Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
RADIOLOGY / CLINICAL RESEARCH
Fat-free muscle index predicts overall survival in mass-forming intrahepatic cholangiocarcinoma patients:
a sex-stratified analysis
1
Department of Radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, China
2
Department of Neurology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, China
3
Department of Pathology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, China
Submission date: 2023-01-04
Final revision date: 2023-01-26
Acceptance date: 2023-02-07
Online publication date: 2023-02-09
Corresponding author
Yang Yang
Department of Radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, 1095 Jiefang Avenue, Wuhan, Hubei, 430030, P.R.Chi, 430030, Wuhan, China
Department of Radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, 1095 Jiefang Avenue, Wuhan, Hubei, 430030, P.R.Chi, 430030, Wuhan, China
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Sarcopaenia is associated with adverse outcomes in patients with malignancies, and it remains unclear whether the sex discrepancy of sarcopaenia or muscle loss leads to different prognoses in patients with mass-forming intrahepatic cholangiocarcinoma (MICC).
Material and methods:
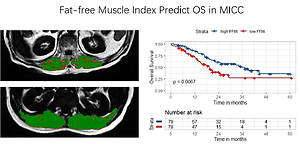
Patients who were pathologically diagnosed with MICC and underwent partial hepatectomy between 2012 and 2019 were recruited. Fat-free muscle areas (FFMA) were defined as areas of bilateral erector spinae muscles on dual-echo, T1-weighted, gradient-recalled-echo images at the level of the radix of the superior mesenteric artery. Fat-free skeletal muscle index (FFMI) was calculated by dividing the FFMA by the individual’s height squared. The prognostic value of FFMI was investigated using the Kaplan-Meier method and multivariable Cox regressions in both the entire cohort and in sex-specific subgroups.
Results:
A total of 157 patients were finally included. Cut-off values for the definition of low FFMI were 14.19 cm2/m2 in males and 11.07 cm2/m2 in females. Patients with low FFMI had significantly shorter overall survival (OS) than those with high FFMI in the entire cohort (19.42 vs. 35.29 months, p = 0.0067) and male patients (17.25 vs. 37.19 months, p = 0.006), but not in females. Multivariate analyses showed that low FFMI was a significant predictor of OS in the entire cohort (HR = 1.725, 95% CI: 1.054–2.821, p = 0.030) and in male patients (HR = 2.145, 95% CI: 1.113–4.133, p = 0.023). No association between FFMI and disease-free survival was found in both the entire cohort and sex-specific subgroups.
Conclusions:
Preoperative FFMI measured by MRI is a prognostic biomarker for OS in MICC patients, and it is more sensitive in males than in females.
Sarcopaenia is associated with adverse outcomes in patients with malignancies, and it remains unclear whether the sex discrepancy of sarcopaenia or muscle loss leads to different prognoses in patients with mass-forming intrahepatic cholangiocarcinoma (MICC).
Material and methods:
Patients who were pathologically diagnosed with MICC and underwent partial hepatectomy between 2012 and 2019 were recruited. Fat-free muscle areas (FFMA) were defined as areas of bilateral erector spinae muscles on dual-echo, T1-weighted, gradient-recalled-echo images at the level of the radix of the superior mesenteric artery. Fat-free skeletal muscle index (FFMI) was calculated by dividing the FFMA by the individual’s height squared. The prognostic value of FFMI was investigated using the Kaplan-Meier method and multivariable Cox regressions in both the entire cohort and in sex-specific subgroups.
Results:
A total of 157 patients were finally included. Cut-off values for the definition of low FFMI were 14.19 cm2/m2 in males and 11.07 cm2/m2 in females. Patients with low FFMI had significantly shorter overall survival (OS) than those with high FFMI in the entire cohort (19.42 vs. 35.29 months, p = 0.0067) and male patients (17.25 vs. 37.19 months, p = 0.006), but not in females. Multivariate analyses showed that low FFMI was a significant predictor of OS in the entire cohort (HR = 1.725, 95% CI: 1.054–2.821, p = 0.030) and in male patients (HR = 2.145, 95% CI: 1.113–4.133, p = 0.023). No association between FFMI and disease-free survival was found in both the entire cohort and sex-specific subgroups.
Conclusions:
Preoperative FFMI measured by MRI is a prognostic biomarker for OS in MICC patients, and it is more sensitive in males than in females.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.