Introduction
The worldwide prevalence of rheumatoid arthritis (RA), a chronic autoimmune inflammatory illness mostly affecting the joints, is estimated to be between 0.24% and 1.00% in the general population [1, 2]. One of RA’s primary clinical manifestations is symmetrical polyarthritis, characterized by pain, swelling, and stiffness, and the persistent inflammation of RA causes joint damage, deformity, bone destruction, and even severe disability [3]. RA may also affect important internal organs, such as the lungs, heart, nervous system, and respiratory system, leading to life-threatening complications [4]. The main complaint of patients with RA is continual or recurring pain [5], and approximately 75% of RA-related costs are caused by loss of work efficiency [6]. In addition, RA cost estimates are highly uncertain and frequently change substantially, such as estimates of the costs of direct medical care and functional disability that prevents people from working [5]. Therefore, RA has severe adverse effects on people’s health and income, and substantial healthcare resources are required to support and treat people with RA.
The prevalence of RA increases with age, and the occurrence of seropositive RA in adolescents and adults is highly correlated with increasing age of onset. RA significantly increases the occurrence of cerebrovascular illness, ischemic stroke, and coronary artery disease in young people. In addition, 90% of individuals can avoid joint deterioration with early RA diagnosis and therapy [4]. Clinical symptoms in patients treated early are significantly different from those in undertreated patients. Compared with patients who develop RA at an older age, patients who develop RA at a young age usually tend to have a better prognosis in terms of function or disease course [7]. However, there have been significantly fewer studies of young people with early-onset RA than of older people with RA, which underscores the need to determine the global burden of RA – that is, the disability-adjusted life years (DALYs) due to RA – in young adults, i.e., those aged 15–49.
The calculated global burden of RA varies with data sources, age and sex distributions of study groups, classification criteria, and statistical methods and sample size. For example, in 2014, Cross et al. [8] reported the first global burden of RA determined based on a Global Burden of Disease Study (GBD), i.e., GBD 2010. Subsequently, Safiri et al. [9] reported the global burden of RA based on GBD 2017. As GBD is continually updated and expanded, an updated estimate of the burden of RA is required. Accordingly, this study determined incidence of and DALYs due to RA in young adults based on GBD 2019 data, with the aim of clarifying and forecasting long-term trends in the global burden of RA in young adults at regional and country levels to provide evidence for policymakers.
Material and methods
GBD overview
The GBD is organized and conducted by the Institute for Health Metrics and Evaluation [10]. Compared with GBD 2017, GBD 2019 encompassed nine additional nations and territories [10] and thus collected data on 369 kinds of illnesses and injuries and 87 kinds of risk factor burden among 204 countries and areas, seven super regions, and 21 areas from 1990 to 2019. Consequently, GBD 2019 is the most comprehensive and detailed GBD to date, and its results are publicly available at: https://vizhub.hcalthdata.org/gbd/results. A detailed description of GBD 2019 data collection and processing, and an overview of the methodology used to generate the results, have been published [10, 11]. Furthermore, comprehensive details on both fatal and non-fatal approximations may be found at http://ghdx.healthdata.org/ghd-results-tool. Since the study’s foundation is a publicly accessible database, ethical clearance is not necessary.
The SDI is a composite statistic that evaluates a nation’s degree of development by taking into account its overall fertility rate, average educational attainment for those over 15, and lag distributed income (LDI) per capita [10]. Five categories were created based on the SDIs of the countries: low, low-middle, middle, high-middle, and high.
Case definition
The symptoms of RA, a systemic autoimmune condition, may include joint pain, swelling, and deformity in addition to systemic symptoms. International Classification of Diseases (ICD)-9 codes 714.0–714.9 and ICD-10 codes M05, M06, and M08 serve as the foundation for the case definitions of RA in the GBD [10].
Compilation of results
The total number of years of life lost as a result of disease-related impairment and premature mortality is known as the DALYs. The effects of age structures were eliminated by standardizing all GBD 2019 results concerning the world population and reported per 100,000 population, where the standard population was the unweighted average of the distribution of a specific age proportion in 2019 in all populations equal to or greater than 5 million. The age-standardized incidence rate (ASIR) is the sum of the products of a specific age ratio. The 95% uncertainty interval (UI) for each assessment was determined using a Bayesian meta-regression tool, Dis-Mod-MR2.1, based on the 25th and 975th numerical calculations of 1000 ordered draws.
The estimated annual percentage changes (EAPCs) of the ASIR of and DALYs caused by RA were calculated to ascertain the long-term trends in these variables. A fitting model was then used to calculate the appropriate 95% confidence intervals (CIs). In addition, the socio-demographic index (SDI) was used, as it is a comprehensive universal measure for assessing sustainability and health in a region on a scale from 0 to 1. This allowed a locally weighted scatterplot and a smooth regression and trend line to be employed to characterize the relationship between ASIR, its EAPC, and SDIs. All statistics were calculated using R software (4.2.1), and data were visualized using the RColorBrewer, Biocmanager, circlize, and ggplot2 software packages.
Results
Global distribution and change trends of RA in young adults
Globally, in 2019, the ASIR of and age-standardized DALY rates due to RA in young adults were 12.02 and 22.76 per 100,000, respectively. Compared with 1990, this represents an increase of 0.8% and 0.7%, respectively. Globally, from 1990 to 2019, the ASIR (EAPC = 0.31) of and age-standardized DALY rate (EAPC = 0.17) due to RA in young adults per 100,000 population showed a positive trend (Table I, Figure 1, Supplementary Figure S1).
Table I
Age-standardized incidence rate (ASIR) and age-standardized DALY rate of rheumatoid arthritis by location for 15 to 49 years, both sexes, in 1990 and 2019, and its temporal trends from 1990 to 2019
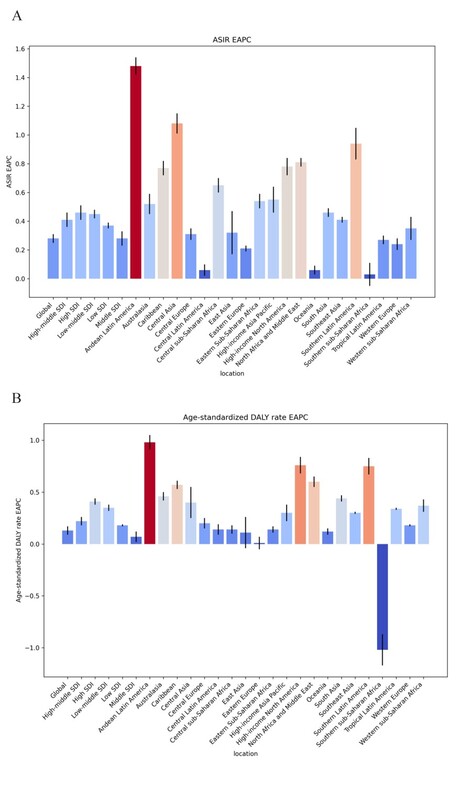
Figure 1
EAPC of the age-standardized incidence rate (ASIR) and age-standardized DALY rate of rheumatoid arthritis for the world, 21 regions and different SDI sub-regions from 1990 to 2019: A – age-standardized incidence rate; B – age-standardized DALY rate

In 2019 and in terms of sex, the incidence of and DALYs due to RA were higher in youthful adult females than in youthful adult males in the five SDI regions and the 21 geographical regions. The prevalence of RA in young adults rose significantly in all five SDI regions and in most geographic regions, with the number of DALYs due to RA increasing slightly more in young adult men than in young adult women worldwide, and in high-SDI and high-middle-SDI regions than in other SDI regions (Figure 2, Supplementary Figure S2).
Figure 2
Time trends for incidence rate, and number of DALYs of rheumatoid arthritis by region from 1990 to 2019 – both genders: A – incidence rate; B – number of DALYs

Young adults were divided into seven groups by age, namely 15–19-, 20–24-, 25–29-, 30–34-, 35–39-, 40–44-, and 45–49-year age groups, and an age-group heat map was constructed depicting the incidence of RA. This revealed that it was similar across all age groups. However, the DALY rate due to RA showed a positive trend with increasing age and was higher among young adults aged 35–49 and older than among adolescents (Figure 2, Supplementary Figure S3, Supplementary Tables SI–SIV).
Distribution and change trends of RA in young adults by SDI region
Table I and Supplementary Figure S1 show that in 2019, the ASIR of and age-standardized DALY rate due to RA in young adults per 100,000 population in the five SDI regions were highest in the high-SDI region (14.33 and 27.28, respectively), followed by the high-middle-SDI region, whereas they were lowest in the low-SDI region (9.32and 16.51, respectively). Table I and Figure 1 show that from 1990 to 2019, the ASIR of and age-standardized DALY rates due to RA in young adults showed a consistent positive trend in the five SDI regions and increased the most in the low-middle SDI region (EAPC = 0.52 and EAPC = 0.43, respectively) and the least in the middle-SDI region (EAPC = 0.35 and EAPC = 0.15, respectively).
Distribution and change trends of RA in young adults by geographical region
In 2019 and among the 21 geographical regions, the ASIRs of RA in young adults per 100,000 population were highest in Southern sub-Saharan Africa (23.07), Central Latin America (21.9) and Central Asia (21.37), and lowest in Western sub-Saharan Africa (3.69), Oceania (5.71), and Southeast Asia (6.69). From 1990 to 2019 and among the 21 geographical regions, the ASIR of RA in young adults per 100,000 population increased the most in Andean Latin America (EAPC = 1.45), Central Asia (EAPC = 1.03), and Southern Latin America (EAPC = 0.94) and decreased the most in Southern sub-Saharan Africa (EAPC = –0.06), Oceania (EAPC = 0.09), and Central Latin America (EAPC = 0.09) (Table I; Supplementary Table SV; Figures 1 A and 3 A; Supplementary Figures S1 A, S3 A, S4 A, S5 A, S6 A, S7 A, and S8 A).
Figure 3
Age-standardized incidence rate (ASIR) and age-standardized DALY rate of rheumatoid arthritis in the world from 1990 to 2019: A – age-standardized incidence rate; B – age-standardized DALY rate
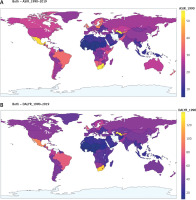
In 2019, out of the 21 geographic regions worldwide, the age-standardized DALY rates due to RA in young adults per 100,000 population were highest in Central Latin America (44.50), Tropical Latin America (44.35), and Central Asia (41.20) and lowest in Western sub-Saharan Africa (7.00), Oceania (12.97), and Southeast Asia (13.52). From 1990 to 2019, the age-standardized DALY rates due to RA in young adults per 100,000 population increased the most in Andean Latin America (EAPC = 0.97),Southern Latin America (EAPC = 0.76) and High-income North America (EAPC = 0.75), and decreased the most in Southern sub-Saharan Africa (EAPC = –1.02) (Table I; Supplementary Table SV; Figures 1 B and 3 B; Supplementary Figures S1 B, S3 B, S4 B, S5 B, S6 B, S7 B, and S8 B).
Distribution and change trends of RA in young adults by country
In 2019 and out of 204 nations and areas, the ASIRs of RA in young adults per 100,000 population were highest in Uzbekistan (33.02), Honduras (30.03), and South Africa (26.34) and lowest in Chad (3.42), Niger (3.53) and Sierra Leone (3.59). From 1990 to 2019, the ASIRs of RA in young adults per 100,000 population increased the most in Equatorial Guinea (EAPC = 1.77), Peru (EAPC = 1.61), and Bhutan (EAPC = 1.48) and decreased the most in Democratic People’s Republic of Korea (EAPC = –0.50), Mexico (EAPC = –0.45) and Zimbabwe (EAPC = –0.26) (Supplementary Tables SI and SVI; Figures 1 A and 3 A; Supplementary Figures S1 A, S3 A, S4 A, S5 A, S6 A, S7 A, and S8 A).
In 2019, the age-standardized DALY rates due to RA in young adults per 100,000 population were highest in Uzbekistan (65.72), Honduras (55.86), and Mexico (49.15) and lowest in Chad (6.60), Niger (6.69), and Sierra Leone (6.83). From 1990 to 2019, the age-standardized DALY rate due to RA in young adults per 100,000 population increased the most in Paraguay (EAPC = 1.62), Guatemala (EAPC = 1.31) and Greenland (EAPC = 1.25), and decreased the most in South Africa (EAPC = –1.30), Estonia (EAPC = –0.62) and Uzbekistan (EAPC = –0.51) (Supplementary Tables SII and SVI; Figures 1 B and 3 B; Supplementary Figures S1 B, S3 B, S4 B, S5 B, S6 B, S7 B, and S8 B).
Relationship between the ASIR and age-standardized DALY rate of RA in young adults and SDI region
Supplementary Figure S9 A shows that there was a nonlinear relationship between the ASIR of RA and SDI region. Specifically, in regions with an SDI of less than 0.7, there was first a positive relationship and then a negative relationship between SDI and the ASIR of RA as the SDI increased, similar to an inverted U shape. In regions with an SDI of 0.7, the ASIR of RA was at a minimum, but in regions with an SDI greater than 0.7, the ASIR of RA increased as the SDI increased. In some regions, such as Southern sub-Saharan Africa, Central Asia, Central Latin America, and Tropical Latin America, the ASIRs of RA were higher than expected. In addition, there was a similar relationship between the age-standardized DALY rate due to RA and SDIs (Supplementary Figure S9 C).
Among the 21 geographical regions, the SDI and the EAPC in the ASIR of RA did not show a significant correlation, which was highest in the region with an SDI of approximately 0.78. In regions with an SDI greater than 0.55 or less than 0.78, the SDI and the EAPC in the ASIR of RA exhibited a favorable association, as the latter increased as the former increased. In regions with an SDI greater than 0.78, the SDI and the EAPC in the ASIR of RA had a negative connection, as the latter decreased as the former increased. However, the increases in the EAPC in the ASIR of RA in Andean Latin America, Southern Latin America, Central Asia, and other regions were much larger than expected (Supplementary Figure S9 B).
Among the 21 geographical areas, the SDI and the EAPC in the age-standardized DALY rate due to RA in young adults decreased overall, but with some variations. Specifically, in regions where the SDI was less than 0.65 or greater than 0.79, SDI and the EAPC in the age-standardized DALY rate had a negative connection due to RA in young adults, as the latter decreased as the former increased. In contrast, in regions where the SDI was greater than 0.65 or less than 0.70, SDI and the EAPC in the age-standardized DALY rate exhibited a favorable association due to RA in young adults, as the latter increased as the former increased. However, the EAPCs in the age-standardized DALY rates due to RA in young adults in Andean Latin America, Southern Latin America, and High-income North America were much larger than expected (Supplementary Figure S9 D).
Discussion
This study analyzed GBD 2019 data to determine the burden of RA in young adults in 21 regions and 204 nations and areas from 1990 to 2019 and the change trends in this burden. The results showed that in this period, the number of cases of RA and the absolute number of DALYs due to RA increased globally, and the ASIR of and age-standardized DALY rate due to RA showed a positive trend, which may be attributable to population growth, improved diagnostic methods and healthcare outcomes, and increased patient survival [12]. In addition, it may be attributable to the facts that GBD 2019 was more comprehensive than previous GBDs and that increased life expectancy has increased the incidence of RA. Cross-regional comparisons revealed that the predominance of RA in young adult women and the incidence of RA overall are increasing in high-SDI regions. In addition, there was clear variation in the burden of RA by geographic region; compared with other regions, low- and lower-middle-income regions such as Tropical Latin America, Central Latin America, Oceania, and Central Asia have a higher burden of RA, and thus patients, families, and societies in these regions are exposed to higher economic costs associated with RA.
RA is a long-term joint condition that primarily affects women and is classified into seropositive and seronegative subtypes. Multiple genetic, environmental, and lifestyle factors are linked to an increased (or reduced) risk of RA, though genetic factors are thought to account for only approximately 40% of cases of seropositive RA and approximately 20% of cases of seronegative RA [13]. Tobacco is an environmental factor that has been extensively studied and is a confirmed risk factor for RA [14]. In addition, multiple studies have consistently demonstrated that occupational silica/dust exposure increases the risk of RA, especially seropositive RA [15], which accounts for the increased risk of RA in low-income areas with high levels of pollution [16]. In a prospective US study, an overall healthy diet was linked to a decreased risk of seropositive RA [17]. This diet was low in animal fats and sugars, reasonably high in fish and omega-3 fatty acids, and high in fruits, grains, and vegetables. A high body-mass index is a risk factor for RA in both men and women [18], and mucosal surface microorganisms (e.g., oral, lung, and intestinal microorganisms), especially bacteria, are significant in the early pathogenesis of RA [19], although the mechanisms of their role remain under study. The top-five factors that directly or indirectly increase the risk of RA in young adults are a poor diet, an unsafe work environment, smoking, hypertension, and a high body mass index [20].
Approximately two thirds of RA patients are female, which may be due to sex hormones and genetic background. Female-specific factors include polycystic ovary syndrome, concentrations of hormones (such as prolactin) [21], early menopause [22], menarche, and breastfeeding. Differences between men’s and women’s access to treatment were also hypothesized as explanations for the predominance of RA in women [23]. However, from 1990 to 2019, the ASIR of and age-standardized DALY rate due to RA were greater in young adult males than in young adult females, which may be linked to smoking, occupational exposure to dust, a poor diet (i.e., high in fat, salt, and sugar), oral bacteria, and obesity [24]. Although the prevalence of RA rises with age in the West [25], the current research of young individuals (i.e., those aged 15–49) found no significant difference in the age of RA onset. However, the DALY rate due to RA generally rose with age, which is attributable to the increased risk of exposure over time to external environmental factors that can cause RA, such as decreased oral hygiene and nutritional status, occupational pollution, and smoking.
RA has a significantly adverse impact on physical functioning, as it can cause fatigue, together with wear, fracture, and functional degradation of joints. In addition, compared to those without RA, those with RA have a significantly increased risk of cardiovascular, gastrointestinal, respiratory, infectious, and hematological diseases. Thus, RA not only lowers quality of life and functional status but also drastically shortens life expectancy and increases the risk of early death.
Our analysis of GBD 2019 data suggests that the relationship between RA burden and SDI is complex and non-linear. However, it appears to be clear that living in poverty and lacking health insurance coverage are linked to an increased risk of RA. The apparent differences in RA burdens between SDI regions also offer some possible guidelines for the allocation of health resources. Moreover, low-SDI regions such as Tropical Latin America, Central Latin America, and Central Asia have a high RA burden due to various factors. For example, some genes in native Latin Americans are significantly associated with RA at the individual and population levels [26], and Latin America is experiencing an increase in childhood obesity [27] and rapid economic development, with the latter increasing the risk of RA due to exposure to pollutants. This may account for the high incidence of RA in low socioeconomic areas [28]. Similarly, the prevalence and severity of RA are increasing in sub-Saharan Africa and Oceania, where the burden of RA has been underestimated and the allocation of health resources is a low priority [29], and the most effective biologic drugs for RA are far beyond people’s financial means [30]. Thus, most patients with RA in these regions are treated with ineffective or unproven drugs. Moreover, these regions have an insufficient number of rheumatologists and rheumatology nurses to diagnose and treat various rheumatic diseases [31], resulting in disability and/or premature death of patients. Thus, the problems of poor drug availability, poor healthcare conditions, patient distrust, insufficient numbers of specialists, and misdiagnosis of RA in low-income areas must be solved, and there is an urgent need to identify the RA burden and implement cost-effective treatments and health services in these areas.
We also found that there have been significant increases in the ASIR of and age-standardized DALY rates due to RA in high-SDI regions, such as High-income North America, illustrating the advantages of improving case identification and access to care in multiple healthcare settings, such as rheumatology clinics, emergency departments, and inpatient facilities. However, although diagnosis and treatment can achieve so-called remission, 27–50% of patients experience clinical levels of social dysfunction, mental distress, pain, and fatigue after 5 years [32], and RA comorbidities are often linked to an increased risk of infection, cancer, and cardiovascular disease [33] and may shorten life expectancy. Moreover, there are considerable inequalities in access to RA treatment at the national and international regional levels, which may be attributable to differences in socioeconomic conditions, disease management, and access to specialized care.
The growth in the ASIR of RA in youthful adults in the countries Uzbekistan, Mexico, Paraguay, and Honduras may be attributable to their populations’ similarities in terms of the prevalence of smoking, insufficient exercise, obesity, metabolic syndrome, and malnutrition. There may also be country-specific RA characteristics. For example, in Uzbekistan, some climatic conditions (wet, high temperature, and cloudy conditions) and geographical factors (such as soil quality) influence the activity level and clinical form of RA. In addition, factors related to patient behavior and referral systems lead to delayed diagnosis and treatment of RA. Mexico, Paraguay, and Honduras are countries in the rapidly developing regions of Latin America and the Caribbean, where individual-level factors (e.g., early infection, sanitary conditions, and hormone therapy) and environmental factors (associated with, for example, industrialization, demographic transition, and urbanization) may combine to increase the prevalence of RA. This highlights the potential influence of cultural and socioeconomic factors on the etiology of RA [34]. Therefore, lifestyle-specific prevention and health-promoting response strategies could help reduce the burden of RA.
Based on data from GBD 2019, this study produced the most complete and current statistics on the prevalence of RA in young people worldwide from 1990 to 2019. It also analyzed this burden and its change trends in different countries and regions to provide policy-makers with targeted strategies for RA prevention, diagnosis, and treatment. However, this study had three limitations, as follows. (1) The fatal and non-fatal RA outcome data in GBD 2019 did not completely describe RA and its different stages of development, and therefore the burden of RA could not be analyzed in terms of disease course and severity. (2) Although an increasing number of RA-related risk factors have been recognized, a causative link has been established only between smoking and RA, meaning that it is difficult to identify and distinguish risk factors in a specific region and country. (3) The study group was aged 15–49 and thus not all age groups were examined, meaning that this was not a comprehensive assessment of the global burden of RA in people of all ages.
In conclusion, the ASIRs of and age-standardized DALY rates due to RA in young adults worldwide showed a positive trend from 1990 to 2019, and the risk of RA was higher in young adult women than in young adult men. In addition, these parameters remained high and increased significantly in high-SDI regions. Nevertheless, the burden of RA in low-income countries of sub-Saharan Africa, Latin America, Oceania, and Central Asia is substantial, especially in Uzbekistan, Mexico, Qatar, and Paraguay. Awareness of RA, elimination of its risk factors, and early treatment are key to reducing the burden of RA in young adults and other patients.