Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
DERMATOLOGY / EXPERIMENTAL RESEARCH
IL-36γ promotes psoriasis-like features in keratinocytes in an imiquimod-induced murine model of psoriasis
1
Department of Dermatology, State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Science and Peking Union Medical College, Beijing, China
Submission date: 2021-07-01
Final revision date: 2021-12-16
Acceptance date: 2021-12-29
Online publication date: 2022-01-01
Corresponding author
Hong-Zhong Jin
State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Science and Peking Union Medical College, China
State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Science and Peking Union Medical College, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Psoriasis is a recurrent, chronic inflammatory skin disease with complex pathogenesis. The disease imposes a heavy burden on patients. Interleukin (IL)-36γ belongs to the IL-36 family and is predominantly expressed by epithelial cells. IL-36γ is upregulated in psoriasis lesions. However, the effects of IL-36γ in keratinocytes remain unclear.
Material and methods:
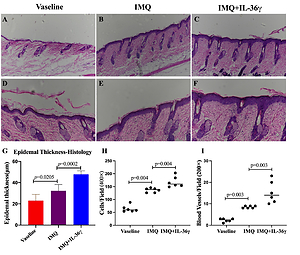
Eighteen IL-36γ-deficient mice were divided into three groups: the vaseline group, the imiquimod (IMQ) group, and the IMQ/IL-36γ group. Vaseline or IMQ was administered for 6 consecutive days. The severity of psoriasis-like lesions was evaluated using a modified Psoriasis Area and Severity Index (PASI) scoring system. Production of cytokines and expression of differentiation markers were assessed by immunohistochemistry.
Results:
IMQ-induced psoriasis lesions were significantly more severe in IMQ/IL-36γ-treated mice compared with vaseline-treated and IMQ-treated mice, as shown by an exacerbated inflammatory phenotype, increased numbers of blood vessels, increased infiltration of cells, and increased epidermal thickness. Expression of loricrin and keratin 5 in skin lesions was decreased following treatment with IL-36γ. Levels of IL-17A, interferon-γ, β-catenin and Dickkopf-related protein 1 were elevated in keratinocytes within psoriatic lesions following IL-36γ stimulation.
Conclusions:
Together, these data showed that IL-36γ contribute to abnormal keratinocytes proliferation and keratinocyte-related proinflammatory cytokines, and suggest that IL-36γ may play an important role in the pathogenesis of psoriasis.
Psoriasis is a recurrent, chronic inflammatory skin disease with complex pathogenesis. The disease imposes a heavy burden on patients. Interleukin (IL)-36γ belongs to the IL-36 family and is predominantly expressed by epithelial cells. IL-36γ is upregulated in psoriasis lesions. However, the effects of IL-36γ in keratinocytes remain unclear.
Material and methods:
Eighteen IL-36γ-deficient mice were divided into three groups: the vaseline group, the imiquimod (IMQ) group, and the IMQ/IL-36γ group. Vaseline or IMQ was administered for 6 consecutive days. The severity of psoriasis-like lesions was evaluated using a modified Psoriasis Area and Severity Index (PASI) scoring system. Production of cytokines and expression of differentiation markers were assessed by immunohistochemistry.
Results:
IMQ-induced psoriasis lesions were significantly more severe in IMQ/IL-36γ-treated mice compared with vaseline-treated and IMQ-treated mice, as shown by an exacerbated inflammatory phenotype, increased numbers of blood vessels, increased infiltration of cells, and increased epidermal thickness. Expression of loricrin and keratin 5 in skin lesions was decreased following treatment with IL-36γ. Levels of IL-17A, interferon-γ, β-catenin and Dickkopf-related protein 1 were elevated in keratinocytes within psoriatic lesions following IL-36γ stimulation.
Conclusions:
Together, these data showed that IL-36γ contribute to abnormal keratinocytes proliferation and keratinocyte-related proinflammatory cytokines, and suggest that IL-36γ may play an important role in the pathogenesis of psoriasis.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.