Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
LIPID DISORDERS / RESEARCH PAPER
Impact of Lipid-Lowering Drug Targets on Genetic Links with Diabetic Retinopathy
1
The Second Affiliated Hospital of Xuzhou Medical University,, China
2
Department of Endocrinology, The Second Affiliated Hospital of Xuzhou Medical University, China
Submission date: 2024-09-03
Final revision date: 2024-12-29
Acceptance date: 2024-12-30
Online publication date: 2025-04-20
Corresponding author
Kuanlu Fan
Department of Endocrinology, The Second Affiliated Hospital of Xuzhou Medical University, 84 Huaihai West Road, Quanshan District, Xuzhou Ci, China
Department of Endocrinology, The Second Affiliated Hospital of Xuzhou Medical University, 84 Huaihai West Road, Quanshan District, Xuzhou Ci, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
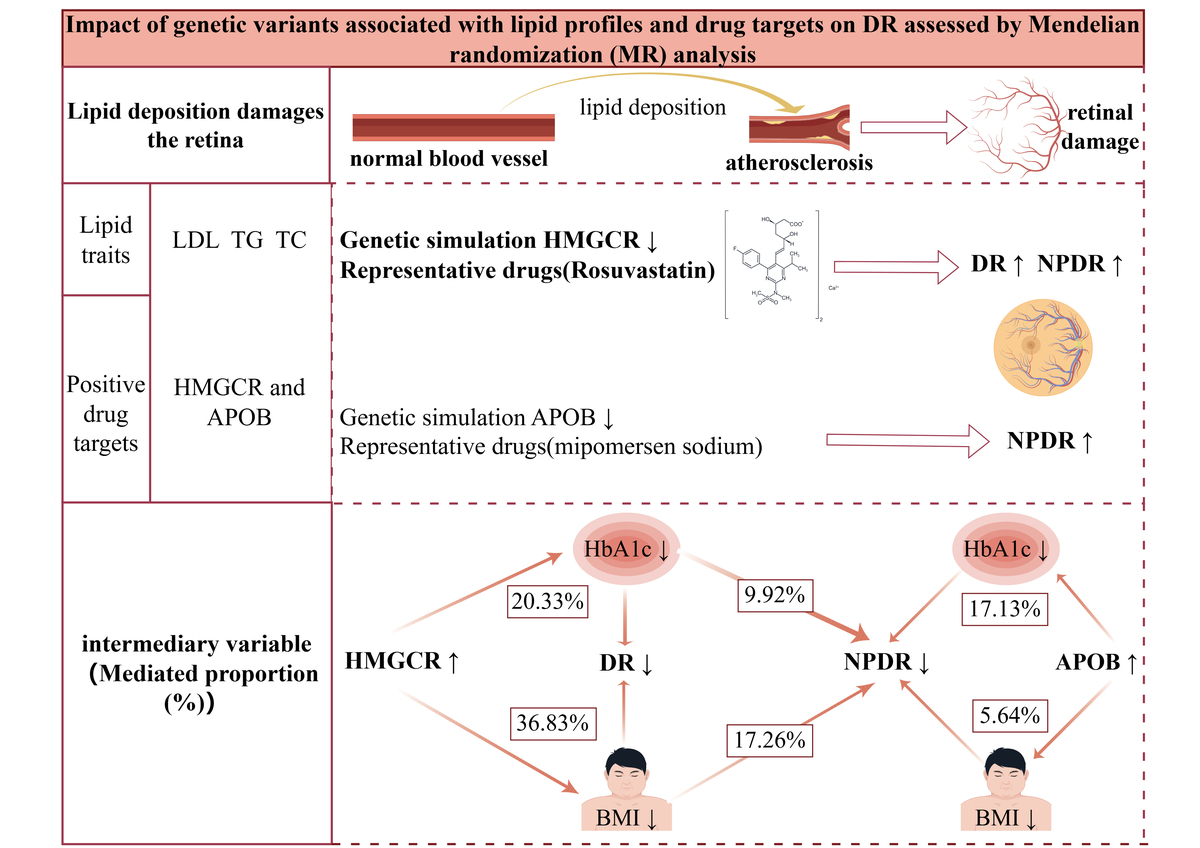
Lipid metabolism is pivotal in diabetic retinopathy (DR) development. Nevertheless, the relationship between lipid-lowering drugs and the risk of DR remains controversial. This study utilized Mendelian randomization (MR) to investigate the potential effects of pharmacological targets for lowering lipid levels on DR and to clarify the causal link between blood lipid characteristics and DR.
Material and methods:
The data comprised genetic variations related to lipid traits and genetic variations associated with lipid-lowering drug targets obtained from the Global Lipid Consortium. Total DR, non-proliferative DR (NPDR), and proliferative DR (PDR) were sourced from the Finnish R9 database. Lipid-lowering drug targets were tested using inverse variance-weighted MR (IVW-MR) and statistics-based MR (SMR). Colocalization and mediation analysis were conducted to validate the results and explore potential mediating factors.
Results:
Results: A reduced risk of total DR and NPDR was linked to genetically improved 3-hydroxy-3-methylglutaryl-CoA reductase (HMGCR) (OR = 0.62; 95% CI: 0.46–0.83; p = 1.30× 10^-2; OR = 0.49; 95% CI :0.34–0.70; p = 9.70× 10^-4). Strong colocalization (PP.H4 = 0.85) was observed between whole blood tissue HMGCR expression and a significant MR relationship with total DR (OR = 0.66; 95% CI: 0.52–0.85; p = 7.31× 10^-4). Furthermore, Body mass index (BMI)and glycated hemoglobin (HbA1c) are critical factors that mediate the impact of HMGCR and APOB on DR risk.
Conclusions:
This Mendelian randomization study suggests that abnormalities in triglyceride (TG) levels serve as a pathogenic element in DR. Of the nine lipid-lowering drug targets assessed, HMGCR and APOB have emerged as potential promising targets for managing NPDR.
Lipid metabolism is pivotal in diabetic retinopathy (DR) development. Nevertheless, the relationship between lipid-lowering drugs and the risk of DR remains controversial. This study utilized Mendelian randomization (MR) to investigate the potential effects of pharmacological targets for lowering lipid levels on DR and to clarify the causal link between blood lipid characteristics and DR.
Material and methods:
The data comprised genetic variations related to lipid traits and genetic variations associated with lipid-lowering drug targets obtained from the Global Lipid Consortium. Total DR, non-proliferative DR (NPDR), and proliferative DR (PDR) were sourced from the Finnish R9 database. Lipid-lowering drug targets were tested using inverse variance-weighted MR (IVW-MR) and statistics-based MR (SMR). Colocalization and mediation analysis were conducted to validate the results and explore potential mediating factors.
Results:
Results: A reduced risk of total DR and NPDR was linked to genetically improved 3-hydroxy-3-methylglutaryl-CoA reductase (HMGCR) (OR = 0.62; 95% CI: 0.46–0.83; p = 1.30× 10^-2; OR = 0.49; 95% CI :0.34–0.70; p = 9.70× 10^-4). Strong colocalization (PP.H4 = 0.85) was observed between whole blood tissue HMGCR expression and a significant MR relationship with total DR (OR = 0.66; 95% CI: 0.52–0.85; p = 7.31× 10^-4). Furthermore, Body mass index (BMI)and glycated hemoglobin (HbA1c) are critical factors that mediate the impact of HMGCR and APOB on DR risk.
Conclusions:
This Mendelian randomization study suggests that abnormalities in triglyceride (TG) levels serve as a pathogenic element in DR. Of the nine lipid-lowering drug targets assessed, HMGCR and APOB have emerged as potential promising targets for managing NPDR.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.