The year 2020 and the ongoing pandemic of a new viral disease with an extremely high virulence [1] has presented modern women choosing to become mothers with particular challenges, not only to their physical health, but also to their mental health [2]. Since the beginning of 2020, women facing the threshold of motherhood have also been struggling with the anxiety of what the course of those 9 months will look like, the sanitary restrictions dictated by the rapidly changing epidemiological situation, the risk of contracting SARS-CoV-2 and the resulting complications, and the lack of certain information on the impact of the disease itself, treatment and vaccination on pregnancy and the developing fetus. Anxiety has been heightened by the feeling of loneliness due to social isolation, the inability of the partner to participate in most procedures, the lack of contact with other pregnant women in birthing schools, the lack of financial stability and limited access to specialists [3, 4]. How common these feelings are can be seen by the appallingly low birth rate during the pandemic – it is the lowest since the Second World War [5]. Responses given by almost 1,000 respondents in a Polish survey testify to the important contribution of factors such as fear of limited access to medical care, as well as childbirth itself in hospital under current conditions and a deterioration of the financial situation [6]. It is worth mentioning that the respondents explicitly denied that the reason for the postponement of procreation plans was due to a deterioration of partner relationships. It seems that in the current situation women are afraid to get pregnant, and parental plans are being put off for a time in the future when conditions become more stable and predictable [6, 7].
Methods
An electronic, voluntary, anonymous survey was completed by 246 women who were pregnant at some stage during the pandemic. A proprietary survey questionnaire, which asked questions relating to feelings of safety among pregnant women/obstetricians, was also shared with participants. The questionnaire consisted of 23 closed questions, 17 questions focused on the course of the pregnancy, health status and social situation. The Pandemic-Related Pregnancy Stress Scale was also used (PREPS – Preis, Mahaffey, & Lobel, 2020 Polish adaptation by Ilska, Kołodziej-Zaleska, Brandt-Salmeri, 2021) after obtaining written consent from the author of the scale. To investigate the problem, the questionnaire included the prenatal stress scale, consisting of the following 3 subscales and items belonging to them: infection-related prenatal stress scale (I-S), preparedness-related prenatal stress scale (P-S), prenatal stress scale related to positive appraisal (POS).
Each item had to be rated on a five-point Likert scale from 1 to 5, where a value of 1 was assigned a rating of “very little”, while a value of 5 was assigned a rating of “very strongly”. The statistical tools used were the two-sided Student’s t test and Spearman’s correlation. Statistical significance was defined as a p-value below 0.05. Statistical calculations were made in the statistical package R Studio.
Results
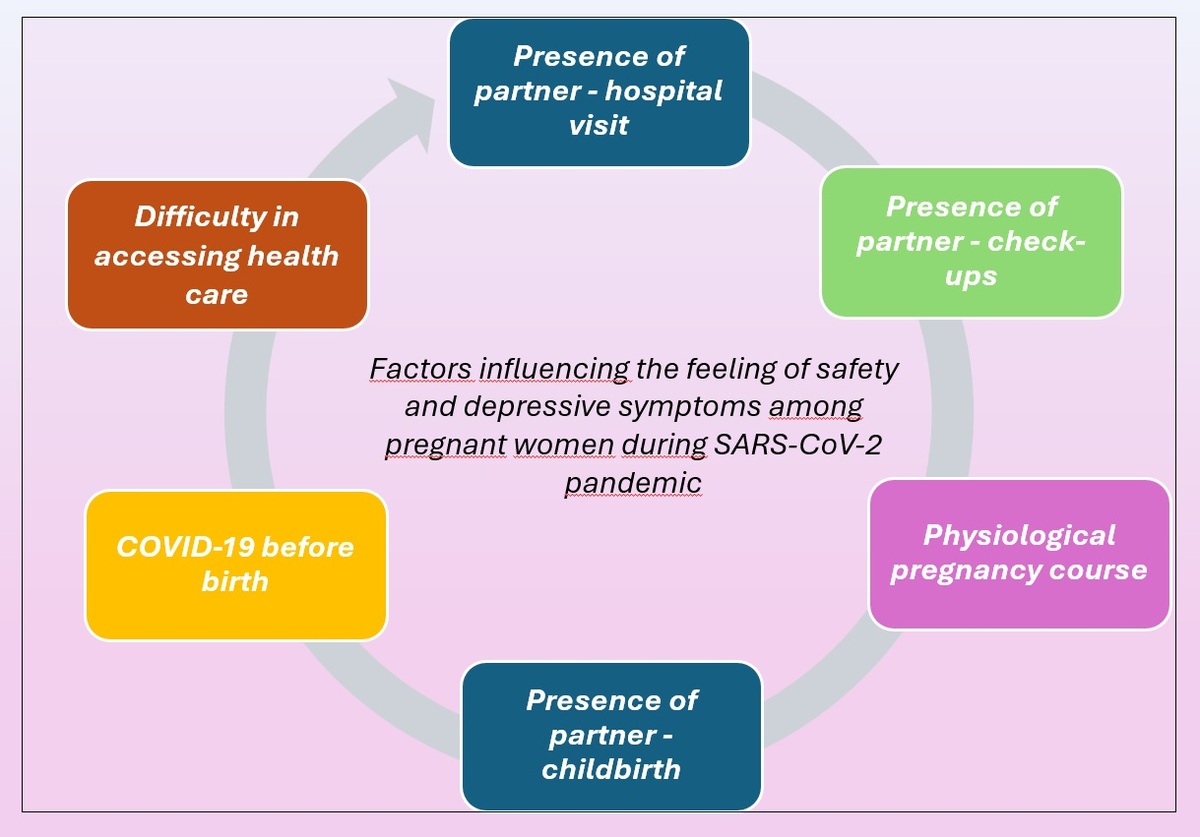
According to the subjective assessment, the presence of a partner at the birth, easy access to health care, the presence of a partner at check-ups and the assistance of an agreed paid specialist at the birth had a significant impact on the sense of safety of the women surveyed. The absence of the same factors had, according to the subjective assessment of the respondents, a negative impact on the feeling of safety. A higher sense of security was characterized by women who did not have any difficulty in accessing health care and whose partner accompanied them in various situations related to the pregnancy (Table I).
Table I
Values of Spearman’s correlation coefficient between individual symptoms in pregnancy and postpartum and individual characterization variables
| Variable | Pregnancy | Postpartum | ||
|---|---|---|---|---|
| Physiological pregnancy course | Fear | –0.19*** | N/A | – |
| COVID-19 before birth | Strength/self–agency | 0.14* | Suicidal thoughts | –0.17** |
| Difficulty in accessing health care | Feeling of safety | –0.16** | N/A | – |
| Presence of partner – check-ups | Calmness | 0.15* | Happiness | –0.21*** |
| Feeling of safety | 0.18** | |||
| Strength/self–agency | 0.14* | Closeness with the child | –0.16** | |
| Closeness with the partner | 0.20*** | |||
| Presence of partner – hospital visit | Negative feelings towards the partner | –0.15* | N/A | – |
| Feeling of safety | 0.16** | |||
| Closeness with the partner | 0.13* | |||
| Presence of partner – childbirth | Anxiety | –0.14* | Sadness | 0.14* |
| Anxiety | 0.20*** | |||
| Happiness | 0.16** | Fear | 0.13* | |
| Helplessness | 0.16** | |||
| Low self–assessment | 0.15* | |||
| Calmness | 0.15* | Happiness | 0.33*** | |
| Calmness | 0.18*** | |||
| Feeling of safety | 0.19*** | |||
| Closeness with the partner | 0.15* | Strength/self–agency | 0.22*** | |
| Closeness with the child | 0.35*** | |||
| Closeness with the partner | 0.31*** | |||
The most significant for prenatal stress during the pandemic was the P-S subscale measuring prenatal stress related to infection, as the mean obtained was the highest for this scale and the results were significantly different from the other two scales. This shows that in the women surveyed prenatal stress related to infection was significantly higher than prenatal stress related to organizing/planning the birth and care and that, despite some positive re-evaluation, the stress related to infection was felt more by them (Table II).
Discussion
We have taken into consideration five studies, and the increase in feelings of anxiety alone among pregnant women tells us that the sense of security is significantly lower than before the pandemic [2, 7, 8]. A study on a population of pregnant Polish women showed that the level of anxiety was significantly higher than before the pandemic [8]. Similarly, research on Jewish and Arab women found that, in the face of the pandemic crisis, women are at risk of psychological distress [9]. In a stress study on a group of 331 pregnant women, the most common psychological response to the pandemic outbreak was depression and anxiety [10]. The father’s presence at childbirth is an interesting issue – it gives the woman a sense of security, acceptance, and freedom to express her feelings and needs [11, 12]. In our own study, a number of contradictions were seemingly demonstrated in this regard. Positive symptoms show greater relevance and a stronger correlation, but it cannot be concluded that family birth protects against the development of depressive symptoms. In the context of the COVID-19 pandemic we found elevated levels of infection-related stress among our respondents (based on the PREPS scale), which affected their sense of safety. The role of stress related to the organization of the birth was slightly lower, but it was also experienced. It fostered negative feelings towards the partner after the birth – this seems logical, since the stress was about what, to some extent, the partner had an influence on. The conclusion is that, considering all the predictive models, it appears that the variables that most frequently recur in worsening anxiety and depressive symptomatology are fear of contagion, loneliness and experienced stress, more so than other variables [13, 14]. The occurrence of positive reappraisal was also reported among respondents, but prenatal stress due to the pandemic was recorded at a higher level.
The most interesting finding is that the impact of the presence of a partner at the birth will, for some mothers, have a protective effect, reducing the risk of depressive symptoms, while for others it will exacerbate this risk.
The main limitation of the study was the retrospective completion of a survey among women who were pregnant at some stage of the pandemic, while feelings of anxiety and fear may have changed with the successive waves of the pandemic.
In conclusion, the impact of the SARS-CoV-2 pandemic on the wellbeing of pregnant women remains negative.