withania somnifera and its withanolides attenuate oxidative and inflammatory responses and up-regulate antioxidant responses in BV-2 microglial cells. Neuromol Med 2016; 18: 241-52.
80.
Bhattacharya SK, Bhattacharya A, Sairam K, Ghosal S. Anxiolytic-antidepressant activity of Withania somnifera glycowithanolides: an experimental study. Phytomedicine 2000; 7: 463-9.
81.
Rai M, Jogee PS, Agarkar G, Santos CA. Anticancer activities of Withania somnifera: current research, formulations, and future perspectives. Pharm Biol 2016; 54: 189-97.
82.
Shivamurthy S, Manchukonda RS, Ramadas D. Evaluation of learning and memory enhancing activities of protein extract of Withania somnifera (Ashwagandha) in Wistar albino rats. Int J Basic Clin Pharmacol 2016; 5: 453-7.
83.
RajaSankar S, Manivasagam T, Sankar V, et al. Withania somnifera root extract improves catecholamines and physiological abnormalities seen in a Parkinson’s disease model mouse. J Ethnopharmacol 2009; 125: 369-73.
84.
Prakash J, Yadav SK, Chouhan S, Singh SP. Neuroprotective role of Withania somnifera root extract in Maneb-Paraquat induced mouse model of parkinsonism. Neurochem Res 2013; 38: 972-80.
85.
Sankar S, Manivasagam T, Krishnamurti A, Ramanathan M. The neuroprotective effect of Withania somnifera root extract in MPTP- intoxicated mice: an analysis of behavioral and biochemical varibles. Cell Mol Biol Lett 2007; 12: 473-81.
86.
Motterlini R, Foresti R, Bassi R, Green CJ. Curcumin, an antioxidant and anti-inflammatory agent, induces heme oxygenase-1 and protects endothelial cells against oxidative stress. Free Radic Biol Med 2000; 28: 1303-12.
87.
Bundy R, Walker AF, Middleton RW, Booth J. Turmeric extract may improve irritable bowel syndrome symptomology in otherwise healthy adults: a pilot study. J Altern Complement Med 2004; 10: 1015-8.
88.
Srivastava S, Saksena AK, Khattri S, Kumar S, Dagur RS. Curcuma longa extract reduces inflammatory and oxidative stress biomarkers in osteoarthritis of knee: a four-month, double-blind, randomized, placebo-controlled trial. Inflammopharmacology 2016; 24: 377-88.
89.
Gunes H, Gulen D, Mutlu R, Gumus A, Tas T, Topkaya AE. Antibacterial effects of curcumin: an in vitro minimum inhibitory concentration study. Toxicol Ind Health 2016; 32: 246-50.
90.
Bala K, Tripathy BC, Sharma D. Neuroprotective and anti-ageing effects of curcumin in aged rat brain regions. Biogerontology 2006; 7: 81-9.
91.
Allegra A, Innao V, Russo S, Gerace D, Alonci A, Musolino C. Anticancer activity of curcumin and its analogues: preclinical and clinical studies. Cancer Invest 2017; 35: 1-22.
92.
Wang Q, Sun AY, Simonyi A, et al. Neuroprotective mechanisms of curcumin against cerebral ischemia-induced neuronal apoptosis and behavioral deficits. J Neurosci Res 2005; 82: 138-48.
93.
Jiang J, Wang W, Sun YJ, Hu M, Li F, Zhu DY. Neuroprotective effect of curcumin on focal cerebral ischemic rats by preventing blood-brain barrier damage. Eur J Pharmacol 2007; 561: 54-62.
94.
Garcia-Alloza M, Borrelli LA, Rozkalne A, Hyman BT, Bacskai BJ. Curcumin labels amyloid pathology in vivo, disrupts existing plaques, and partially restores distorted neurites in an Alzheimer mouse model. J Neurochem 2007; 102: 1095-104.
95.
Mythri RB, Srinivas Bharath MM. Curcumin: a potential neuroprotective agent in Parkinson’s disease. Curr Pharm Des 2012; 18: 91-9.
96.
Motawi TK, Sadik NAH, Hamed MA, Ali SA, Khalil WKB, Ahmed YR. Potential therapeutic effects of antagonizing adenosine A2A receptor, curcumin and niacin in rotenone induced Parkinson’s disease mice model. Mol Cell Biochem 2020; 465: 89-102.
97.
Gouda W, Hafiz NA, Mageed L, et al. Effects of nano-curcumin on gene expression of insulin and insulin receptor. Bull Natl Res Cent 2019; 43: 128.
98.
Storka A, Vcelar B, Klickovic U, et al. Safety, tolerability and pharmacokinetics of liposomal curcumin in healthy humans. Int J Clin Pharmacol Ther 2015; 53: 54-65.
99.
Chan EWC, Lim YY, Chew YL. Antioxidant activity of Camellia sinensis leaves and tea from a lowland plantation in Malaysia. Food Chem 2007; 102: 1214-22.
100.
Tulsulkar J, Shah ZA. Ginkgo biloba prevents transient global ischemia-induced delayed hippocampal neuronal death through antioxidant and anti-inflammatory mechanism. Neurochem Int 2013; 62: 189-97.
101.
Zhou X, Qi Y, Chen T. Long-term pre-treatment of antioxidant Ginkgo biloba extract EGb-761 attenuates cerebral-ischemia-induced neuronal damage in aged mice. Biomed Pharmacother 2017; 85: 256-63.
102.
El-Ghazaly MA, Sadik NAH, Rashed ER, Abd-El-Fattah AA. Neuroprotective effect of EGb7611 and low-dose whole-body g-irradiation in a rat model of Parkinson’s disease. Toxicol Ind Health 2015; 31: 1128-43.
103.
Chen L, Zhang C, Han Y, et al. Gingko biloba extract (EGb) inhibits oxidative stress in neuro 2A cells overexpressing APPsw. Biomed Res Int 2019; 2019: 7034983.
104.
Singh SK, Srivastav S, Castellani RJ, Plascencia-Villa G, Perry G. Neuroprotective and antioxidant effect of Ginkgo biloba extract against AD and other neurological disorders. Neurotherapeutics 2019; 16: 666-74.
105.
Chang KH, Chen CM. The role of oxidative stress in Parkinson’s disease. Antioxidants (Basel) 2020; 9: 597.
106.
Cabrera C, Artacho R, Giménez R. Beneficial effects of green tea – a review. J Am Coll Nutr 2006; 25: 79-99.
107.
Khan N, Mukhtar H. Tea polyphenols for health promotion. Life Sci 2007; 81: 519-33.
108.
Chen H, Zhang M, Qu Z, Xie B. Antioxidant activities of different fractions of polysaccharide conjugates from green tea (Camellia Sinensis). Food Chem 2008; 106: 559-63.
109.
Thakur P, Chawla R, Goel R, Narula A, Arora R, Sharma RK. Antibacterial activity of aquo-alcoholic extract of camellia sinensis against isolates of carbapenem resistant Escherichia coli and food borne pathogens. Int J Biol Pharm Res 2015; 6: 606-16.
110.
Chen BT, Li WX, He RR, et al. Anti-inflammatory effects of a polyphenols-rich extract from tea (Camellia sinensis) flowers in acute and chronic mice models. Oxid Med Cell Longev 2012; 2012: 537923.
111.
Boehm K, Borrelli F, Ernst E, et al. Green tea (Camellia sinensis) for the prevention of cancer. Cochrane Database Syst Rev 2009; 2009: CD005004.
112.
Kim HR, Rajaiah R, Wu QL, et al. Green tea protects rats against autoimmune arthritis by modulating disease-related immune events. J Nutr 2008; 138: 2111-6.
113.
Boadas-Vaello P, Verdú E. Epigallocatechin-3-gallate treatment to promote neuroprotection and functional recovery after nervous system injury. Neural Regener Res 2015; 10: 1390.
114.
Tanaka K, Miyake Y, Fukushima W, et al. Intake of Japanese and Chinese teas reduces risk of Parkinson’s disease. Parkinsonism Relat Disord 2011; 17: 446-50.
115.
Levites Y, Weinreb O, Maor G, Youdim MBH, Mandel S. Green tea polyphenol (-)-epigallocatechin-3-gallate prevents N-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-induced dopaminergic neurodegeneration. J Neurochem 2001; 78: 1073-82.
116.
Guo S, Yan J, Yang T, Yang X, Bezard E, Zhao B. Protective effects of green tea polyphenols in the 6-OHDA rat model of Parkinson’s disease through inhibition of ROS-NO pathway. Biol Psychiatry 2007; 62: 1353-62.
117.
Sharangi AB. Medicinal and therapeutic potentialities of tea (Camellia sinensis L.) –- a review. Food Res Int 2009; 42: 529-35.
118.
Leung LK, Su Y, Chen R, Zhang Z, Huang Y, Chen ZY. Theaflavins in black tea and catechins in green tea are equally effective antioxidants. J Nutr 2001; 131: 2248-51.
119.
Joghataie MT, Roghani M, Negahdar F, Hashemi L. Protective effect of caffeine against neurodegeneration in a model of Parkinson’s disease in rat: behavioral and histochemical evidence. Parkinsonism Relat Disord 2004; 10: 465-8.
120.
Chaturvedi RK, Shukla S, Seth K, et al. Neuroprotective and neurorescue effect of black tea extract in 6-hydroxydopamine-lesioned rat model of Parkinson’s disease. Neurobiol Dis 2006; 22: 421-34.
121.
Anandhan A, Tamilselvam K, Radhiga T, Rao S, Essa MM, Manivasagam T. The aflavin, a black tea polyphenol, protects nigral dopaminergic neurons against chronic MPTP/probenecid induced Parkinson’s disease. Brain Res 2012; 1433: 104-13.
122.
Tulipani S, Romandini S, Busco F, Bompadre S, Mezzetti B, Battino M. Ascorbate, not urate, modulates the plasma antioxidant capacity after strawberry intake. Food Chem 2009; 117: 181-8.
123.
Balk E, Chung M, Raman G, et al. B vitamins and berries and age-related neurodegenerative disorders. Evid Rep Technol Assess (Full Rep) 2006; 134: 1-161.
124.
Lhaj ZA, Ibork H, El Idrissi S, et al. Bioactive strawberry fruit (Arbutus unedo L.) extract remedies paraquat-induced neurotoxicity in the offspring prenatally exposed rats. Front Neurosci 2023; 17: 1244603.
125.
Amro M, Teoh S, Norzana A, Srijit D. The potential role of herbal products in the treatment of Parkinson’s disease. Clin Ter 2018; 169: e23-33.
126.
Li J, Long X, Hu J, et al. Multiple pathways for natural product treatment of Parkinson’s disease: a mini review. Phytomedicine 2019; 60: 152954.
127.
Cheng YF, Zhu GQ, Wang M, et al. Involvement of ubiquitin proteasome system in protective mechanisms of Puerarin to MPP+-elicited apoptosis. Neurosci Res 2009; 63: 52-8.
128.
Silva AH, Fonseca FN, Pimenta AT, et al. Pharmacognostical analysis and protective effect of standardized extract and rizonic acid from Erythrina velutina against 6-hydroxydopamineinduced neurotoxicity in Sh-Sy5Y cells. Pharmacogn Mag 2016; 12: 307-12.
129.
Rahman MM, Rahaman MS, Islam MR, et al. Role of phenolic compounds in human disease: current knowledge and future prospects. Molecules 2022; 27: 233.
130.
Lu KT, Ko MC, Chen BY, et al. Neuroprotective effects of resveratrol on MPTP-induced neuron loss mediated by free radical scavenging. J Agric Food Chem 2008; 56: 6910-3.
131.
Jin F, Wu Q, Lu YF, Gong QH, Shi JSJE. Neuroprotective effect of resveratrol on 6-OHDA-induced Parkinson’s disease in rats. Eur J Pharmacol 2008; 600: 78-82.
132.
Rezaei M, Nasri S, Roughani M, Niknami Z, Ziai SA. Peganum Harmala L. extract reduces oxidative stress and improves symptoms in 6-Hydroxydopamine-induced Parkinson’s disease in rats. Iran J Pharm Res 2016; 15: 275-81.
133.
Lopez-Real A, Rey P, Soto-Otero R, Mendez-Alvarez E, Labandeira-Garcia J, Lopez-Real A. Angiotensin-converting enzyme inhibition reduces oxidative stress and protects dopaminergic neurons in a 6-hydroxydopamine rat model of Parkinsonism. J Neurosci Res 2005; 81: 865-73.
134.
Im HI, Joo WS, Nam E, Lee ES, Hwang Y, Kim Y. Baicalein prevents 6-hydroxydopamine-induced dopaminergic dysfunction and lipid peroxidation in mice. J Pharmacol Sci 2005; 98: 185-9.
135.
Chen HQ, Jin ZY, Wang XJ, Xu XM, Deng L, Zhao J. Luteolin protects dopaminergic neurons from inflammation-induced injury through inhibition of microglial activation. Neurosci Lett 2008; 448: 175-9.
136.
Brinkhaus B, Lindner M, Schuppan D, Hahn EJP. Chemical, pharmacological and clinical profile of the East Asian medical plant Centella aslatica. Phytomedicine 2000; 7: 427-48.
137.
Gohil KJ, Patel JA, Gajjar AK. Pharmacological review on Centella asiatica: a potential herbal cure-all. Indian J Pharm Sci 2010; 72: 546-56.
138.
Jia H, Jiang Y, Ruan Y, et al. Tenuigenin treatment decreases secretion of the Alzheimer’s disease amyloid -protein in cultured cells. Neurosci Lett 2004; 367: 123-8.
139.
Memarzia A, Saadat S, Behrouz S, Boskabady MH. Curcuma longa and curcumin affect respiratory and allergic disorders, experimental and clinical evidence: a comprehensive and updated review. Biofactors 2022; 48: 521-51.
140.
Salem MA, El-Shiekh RA, Fernie AR, Alseekh S, Zayed A. Metabolomics-based profiling for quality assessment and revealing the impact of drying of Turmeric (Curcuma longa L.). Sci Rep 2022; 12: 10288.
141.
Kim DS, Park SY, Kim J. Curcuminoids from Curcuma longa L. (Zingiberaceae) that protect PC12 rat pheochromocytoma and normal human umbilical vein endothelial cells from betaA(1-42) insult. Neurosci Lett 2001; 303: 57-61.
142.
Naser AFA, Aziz WM, Ahmed YR, Khalil WKB, Hamed MAA. Parkinsonism-like disease induced by rotenone in rats: treatment role of curcumin, dopamine agonist and adenosine A2A receptor antagonist. Curr Aging Sci 2022; 15: 65-76.
143.
Akhtar MN, Lam KW, Abas F, et al. New class of acetylcholinesterase inhibitors from the stem bark of Knema laurina and their structural insights. Bioorg Med Chem Lett 2011; 21: 4097-103.
144.
Wang YM, Cui QF, Zhao WL, Zhang JY, Wang HQJB. Nrf2/ARE/HO-1 signaling pathway is a new neuroprotective target for Parkinson’s disease. Front Pharmacol 2014; 34: 1125.
145.
Kuribara H, Kishi E, Hattori N, Okada M, Maruyama YJJ. The anxiolytic effect of two oriental herbal drugs in Japan attributed to honokiol from magnolia bark. J Pharm Pharmacol 2000; 52: 1425-9.
146.
Chen JF, Steyn S, Staal R, et al. 8-(3-Chlorostyryl)caffeine may attenuate MPTP neurotoxicity through dual actions of monoamine oxidase inhibition and A2A receptor antagonism. J Biol Chem 2002; 277: 36040-4.
147.
O’Callaghan C, Lewis S. Cognition in Parkinson’s disease. Int Rev Neurobiol 2017; 133: 557-83.
148.
Corona JCJB. Natural compounds for the management of Parkinson’s disease and attention-deficit/hyperactivity disorder. Biomed Res Int 2018; 2018: 4067597.
149.
Empadinhas N, da Costa MS. Diversity, biological roles and biosynthetic pathways for sugar-glycerate containing compatible solutes in bacteria and archaea. Environ Microbiol 2011; 13: 2056-77.
150.
Faria C, Jorge CD, Borges N, Tenreiro S, Outeiro TF, Santos H. Inhibition of formation of -synuclein inclusions by mannosylglycerate in a yeast model of Parkinson’s disease. Biochim Biophys Acta 2013; 1830: 4065-72.
151.
Monciardini P, Iorio M, Maffioli S, Sosio M, Donadio SJM. Discovering new bioactive molecules from microbial sources. Microb Biotechnol 2014; 7: 209-20.
152.
Nam SJ, Kauffman CA, Jensen PR, Fenical WJT. Isolation and characterization of actinoramides A-C, highly modified peptides from a marine Streptomyces sp. Tetrahedron 2011; 67: 6707-12.
153.
Li Y, Li X, Kang JS, Choi HD, Son BW. New radical scavenging and ultraviolet-A protecting prenylated dioxopiperazine alkaloid related to isoechinulin A from a marine isolate of the fungus Aspergillus. J Antibiot 2004; 57: 337-40.
154.
Kajimura Y, Aoki T, Kuramochi K, et al. Neoechinulin A protects PC12 cells against MPP+-induced cytotoxicity. J Antibiot 2008; 61: 330-3.
155.
Zhai A, Zhang Y, Zhu X, et al. Secalonic acid A reduced colchicine cytotoxicity through suppression of JNK, p38 MAPKs and calcium influx. Neurochem Int 2011; 58: 85-91.
156.
Galasso C, Corinaldesi C, Sansone CJA. Carotenoids from marine organisms: biological functions and industrial applications. Antioxidants 2017; 6: 96.
157.
Meenakshi S, Umayaparvathi S, Arumugam M, Balasubramanian T. In vitro antioxidant properties and FTIR analysis of two seaweeds of Gulf of Mannar. Asian Pac J Trop Biomed 2011; 1: S66-70.
158.
Grimmig B, Daly L, Hudson C, Nash K, Bickford PJ. Astaxanthin attenuates neurotoxicity in a mouse model of Parkinson’s disease. Funct Foods Health Dis 2017; 7: 562-76.
159.
Grimmig B, Kim SH, Nash K, Bickford PC, Douglas Shytle RJG. Neuroprotective mechanisms of astaxanthin: a potential therapeutic role in preserving cognitive function in age and neurodegeneration. Geroscience 2017; 39: 19-32.
160.
Gammone MA, Riccioni G, D’Orazio N. Marine carotenoids against oxidative stress: effects on human health. Mar Drugs 2015; 13: 6226-46.
161.
Karaman MW, Herrgard S, Treiber DK, et al. A quantitative analysis of kinase inhibitor selectivity. Nat Biotechnol 2008; 26: 127-32.
162.
Schupp P, Steube K, Meyer C, Proksch P. Anti-proliferative effects of new staurosporine derivatives isolated from a marine ascidian and its predatory flatworm. Cancer Lett 2001; 174: 165-72.
163.
Wakita S, Izumi Y, Nakai T, et al. Staurosporine induces dopaminergic neurite outgrowth through AMPactivated protein kinase/mammalian target of rapamycin signaling pathway. Neuropharmacology 2014; 77: 39-48.
164.
Bharate SB, Sawant SD, Singh PP, Vishwakarma R. Kinase inhibitors of marine origin. Chem Rev 2013; 113: 6761-815.
165.
Fathy RF, Abdel-Rahim EA, Shallan MA, Khalil WKB, Bassem SM, Abdel-Gawad FKH. Assessment of Holothuria atra extracts against synthetic textile dyes induced endocrine disorders, biochemical and genetic alterations in Nile Tilapia (Oreochromis Niloticus). Int J Pharm Res 2021; 13: 3392-9.
166.
Chalorak P, Jattujan P, Nobsathian S, Poomtong T, Sobhon P, Meemon K. Holothuria scabra extracts exhibit anti-Parkinson potential in C. elegans: a model for anti-Parkinson testing. Nutr Neurosci 2018; 21: 427-38.
167.
Xu J, Guo S, Du L, et al. Isolation of cytotoxic glucoerebrosides and long-chain bases from sea cucumber Cucumaria frondosa using high speed counter-current chromatography. J Oleo Sci 2013; 62: 133-42.
168.
Ahmad J, Haider N, Ahmed Khan M, et al. Novel therapeutic interventions for combating Parkinson’s disease and prospects of Nose-to-Brain drug delivery. Biochem Pharmacol 2022; 195: 114849.
169.
Burns J, Buck AC, D’ Souza S, Dube A, Bardien S. Nanophytomedicines as therapeutic agents for Parkinson’s disease. ACS Omega 2023; 8: 42045-61.
170.
Renero-Lecuna C, Iturrioz-Rodríguez N, González-Lavado E, et al. Effect of size, shape, and composition on the interaction of different nanomaterials with HeLa cells. J Nanomaterials 2019; 28: 7518482.
171.
Ahmed Khan M, Haider N, Singh T, et al. Promising biomarkers and therapeutic targets for the management of Parkinson’s disease: recent advancements and contemporary research. Metab Brain Dis 2023; 38: 873-919.
172.
Farah FH, Nanocarriers as delivery systems for therapeutics agents. Int J Pharm Sci Res 2019; 10: 3487-507.
173.
Zhu X, Vo C, Taylor M, Smith BR. Non-spherical micro- and nanoparticles in nanomedicine. Materials Horizons 2019; 6: 1094-121.
174.
Chen P, Wang H, He M, Chen B, Yang B, Hu B. Size-dependent cytotoxicity study of ZnO nanoparticles in HepG2 cells. Ecotoxicol Environ Safety 2019; 171: 337-46.
175.
Chaicherd S, Killingsworth MC, Pissuwan D. Toxicity of gold nanoparticles in a commercial dietary supplement drink on connective tissue fibroblast cells. SN Appl Sci 2019; 1: 336.
176.
Jeevanandam J, Chan YS, Danquah MK. Biosynthesis of metal and metal oxide nanoparticles. ChemBioEng Rev 2016; 3: 55-67.
177.
Naz S, Gul A, Zia M. Toxicity of copper oxide nanoparticles: a review study. IET Nanobiotechnol 2020; 14: 1-13.
178.
Prasad EM, Hung SY. Current therapies in clinical trials of Parkinson’s disease: a 2021 update. Pharmaceuticals 2021; 14: 717.
179.
Sainz V, Conniot J, Matos AI, et al. Regulatory aspects on nanomedicines. Biochem Biophys Res Commun 2015; 468: 504-10.
180.
Hua S, de Matos MBC, Metselaar JM, Storm G. Current trends and challenges in the clinical translation of nanoparticulate nanomedicines: pathways for translational development and commercialization. Front Pharmacol 2018; 9: 790.
181.
Henchcliffe C, Beal MF. Mitochondrial biology and oxidative stress in Parkinson disease pathogenesis Nat Clin Pract Neurol 2008; 4: 600-9.
182.
Naoi M, Wu Y, Shamoto-Nagai M, Maruyama W. Mitochondria in neuroprotection by phytochemicals: bioactive polyphenols modulate mitochondrial apoptosis system, function and structure. Int J Mol Sci 2019; 20: 2451.
183.
Naoi M, Inaba-Hasegawa K, Shamoto-Nagai M, Maruyama W. Neurotrophic function of phytochemicals for neuroprotection in aging and neurodegenerative disorders: modulation of intracellular signaling and gene expression. J Neural Transm (Vienna) 2017; 124: 1515-27.
184.
Caruso G, Torrisi SA, Mogavero MP, et al. Polyphenols and neuroprotection: therapeutic implications for cognitive decline. Pharmacol Ther 2022; 232: 108013.
185.
Patti AM, Al-Rasadi K, Giglio RV, et al. Natural approaches in metabolic syndrome management. Arch Med Sci 2018; 14: 422-41.
186.
Kim HR, Kim WK, Ha AW. effects of phytochemicals on blood pressure and neuroprotection mediated via brain renin-angiotensin system. Nutrients 2019; 11: 2761.
187.
Rzajew J, Radzik T, Rebas E. calcium-involved action of phytochemicals: carotenoids and monoterpenes in the brain. Int J Mol Sci 2020; 21: 1428.
188.
Salemi M, Cosentino F, Lanza G, et al. mRNA expression profiling of mitochondrial subunits in subjects with Parkinson’s disease. Arch Med Sci 2021; 19: 678-86.
189.
Abo-Grisha N, Essawy S, Abo-Elmatty DM, Abdel-Hady Z. Effects of intravenous human umbilical cord blood CD34+ stem cell therapy versus levodopa in experimentally induced Parkinsonism in mice. Arch Med Sci 2013; 9: 1138-51.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.