Introduction
Diabetes is one of the diseases that seriously endanger human health. By 2022, there were about 526 million diabetes patients worldwide and about 124 million diabetes patients in China [1, 2]. Blood glucose monitoring is the basis and an important link of intensive treatment for patients with diabetes. Patients with poor blood glucose control need to have blood glucose monitoring more than 4 times a day [3]. In addition to diabetes patients, severe patients, and postoperative fasting patients also need to monitor blood glucose every day [4]. At present, the clinical blood glucose monitoring methods mainly include capillary blood glucose monitoring (mainly fingertip blood glucose monitoring) and venous blood glucose monitoring. The determination of venous blood glucose value is an internationally recognized gold standard because of its high accuracy [5]. However, due to the shortcomings of complex operation, high blood demand, and long waiting time for results, this process cannot be used as the main means of frequently monitoring blood glucose. The portable blood glucose meter is used to measure blood glucose at the fingertips, which has the advantages of small volume, simple operation, low blood demand, fast collection of results and less trauma [6–8], which is commonly used in hospital and home blood glucose monitoring. Although peripheral blood glucose is the most commonly used method for blood glucose monitoring, there is no unified standard for taking the first drop or the second drop of blood when collecting a blood sample.
In 2010, the Ministry of Health of China stated that the first drop of blood should be abandoned and the second drop of blood glucose should be used to detect blood glucose in the “Code of Management and Clinical Practice of Portable Blood Glucose Tester in Medical Institutions” [9]. To date, a large number of studies at home and abroad have reported that there is no significant difference in the blood glucose value measured by the first two drops of blood. However, some studies have reported that the blood glucose measured by the first two drops of blood is different, so the second drop of blood should be used to detect blood glucose. There are systematic reviews [10–12] to compare and analyze the differences in the effect of blood glucose determination between the first two drops of blood, but there are few reports included in the systematic evaluation, the heterogeneity of instruments and methodologies is not discussed, and the conclusions are not comprehensive. Different opinions and views make clinical workers confused in the implementation of treatment and health education. Therefore, the purpose of this study is to provide useful reference information for clinical blood glucose monitoring and nursing and health education by analyzing the difference of blood glucose detection between the first two drops of capillary blood by meta-analysis.
Material and methods
This meta-analysis and systematic review was conducted and reported based on the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement [13].
Literature criteria
The inclusion criteria of the literature for this meta-analysis were as follows: (1) the population of the study consisted of patients who needed to have their blood glucose monitored; (2) the study was designed as a non-randomized controlled trial matched before and after, and the design of the study was reasonable; (3) the literature reported the value of blood glucose in the first two drops of the fingertips.
The exclusion criteria were as follows: (1) literature with poor quality and repeated reports; (2) reports whose original data were incomplete or unable to be extracted and used; (3) unmatched trials, simple case reports or nursing summaries, reviews.
Literature search
The two authors searched PubMed, ClinicalTrials, Cochrane Library, Clinical Evidence, EMBASE, China National Knowledge Infrastructure (CNKI), Wanfang and Weipu databases. This study searched all the relevant literature about the comparison of blood glucose values of the first capillary blood from the establishment of each database until November 10, 2023. The literature search formula of this study was as follows: (“diabetes mellitus” OR “capillary blood” OR “glucose” OR “blood glucose” OR “blood sugar”) AND (“first drop” OR “second drop” OR “monitoring” OR “blood glucose monitoring” OR “measurement”). In strict accordance with the purpose of the study and the inclusion criteria of the literature, the two researchers independently reviewed the titles and abstracts of the literature to determine whether the literature was included or not. For the literature with different opinions, the third person would intervene to reach an agreement after discussion. For the included literature, the basic information of the literature was extracted and sorted out by two researchers, including the first author, publication time, the general data of patients, such as included population, the number of matched cases, details of blood glucose monitoring and outcomes.
Literature quality assessment
The included literature quality evaluation was completed independently by two researchers, and the evaluation results were cross-reviewed and discussed. If there were any differences, the third researcher was consulted. The methodological index for non-randomized studies (MINORS) tool was used to evaluate the quality of the included studies. There were 12 evaluation indicators in the MINORS tool, each item was evaluated with a score of 0 to 2, and the highest score was 24. A score of 0 indicated that the item was not reported in the literature, a score of 1 indicated reported but insufficient information, and a score of 2 indicated that the literature reported and provided sufficient information. The higher the evaluation score is, the better is the quality of the literature.
Statistical analysis
RevMan 5.4 software was used for meta-analysis in this study. This meta-analysis calculated the mean difference (MD) and its 95% confidence interval (CI) for continuous variable data. The heterogeneity included in the study was analyzed by the χ2 test (the test level was α = 0.1), and the heterogeneity was quantitatively judged by the I2 value. If there was no statistical heterogeneity (I2 < 50%, p > 0.1) among the results of each study, the fixed effect model was used for meta-analysis. If there was statistical heterogeneity (I2 ≥ 50%, p < 0.1) between the results of each study, the source of heterogeneity was further analyzed. After excluding the obvious clinical heterogeneity, a random effect model was used for meta-analysis. The publication bias of the results was analyzed by funnel plot and the Egger regression test. P < 0.05 indicated that there was a significant difference between the two groups.
Results
Study selection
As presented in Figure 1, according to the retrieval strategy, this meta-analysis preliminarily retrieved 166 articles. After preliminary reading of titles and abstracts, 58 articles that met the inclusion criteria were selected. After reading the full text, 23 studies [14–36] were finally included in this meta-analysis.
Characteristics of included studies
As shown in Table I, of the included 23 studies, a total of 3121 patients were included, the included studies reported 6340 cases for first and second drop of capillary blood respectively. The 23 studies included were from China, Turkey, India and Italy. The included studies had established clear inclusion and exclusion criteria, and reported the basic information of each group.
Table I
Characteristics of included studies
Quality of included studies
All the included studies were self-paired non-randomized controlled studies. Items 6, 7 and 8 of the MINORS tool were not reported in each trial, while other items were reported and provided the necessary information. The overall quality of the literature included was good (Table II).
Table II
Quality of included studies
Meta-analysis
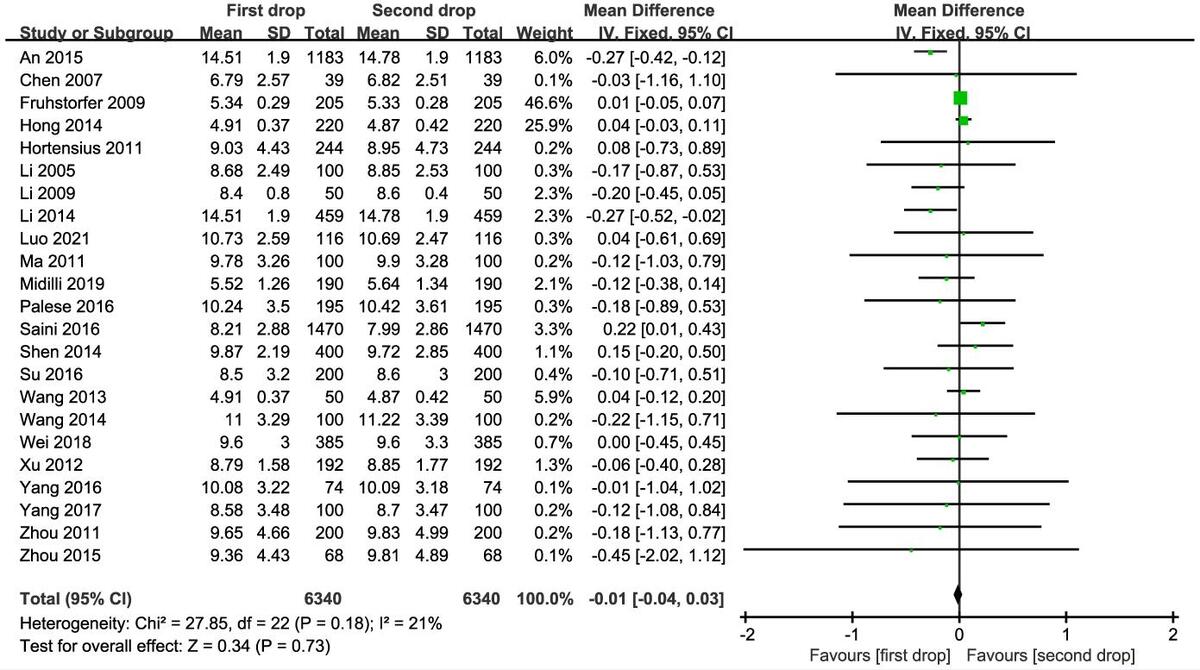
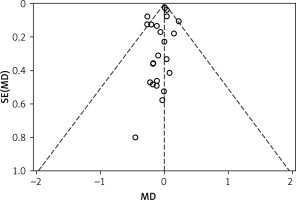
All the included 23 studies reported the blood glucose value of the first versus second drop of capillary blood. As presented in Figure 2, there was no significant difference in the measured value of blood glucose between the first drop and the second drop of capillary blood (MD = –0.01, 95% CI (–0.04, 0.03), p = 0.73). Funnel plot (Figure 3) and Begg’s test results (p = 0.152) showed that there was no publication bias in the synthesized outcome.
Among the 23 studies included, 8 used the glucose oxidase (GOD) method and 8 used the glucose dehydrogenase (GDH) method for the blood glucose meter measurement method, and the other 7 articles concerned other brand blood glucose meters that were not reported and therefore were not included in the analysis. The results of the meta-analysis showed that there was no significant difference in the first two drops of blood glucose between the GOD blood glucose meter and GDH blood glucose meter.
Of the 23 studies included, 13 studies only used 75% ethanol to disinfect fingertips, 6 studies used flowing water to wash hands and then used 75% ethanol to disinfect hands, and 3 studies used hand washing only with flowing water. The subgroup analysis of three different cleaning methods showed that there was no significant difference in the blood glucose value in the first two drops among the hand washing group, disinfection group and hand washing disinfection group (p > 0.05).
Sensitivity analysis
In this study, the results of one of the studies were removed in turn to observe the value of the combined effect of the remaining studies, and the combined effect of each group was within the 95% CI of the total combined effect, and the results did not change significantly, indicating that the results of the analysis were robust and reliable.
Discussion
Blood glucose monitoring provides information about the body’s glucose metabolism, and its accuracy is essential for correct clinical decisions, especially in patients whose insulin dose is determined by blood glucose results [37, 38]. Venous blood glucose is considered to be a reliable monitoring index, but because it takes a long time to check blood glucose levels in hospital laboratories, which may lead to delayed treatment, bedside blood glucose meters are often used to measure blood sugar [39]. At present, the monitoring of blood glucose in the fingertips is a simple, rapid and reliable method. It is observed that in clinical practice, nurses use different methods to collect blood samples for capillary blood glucose determination [40]. There is no standard practice in blood glucose measurement either in the literature or in clinical practice. Therefore, for health care workers and patients who are regularly monitored, it is very important to determine the correct blood glucose measurement technique to avoid inaccurate results. In this study, the blood glucose values measured by the first two drops of blood in 23 reports were analyzed by meta-analysis. The results showed no difference in blood glucose between the first drop and the second drop of blood, suggesting that both of them can be used for the determination of blood glucose.
In the past, many health care providers thought that the first drop of fingertip blood should be abandoned because the first drop of fingertip blood is usually taken from the capillaries of the fingertips, and the blood sample contains interstitial and intracellular fluid, which was a mixture of arterioles, venules and capillaries [41]. When collecting blood samples, excessive squeezing of the fingertips will lead to the mixing of tissue fluid and blood samples, resulting in incorrect measurement results [42]. Also, wiping off the disinfectant after disinfection cannot completely remove the residual disinfectant on the skin surface, and the first drop of peripheral blood is inevitably mixed with a small amount of disinfectant, thus affecting the accuracy of the measured value. Furthermore, the exudation of tissue fluid decreases with time, and the mixed tissue fluid of the second drop of peripheral blood may be lower than that of the first drop of peripheral blood [43]. At present, many nursing experts and educators recommend that patients wash their hands with water and soap and use the first drop of blood [44].
Some studies [45, 46] compare the values of the first drop and the second drop of blood in blood glucose self-monitoring with that of venous blood, and come to the conclusion that there is no difference in blood glucose value between venous blood and the first drop of blood. Under the condition that the patient’s hands are clean, the first drop of blood is closer to the value of venous blood glucose [47, 48]. The first drop of fingertip blood is mostly natural flow, while for the second drop of fingertip blood, if the needle depth is insufficient, often external force needs to be used to force blood outflow, because external force extrusion can cause too much tissue fluid exudation and hemodilution. Hemodilution also causes dilution of other components that need to be tested, resulting in a poor test value [49]. If the needle depth is increased, it will increase the pain of patients, and the wound will also deepen. For patients who need to have blood glucose monitored for a long time, it will increase the resistance of patients and reduce the compliance of regular blood glucose monitoring [50].
At present, the core technology of blood glucose meters mainly includes GOD and GDH. The GOD blood glucose meter has high specificity to glucose and is not disturbed by other glucose, but is easily disturbed by oxygen. The GDH blood glucose meter can easily be disturbed by other glucose, but not easily disturbed by oxygen [51, 52]. Due to the difference in the principle of blood glucose detection between the two blood glucose meters, it may affect the blood glucose value of the first two drops of blood, and then affect the difference [53]. According to the subgroup analysis of different kinds of blood glucose meters, no matter whether a GOD or GDH blood glucose meter, there is no significant difference in the rapid determination of blood glucose by using the first two drops of blood, and the first drop of blood can be used to detect blood glucose directly. Additionally, this study found that irrespective of whether the patient washes the hands or not, the first drop of peripheral blood can still be chosen for blood glucose detection. The results of this study suggest that when using a rapid blood glucose meter to determine the blood glucose value, as long as it is operated correctly, it is not necessary to wipe off the peripheral blood of the first drop, but the first drop of peripheral blood can be used directly to determine the blood glucose value. In the busy nursing work, this can not only save the trouble of wiping off the first drop of blood, and reduce the consumption of disposable medical supplies and blood contamination, but also save more valuable working time, and reduce the patient’s pain. However, it must be noted that the included studies do not report that the difference between the dosage in the first and second drop is also similar among different levels of glycemia, and we cannot calculate it because of the limited data. Therefore, future studies should report more about the dosage in the first and second drop and identify the potential association with the different levels of glycemia.
There are some limitations in this meta-analysis that are worth considering. Firstly, the patients in the included studies have no obvious abnormal peripheral circulation or other special changes in blood glucose, so for patients with other disease types and special conditions, the difference of blood glucose values in the first two drops of the fingertips also needs other studies to supplement the relevant data. In addition, most of the included studies did not report the corresponding venous blood glucose values. This study only compared the blood glucose values of the first two drops of blood, but did not include the venous blood glucose values. In the future, it is necessary to compare the blood glucose values of the first two drops of blood and venous blood glucose values, and analyze which of the first two drops of fingertip blood is closer to the venous blood glucose value, to provide more reliable evidence for clinical blood glucose monitoring and nursing.
In conclusion, the results of the meta-analysis showed no significant difference between the first drop of blood and the second drop of blood in the rapid determination of blood glucose, and it is not necessary to abandon the first drop of blood when measuring peripheral blood glucose. Measuring blood glucose with the first drop of blood not only helps to reduce the time pressure of nurses to detect blood glucose, and reduces the waste of medical resources, but also reduces the inconvenience and pain of patients’ daily diabetes management, which has certain social and economic benefits.