High-quality cardiopulmonary resuscitation (CPR) is crucial for survival after cardiac arrest. Despite regularly updated guidelines and extensive training efforts, the quality of CPR performed by healthcare providers remains suboptimal [1]. The survival rate for cardiac arrest is still very low, with only 1% to 6% of out-of-hospital cardiac arrest (OHCA) patients and less than 17% of in-hospital cardiac arrest (IHCA) patients surviving [2–4].
Quality control circles (QCC) originated as a business management concept and were most popular in the 1980s [5]. China Hospital Association for Quality Management was established in 2013, and it has been reported that QCC activities have gradually been implemented in the domestic healthcare field in recent years, with significant benefits for improving healthcare quality [6–9]. However, we have not found any studies on the impact of QCC on the quality of emergency CPR. Therefore, to investigate the effect of QCC on the quality of CPR in the emergency department, we conducted this study to compare the quality and outcomes of CPR in emergency patients before and after QCC implementation. Our aim was to determine whether QCC can improve the quality of emergency CPR, thereby enhancing the return of spontaneous circulation (ROSC), in-hospital survival rate, and discharge survival rate.
A retrospective observational study was conducted at Tenth People’s Hospital of Tongji University. Patients were included based on the following criteria: adults (> 18 years) who experienced IHCA and received CPR in the emergency resuscitation room between February 1, 2021 and September 30, 2021, and between February 1, 2022 and September 30, 2022. Exclusion criteria were: 1) incomplete video recordings or failure to obtain necessary data; 2) patients with one of the following obvious and irreversible signs of death: decomposition, postmortem lividity, rigor mortis; 3) family refusal to participate in the study. Patients during the QCC activity period were not included. All patients were divided into pre-QCC and post-QCC groups based on their admission time. Informed consent was obtained from the families of all patients upon admission. This study was approved by the Ethics Committee of the Tenth People’s Hospital of Tongji University (SHSY-IEC-3.0/16-69/08).
Our hospital established a QCC activity promotion team under the supervision of the administration department to explore ways to improve the quality of CPR in the emergency department. This QCC activity was initiated by the management and required the participation of all doctors and nurses in the emergency resuscitation room. The QCC activity focused exclusively on CPR quality, with each session lasting approximately 90 min. QCC activities were held twice a week from October 1 to December 31, 2021. Wednesday sessions began by identifying CPR-related topics, such as chest compression rate and pause times. Videos and records of all patients included in the previous week were discussed in detail during these sessions. Then, all members provided insights and comments based on the latest guidelines, literature, and experiences. Solutions were documented in writing and implemented within the following days. Monday sessions aimed to provide feedback on the issues raised the previous Wednesday. By comparing video recordings before and after the last QCC session, difficulties and prospects for improving CPR quality were identified. In our study CPR in both compared time intervals were performed by the same team.
Three sets of real-time video recording systems (DS-8000 video network DVR, Hikvision, Hangzhou, China) recorded various steps and processes of CPR from different angles. All resuscitation processes were time-stamped and stored on hard drives. Each patient’s medical data were documented in their medical records.
Data collected from medical records included patient age, gender, cause of cardiac arrest, initial rhythm, duration of cardiac arrest, number of rescuers involved, ROSC, in-hospital survival rate, and discharge survival rate. The neurological prognosis of all patients who achieved ROSC was assessed using the Cerebral Performance Category (CPC) score, evaluated at 24 h for surviving patients, and reassessed at discharge.
All video recordings were reviewed by two trained observers using standardized forms to assess CPR quality. Parameters considered included average chest compression rate (AVCR), actual chest compression rate (ACCR), percentage of pause time during chest compressions (PPT), time from monitor alarm to first chest compression (FCT), time from monitor alarm to first manual ventilation (FMT), use of a mechanical chest compressor (MCC, Sunlife Science, Hong Kong), and the number of rescuers. AVCR was calculated as N/T1, ACCR as N/(T1-T2), and PPR as T2/T1 (where N is the total number of chest compressions, T1 is the total chest compression time, and T2 is the chest compression pause time). The MCC was set to a rate of 100 bpm. T2 was defined as any time interval longer than 1 s between consecutive compressions. All data were analyzed using SPSS 23.0 (IBM Corp.). The χ2 test was used for comparing multiple percentages, and either the independent samples t-test or the Mann-Whitney U test was employed for comparing continuous data. P < 0.05 was considered statistically significant.
A total of 114 patients were included in the study, with 52 patients in the pre-QCC group and 62 patients in the post-QCC group. There were no statistically significant differences between the two groups regarding age, gender, weight, initial rhythm, cause of cardiac arrest, duration of cardiac arrest, MCC usage, and the number of rescuers (p > 0.05).
The clinical outcome characteristics of the two groups are presented in Table I. Regarding the primary endpoint, the ROSC rate was significantly higher in the post-QCC group compared to the pre-QCC group (43.5% vs. 25.0%; p = 0.04). For secondary endpoints, the 24-hour survival rate was significantly higher in the post-QCC group compared to the pre-QCC group (30.6% vs. 13.5%; p = 0.03). Similarly, the discharge rate was significantly higher in the post-QCC group compared to the pre-QCC group (17.7% vs. 5.8%; p = 0.05).
Table I
Comparison of patient clinical prognosis between two groups
| Parameter | Pre-QCC Group (n = 52) | Post-QCC Group (n = 62) | P-value |
|---|---|---|---|
| ROSC | 13 (25.0) | 27 (43.5) | 0.04* |
| Survival to hospitalization | 7 (13.5) | 19 (30.6) | 0.03* |
| Survival to hospital discharge | 3 (5.8) | 11 (17.7) | 0.05 |
The neurological outcomes of ROSC patients in both groups are presented in Table II. In the pre-QCC group, 15.4% of ROSC patients had a CPC score of 1 or 2, while the proportion in the post-QCC group was 18.5%. Although there was a relative increase in the CPC scores in the latter group, there was no statistically significant difference (p = 1.00).
Table II
Comparison of CPC scores between two groups
| CPC score* | Pre-QCC Group (n = 13) | Post-QCC Group (n = 27) | P-value |
|---|---|---|---|
| 1 | 1(7.7) | 2 (7.4) | 1.00 |
| 2 | 1 (7.7) | 3 (11.1) | |
| 3 | 3 (23.1) | 7 (25.9) | |
| 4 | 0 (0) | 3 (11.1) | |
| 5 | 8 (61.5) | 12 (44.4) |
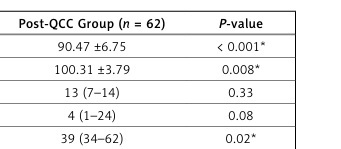
Table III shows the CPR parameters during cardiac arrest for both groups. Compared to the pre-QCC group, the post-QCC group had higher AVCR and ACCR, and significantly shorter FMT, with statistically significant differences (p < 0.05). There were no statistically significant differences in FCT and PPT between the two groups (p > 0.05).
Table III
Comparison of CPR parameters between two groups
| Parameter | Pre-QCC Group (n = 52) | Post-QCC Group (n = 62) | P-value |
|---|---|---|---|
| AVCR [cpm] | 82.40 ±8.51 | 90.47 ±6.75 | < 0.001* |
| ACCR [cpm] | 97.67 ±6.07 | 100.31 ±3.79 | 0.008* |
| PPT (%) | 14 (7–17) | 13 (7–14) | 0.33 |
| FCT [s] | 8 (3–24) | 4 (1–24) | 0.08 |
| FMT [s] | 45 (24–98) | 39 (34–62) | 0.02* |
In this study, we found that QCC improved the ROSC rate and in-hospital survival rate of patients undergoing CPR in the emergency department. QCC also influenced CPR parameters, including AVCR, ACCR, and FMT. Among these improved CPR parameters, AVCR was a key factor in promoting QCC-related ROSC rates and in-hospital survival.
Cerebral resuscitation remains a significant issue in neurosciences. A large-scale clinical trial indicated that only 27% of adults achieve good neurological recovery after CPR [4]. Near infrared spectroscopy (NIRS) is a new technology that enables continuous non-invasive brain oxygen monitoring, which has been widely valued by clinicians. NIRS can also be used in evaluation of the quality of cardiopulmonary resuscitation, early detection of repeat cardiac arrest and prognosis of patients, assessment of autonomic cerebral blood flow regulation, and monitoring of the efficacy of mild hypothermia therapy (TTM) and extracorporeal membrane oxygenation (ECMO) treatment [10]. We carried out bedside NIRS monitoring on all 26 patients admitted to the ICU in this study, who successfully recovered ROSC after cardiopulmonary resuscitation. In this study, we calculated cerebral blood flow regulation ability, cerebral oxygen metabolism and other brain monitoring data based on oxygen saturation of local brain tissue (rScO2) to provide a more individualized and refined treatment plan for patients with cardiac arrest. Our study found that cerebral perfusion in the post-QCC group appeared better than in the pre-QCC group. However, there was no statistically significant difference in neurological outcomes between the two groups. We found that the ROSC rate and 24-hour survival rate of IHCA patients in the post-QCC group were significantly higher than those in the pre-QCC group. However, there was no significant difference in the final neurological outcomes between the two groups. This study is the first retrospective study on QCC in clinical CPR for IHCA patients in China. The results have guiding value for the application of QCC globally, particularly in the Chinese emergency system.
Previous studies have reported a significantly increased risk of out-of-hospital and in-hospital cardiac arrest during the COVID-19 pandemic [11]. The Chinese government fully lifted coronavirus control in December 2022, so the COVID-19 pandemic occurred after December 2022. Our study was not conducted during the COVID-19 epidemic in China. In our study population, the proportion of respiratory failure as the cause of cardiac arrest was 11/52 (21.2%) in pre-QCC group and 13/62 (21.0%) in the post-QCC group, and there was no significant difference between the two groups (p > 0.05), which was similar to the proportion of cardiac arrest caused by respiratory failure in previous studies. In addition, the proportion of patients with COVID-19 recorded in their previous medical history was very low, 4/52 (7.7%) and 5/62 (8.1%) in the pre-QCC and post-QCC groups, respectively, and there was no significant difference between the two groups (p > 0.05). Therefore, we concluded that COVID-19 may increase the incidence of cardiac arrest, but it had little effect on ROSC rate, survival admission rate and discharge rate of patients before and after QCC in our study.
AVCR and ACCR are two parameters that combine chest compression rate and compression pause time, and they can explain the significant improvements in ROSC rate and in-hospital survival rate in the post-QCC group. Higher quality CPR clearly increases the survival chances and quality of life of cardiac arrest patients, with chest compressions being one of the most crucial factors [12, 13]. Adequate chest compressions ensure cardiac output and sufficient tissue perfusion. Studies have reported that higher chest compression rates are significantly associated with better CPR survival rates [14]. Additionally, increasing the number of chest compressions and reducing the proportion of pauses and interruptions in chest compressions are emphasized in the latest CPR guidelines. These changes are crucial for improving the survival rates of cardiac arrest patients.
In conclusion, QCC is a promising and applicable new method for CPR clinical practice in emergency resuscitation rooms. It improves the ROSC rate and in-hospital survival rate in emergency CPR practice. It also affects CPR parameters, including AVCR, ACCR, and FMT. Among these improved CPR parameters, AVCR and ACCR are key factors promoting the QCC-related ROSC rate and in-hospital survival.