Lung resection is a surgical procedure indicated in patients with lung tumors or, sometimes, with non-malignant lung diseases [1]. The most common type of lung cancer is non-small cell lung cancer, where surgical resection is the primary mode of treatment in the early stages [2]. Prognosis and length of survival (including the 5-year survival rate) vary according to the type of cancer. Regardless of such variation, lung resection is a significant factor in increasing survival, especially in the case of severe types of cancer [3–5]. The surgery may, however, lead to a deterioration in the patient’s functional status. This deterioration can typically be objectified by measurement of lung function, i.e. spirometry, which is part of the preoperative examinations [6]. These parameters are, however, not always measured in post-operative follow-up examinations.
Lung cancer is the second most prevalent cancer and it is a leading cause of cancer death worldwide [7]. In the Czech Republic, lung cancer ranks third in cancer incidence but in absolute first place in terms of cancer mortality [8]. There are 8 highly specialized thoracic surgery cancer centers in the Czech Republic, including University Hospital Ostrava, where most lung cancer patients are treated. Early diagnosis of lung cancer has a major impact on the patient’s prognosis. In the Czech Republic, more than 70% of lung tumors are detected in clinical stage IV or III [9]. Because of this late detection, the prognosis of lung cancer is unfavorable, and the 5-year survival in patients with lung cancer is quite low: 9.4–14% according to Ulusan et al. [10] In the Czech Republic, the 5-year survival rate has increased from 9.6% to 19.3% over the last 20 years. That is why the Czech Republic introduced a lung cancer screening program [8].
Tobacco smoking (both past and current) is considered one of the most significant risk factors for developing lung cancer. Other risk factors include environmental and occupational exposures such as air pollution, asbestos exposure, ionizing radiation, and radon; and family history. These factors are significant in industrially burdened regions, which include the Moravian-Silesian Region [11, 12]. Workers in high-risk professions are subject to regular occupational health examinations, utilizing, however, only basic examination methods [13].
This prospective study aimed to evaluate the functional lung condition defined by spirometry and whole-body plethysmography parameters and other risk factors for lung cancer in patients undergoing lung resection for suspected lung cancer, and assess these factors in relation to the established lung cancer screening criteria in the Czech Republic, as well as to assess the development of lung functions in the post-surgical period.
Methods
Study group
The study group consisted of patients referred for lung resection due to a suspected pulmonary malignancy at the University Hospital Ostrava in the period of 5/2021–12/2022. Additional inclusion criteria were patient consent, age 18+, good usage of the Czech language, and orientation to time and place.
In all, 74 patients entered the study. Some patients, however, opted out of the surgery or decided to exit the study. Fifty-four patients underwent the first examination and subsequent surgery but the compliance in attending the follow-ups was problematic. From the original group, 20 patients decided not to undergo surgery. Of the remaining 54, unfortunately, not all of them came to the planned check-ups according to the study protocol, e.g. due to distance, post-operative complications, etc. Only 45 people came for the pre-operative examination, only 48 patients at hospital discharge, 48 patients 3 weeks after surgery, and 37 patients 3 months after surgery. A significant proportion of the patients did not come at least once; therefore there remained only 24 patients who completed all examinations.
Research methods and data collection
All patients scheduled for lung resection at the University Hospital due to suspected lung cancer were approached to enter the study. Functional status was evaluated by spirometry and whole-body plethysmography before the surgery, on discharge (i.e., approximately on day 8 after the surgery), 3 weeks, and 3 months after the surgery. Spirometric parameters included forced vital capacity (FVC), vital capacity (VC), forced expiratory volume at 1 s (FEV1), and the FEV1/FVC ratio; total lung capacity (TLC) was measured by whole-body plethysmography. All parameters are presented as % of predicted based on age, height, weight and sex of the individual patient. Both spirometry and plethysmography were performed at the same department of the University Hospital Ostrava according to the ATS/ERS guidelines [14].
Demographic data, family, and personal history with an emphasis on risk factors were acquired through questionnaires.
Results
Study group description
The mean age of the patients in the final cohort was 65.2 ±9.1 years (min. 37, max. 79), with a slight predominance of women (54.2%) over men (45.8%). Adenocarcinoma (37.5%) and squamous cell carcinoma (16.7%) were the most common histological findings. Family history of lung cancer was reported by 29.2% of patients. Current smoking was reported by 25% of patients, with an average of 11 ±6 cigarettes per day. In all, 29.2% were ex-smokers, having smoked an average of 13 ±6 cigarettes/day for 33 years. Regular exposure to passive smoking was reported by 21.6% of patients. History of occupational exposure was reported by 20.8% of patients, all of whom had worked in coal mines. All details of the cohort are shown in Table I.
Table I
Description of the patients undergoing lung resection including risk factors for lung disease (n = 24)
Function assessment
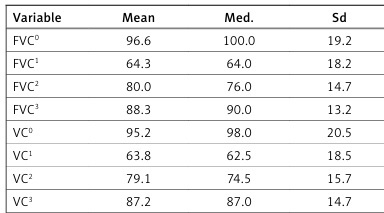
Results of pulmonary function assessment by spirometry and whole-body plethysmography are presented in Table II. The average results of the preoperative spirometry and plethysmography examination are within the norms. Both FVC and VC were lower than the predictive value (i.e. 80%) in only 5 patients. The FEV1 indicator was below the norm in only 8 patients. Compared to the preoperative examination, all mean and median values of each parameter (except the FEV1/FVC ratio) significantly deteriorated after the surgery. The most significant decline was recorded in FVC, which dropped from a mean preoperative value of 96.6% to 64.3% (p < 0.001). A gradual improvement in this parameter to 80.0% and 88.3% was observed at subsequent examinations, but the values still remained statistically significantly worse than preoperatively.
Table II
Functional status of the patients undergoing lung resection (n = 24)
| Variable | Mean | Med. | Sd | Min. | Max. | P-value* |
|---|---|---|---|---|---|---|
| FVC0 | 96.6 | 100.0 | 19.2 | 67 | 139 | |
| FVC1 | 64.3 | 64.0 | 18.2 | 23 | 102 | < 0.001x |
| FVC2 | 80.0 | 76.0 | 14.7 | 48 | 108 | < 0.001x |
| FVC3 | 88.3 | 90.0 | 13.2 | 62 | 108 | 0.001x |
| VC0 | 95.2 | 98.0 | 20.5 | 64 | 144 | |
| VC1 | 63.8 | 62.5 | 18.5 | 22 | 102 | < 0.001x |
| VC2 | 79.1 | 74.5 | 15.7 | 46 | 108 | < 0.001x |
| VC3 | 87.2 | 87.0 | 14.7 | 60 | 110 | 0.001x |
| FEV10 | 90.9 | 92.0 | 16.9 | 59 | 126 | |
| FEV11 | 61.4 | 64.0 | 13.1 | 26 | 81 | < 0.001x |
| FEV12 | 74.4 | 73.0 | 13.0 | 47 | 97 | < 0.001x |
| FEV13 | 80.7 | 81.0 | 11.8 | 59 | 109 | < 0.001x |
| FEV1/FVC0 | 77.4 | 78.7 | 7.9 | 62.1 | 88.7 | |
| FEV1/FVC1 | 79.8 | 80.7 | 10.0 | 58.3 | 93.9 | 0.016x |
| FEV1/FVC2 | 75.9 | 77.6 | 9.4 | 59.1 | 90.5 | 0.869x |
| FEV1/FVC3 | 74.8 | 75.7 | 9.1 | 57.4 | 90.7 | 0.111x |
| TLC0 | 91.8 | 89.0 | 21.0 | 51 | 135 | |
| TLC1 | 70.9 | 69.0 | 17.4 | 32 | 104 | < 0.001x |
| TLC2 | 75.3 | 76.0 | 17.6 | 40 | 107 | < 0.001x |
| TLC3 | 81.5 | 80.0 | 18.5 | 43 | 113 | 0.001x |
A similar course was observed in VC, which decreased from 95.2% to 63.8% (p < 0.001) postoperatively, and in plethysmography (TLC), decreasing from a preoperative value of 91.8% to 70.9% on discharge (p < 0.001). Subsequent follow-up examinations saw gradual improvement in the pulmonary function parameters VC, FVC, FEV1, and TLC, with a tendency to match the original results.
Discussion
Lung cancer is a serious and potentially lethal diagnosis. The treatment includes surgery – resection of the affected part of the lung. Lung resection interferes with the patient’s life as it can lead to a significant deterioration in functional status.
In 2022, a screening program for early detection of lung cancer was introduced in the Czech Republic. The target population of the program consists of smokers (current and ex-smokers) aged 55–74 years with at least 20 pack-years or the equivalent [15]. No other risk factors are taken into account. In our study, approximately 30% of patients had a family history, 20% were passive smokers and 20% had a history of occupational exposure (and 35.2% in the original sample of all 54 patients who underwent the surgery in the biggest center covering a region with a population of about 1.2 million). We believe that failing to take into account these factors, especially occupational exposure, in a screening program may represent an important omission, and that they should be considered in the inclusion criteria for the screening program.
The likelihood of detecting lung cancer during occupational examinations at an early stage is low anyway [16], as during occupational health examinations, only spirometry and chest X-ray are performed (unlike during the screening program using low-dose CT – LDCT – with higher sensitivity). In our study, one fifth of the patients were former coal miners. A large cohort of 3476 miners from our region was previously studied, where a third of the patients were non-smokers [17]. We can, therefore, ask whether the exclusion of non-smoking individuals with occupational hazard is reasonable as a randomized controlled trial proved a decreased mortality rate when LDCT lung cancer screening was performed compared to a simple chest X-ray [18] by as much as 20%, while another trial comparing LDCT vs. no screening revealed a difference of 24% [19]. These data suggest that X-ray screening might be ineffective, which was also concluded by Thomas and Tanner [20]. This does not necessarily mean that X-ray has no place in occupational health examinations, as it can detect other diseases such as pneumoconiosis [21]. This suggests that based on a rough estimate, up to an alarming one-third of high-risk patients (non-smokers with occupational exposure) may be omitted in lung cancer screening.
Considering that according to the 2014–2018 data, 50% of lung tumors were detected only at clinical stage IV and 20% at stage III, which made it the latest diagnosed malignancy of all [15], the introduction of effective screening would be certainly beneficial. Most screening programs around the world also use age and smoking status as inclusion criteria, but, as mentioned, these are not the only risk factors for lung cancer. Establishing appropriate screening criteria would lead to earlier detection of lung carcinomas, which could improve the survival of lung cancer patients [19, 22]. Predictive models that include (in addition to smoking status and age) sex, history of other malignancies, family history of lung cancer including the age of onset, asbestos exposure, and history of pneumonia could help establish such selection criteria and thus improve screening effectiveness [19]. For example, according to Tringali et al., inclusion criteria for screening in the UK also include asbestos exposure, family history of lung cancer at an early age, previous malignancy, and non-cancer respiratory disease (e.g. COPD) [23].
The patients’ functional status was assessed by spirometry. The thresholds of 80% for FVC and FEV1 and 75% (70% in people over 50 years of age) for FEV1/FVC prevails in everyday practice [24, 25]. Spirometry also plays a key role in occupational health examinations. It is worth noting that according to the preoperative spirometry values, these criteria would detect only approximately 20% (based on the results of pre-operative FVC values, which indicate a restriction disorder and therefore may point to the presence of a tumor) of patients in our group and refer them for further examination despite the fact that all of them had confirmed or highly suspected malignancy at the time of the pre-operative spirometry test. Even 3 months after the surgery, when the spirometry results were significantly worse than at the pre-operative spirometry, the mean FVC and FEV1 values were above 80% again (i.e., normal).
The sharp decline in lung function values after surgery is mainly caused by chest wall damage and the resected lung and general anesthesia; a gradual recovery can be, however, observed over time, with an observable improvement at 3 months after the surgery. This has been reported by Ueda et al. [26] and also observed in our patient group. In a longer time horizon of 3–12 months after the surgery, however, the outcomes vary among studies. Ueda et al. described 6 studies, with FVC values at 3–12 months being reduced only by 5.9–18.9% compared to preoperative levels, despite the lobectomy corresponding to a loss of approximately 20% of lung parenchyma [26]. Lobectomy was also the most common surgery in our study group (66.7%), with a mean FVC reduction of 8.3% at 3 months postoperatively compared with the preoperative examination.
In a study by Shin et al. they also found a significant reduction in pulmonary function values in the immediate postoperative period and a subsequent improvement at 6 and 12 months after surgery. A greater decrease in lung function values was noted by Shin et al. in patients who underwent bilobectomy/pneumonectomy versus lobectomy [27], which is logical given the greater extent of resected lung tissue. This is confirmed by a study by Gu et al., who noted a statistically significant difference in lung function values 6 months after surgery according to the type of procedure and the related extent of resected lung tissue in lobectomy vs. segmentectomy vs. wedge resection [28]. Unfortunately, we could not evaluate the difference in surgery in our study because bilobectomy was performed in only 3 patients (and pneumonectomy in none).
The presence of a tumor can cause both obstructive and restrictive ventilatory disorders. A restrictive disorder can be suspected where FVC is reduced, but spirometry as such does not serve as a definitive diagnostic tool for this purpose. According to De Matteis et al., a specificity of 96% and sensitivity of 71% can be achieved using a combined threshold of FVC < 70% and FEV1/FVC ≥ 70% [29]. On the other hand, an obstructive ventilatory disorder can be directly diagnosed based on low FEV1 at spirometry. Wasswa-Kintu considered even a relatively small reduction in FEV1 to be a significant predictor of lung cancer; namely, an FEV1 drop below 90% was associated with a 30% increase in the risk of lung cancer in men and a 164% increase in women [30]. In our study group, this threshold (FEV1 < 90%) was met in 45% of patients.
Impaired lung function is caused by reduced ventilation and oxygen uptake, which further negatively affects bodily functions, physical health, sleep, and psychosocial aspects. These associations were investigated in detail by Wen et al., whose results revealed a statistically significant association between lung function (expressed as FVC and FEV1) and the quality of life, especially in the domain of physical health [31]. Their results are consistent with ours, as we also observed a decrease in the quality of life in the domains evaluating physical health in our previous study [32].
Our study has some limitations, such as the monocentric character of data acquisition and the study group size. On the other hand, the study group comprised a full sample of patients treated in the principal center for thoracic surgery for the entire Moravian-Silesian region over an 18-month period, and the final group size was affected by poor patient compliance, which is outside the powers of the investigators. We could not accurately assess the impact of selection bias because all patients who were scheduled for lung resection surgery due to suspected lung cancer in University Hospital Ostrava (which is one of the 8 highly specialized thoracic surgery cancer centers in the Czech Republic) were approached to participate in the study. Based on long-term statistics, around 50 patients per year are scheduled for lung resection in this hospital. Still, we believe that our study can be a valuable basis for further research in patients undergoing lung resection and provides evidence for broadening the inclusion criteria for the screening program beyond the current sole criterion of smoking to include occupational health and family history.
In conclusion, lung resection significantly affects the lung functions. Despite the gradual improvement, the original values are (unsurprisingly in view of the fact that a part of the lungs has been resected) not achieved over a 3-month period. Lung cancer is often detected at late clinical stages in the Czech Republic, which could be improved by the newly introduced screening approach. However, this screening targets only smokers. This might pose a problem for individuals with a history of occupational exposure, who could also benefit from such screening, as standard occupational health examinations (including only spirometry and chest X-ray) appear to be insufficient for revealing lung cancer.