A 65-year-old male with a history of two myocardial infarctions (in 2000 and 2007), atrial fibrillation, hypertension, type 2 diabetes, gout, and prostate hypertrophy presented to the urology outpatient clinic due to hematuria noticed in November 2020. An abnormal growth in the patient’s urinary bladder led to transurethral resection of the tumor. Pathology confirmed low-grade papillary urothelial cancer, staged as pTa. Computed tomography (CT) scans of the thorax, abdomen, and pelvis revealed a suspicious mass in the right lung hilum. Positron emission tomography (PET) imaging and bronchoscopy with biopsy were performed. Pathology confirmed a diagnosis of lung adenocarcinoma (Figure 1). The disease was staged as cT4N1M1c, with dissemination to the right adrenal gland and focal metastatic lesions in the abdomen. The patient began chemo-immunotherapy with cisplatin, pemetrexed and pembrolizumab in February 2021. Initially, 4 courses were planned. Treatment tolerance and the patient’s condition throughout the courses were satisfactory, with no severe adverse events reported. Restaging examinations performed after the 2nd and 4th courses showed stable disease. A decision had been made to continue treatment with pemetrexed and pembrolizumab.
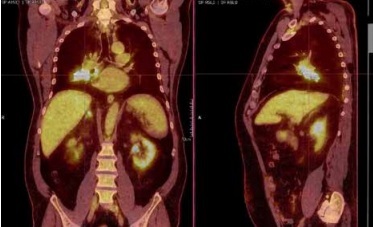
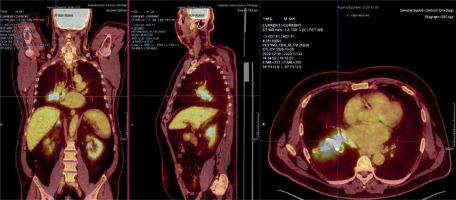
Figure 1
Positron emission tomography with 18F-fluorodeoxyglucose performed during the diagnostic process. A 50 × 92 × 70 cm lesion with increased glucose metabolism is visible, extending from the hilum to the lower lobe of the right lung
In April, the patient reported shortness of breath and a productive cough. Tests revealed an increased serum concentration of procalcitonin (PCT) (Table I). However, these symptoms did not correlate with other laboratory tests, such as C-reactive protein (CRP), blood and urinary cultures, physical examination findings, or imaging results. Presence of infection, pulmonary embolism, renal or liver failure, eosinophilia, severe hyperglycemia and medication-related causes were ruled out, indicating the cancer as the cause of elevated PCT. The patient underwent two more courses of systemic treatment but reported worsening of the symptoms in June 2021. The concentrations of PCT were increasing, still without any correlation with CRP or bacteria cultures (Table I). Symptomatic treatment led to remission of the symptoms. Soon after that, the patient reported hemoptysis and was qualified for palliative radiation therapy targeting the right lung tumor. Restaging CT imaging showed progression of the primary tumor and new metastatic lesions in both lungs, left adrenal gland, bones and abdominal subcutaneous tissue. Due to severe pain, he received palliative radiation therapy to C7-Th2 and L1-S1 sections of the spine. In July 2021, second-line single-agent systemic therapy with docetaxel was started but elicited no response. CT scans performed in August 2021 again showed disease progression (Figure 2). PCT was extremely elevated, still without infection symptoms, low CRP value and negative blood cultures (Table I). Due to no response to treatment and worsening general condition, best supportive care was introduced. The patient died in September 2021.
Table I
Concentrations of serum procalcitonin at subsequent time points during treatment
| Date | Serum procalcitonin [ng/ml] (Normal values: 0.00–0.05 ng/ml) |
|---|---|
| 28.04.2021 | 9.83 |
| 28.04.2021 | 9.51 |
| 10.06.2021 | 53.45 |
| 11.06.2021 | 47.20 |
| 14.06.2021 | 59.93 |
| 15.06.2021 | 62.01 |
| 23.06.2021 | 72.62 |
| 26.08.2021 | 477.10 |
| 29.08.2021 | 880.16 |
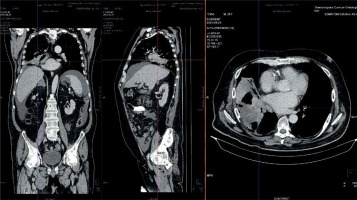
Figure 2
Computed tomography of the thorax, abdomen and pelvis performed after the last line of treatment. Radiology reported enlargement of the tumor of the right lung as well as new metastases to the left and right lung, left adrenal gland, bones and abdominal subcutaneous tissue
Although elevated PCT is often reported in patients with various malignant tumors or other medical conditions, this is the first report of a lung cancer patient presenting with such extremely high concentration of this peptide without associated infection [1–3]. Elevated PCT is a negative prognostic factor in lung cancer patients, as proven in the literature. In the described patient we observed a similar pattern – very limited response to treatment and rapid dissemination of the disease [1, 4, 5]. Kajikawa et al. found a significantly negative influence of elevated PCT on overall survival curves of non-small cell lung cancer (NSCLC) patients when compared with patients without PCT elevation [4]. Additionally, Garoutte et al. discovered that among patients with NSCLC, only the ones with liver metastases presented with elevated PCT [5]. Physicians should consider hyperprocalcitoninemia without infection as potentially indicative of the underlying malignant disease.