Introduction
Systemic lupus erythematosus (SLE) is a prototypic autoimmune disorder with a variable clinical course, ranging from mild to severe forms. It mainly occurs in women, especially those of fertile age [1, 2]. Due to the advances in obstetrics and rheumatology, pregnancy is now feasible for the majority of female SLE patients [3, 4]. However, the risk of adverse pregnancy outcomes in SLE patients is still high, especially fetal loss, neonatal death, fetal growth restriction (FGR) and preeclampsia [4].
A variety of factors may be related to fetal and maternal adverse outcomes, among which disease activity is the most concerned [5]. Lupus nephritis has been found to increase the risk of hypertension disorders of pregnancy in women with SLE [6], and even those with previous renal flare were reported to have increased incidence of eclampsia [7] and FGR [8]. Consequently, women with SLE are recommended to consider pregnancy during periods of inactive or stable disease [9], because active disease has been identified as an important predictor for poor pregnancy outcomes [10], while a remission at least 6 months before conception could reduce the risk of unfavorable pregnancy outcomes [11].
Currently, it is still unclear what kind of disease activity is associated with a certain unsatisfactory pregnancy outcome and whether it will affect the offspring of patients. In this study, we summarized the main adverse outcomes during the prenatal period through retrospective analysis of 198 deliveries of 194 SLE patients, and then searched for their associations with the sub-items of the SLE disease activity index (SLEDAI) at the time of delivery. Meanwhile, the living status of patients’ offspring was also evaluated and compared with their peers.
Material and methods
Patients
A retrospective review of medical records of consecutive deliveries of SLE patients admitted to the obstetrics department of Nanjing Drum Tower Hospital from October 2001 to January 2018 was performed. All SLE patients fulfilled the 1997 American College of Rheumatology revised criteria for SLE [12]. Organ activity was defined as follows: neurological activity (seizure, psychosis, organic brain syndrome, visual disturbance, cranial nerve disorder, lupus headache and cerebrovascular accident), vasculitis, arthritis, myositis, renal activity (urinary casts, hematuria, proteinuria and pyuria), mucocutaneous activity (rash, alopecia and mucosal ulcers), serositis (pleurisy and pericarditis), low complement, increased DNA binding, fever, hematologic activity (thrombocytopenia and leukopenia). Overall disease activity was evaluated according to the SLE Disease Activity Index 2000 (SLEDAI-2k) [13]. According to the criteria, 0–6 points represented mild activity, 7–12 points represented moderate activity, and > 12 points represented severe activity [14]. Survival and growth status of offspring of SLE patients was checked in March 2020 and those lost to follow-up were excluded from the cohort. Data of deliveries of normal pregnant women in the same period were also collected as a control group matched for age, gender and body mass index (BMI). Those with co-infections, serious systemic diseases or inflammatory rheumatic diseases were excluded from the healthy control group.
Classification of adverse outcomes
Maternal adverse outcomes were defined as having one or more of the following: 1) gestational hypertension (systolic blood pressure (SBP) > 140 mm Hg and/or diastolic blood pressure (DBP) > 90 mm Hg after the 20th week of gestation in a previously normotensive woman), 2) preeclampsia (proteinuria or new end-organ dysfunction after 20 weeks of gestation in women with de novo or superimposed on chronic hypertension)/eclampsia (with the occurrence of seizures in patients with preeclampsia), 3) puerperal infection, 4) placental anomalies (including placental abruption, placenta previa and placental adherence), 5) gestational diabetes mellitus (abnormalities in glucose metabolism first detected or occurring during pregnancy), 6) others: intrahepatic cholestasis (a disorder of pregnancy occurring in the third trimester, characterized by pruritus, elevated serum transaminases and serum bile acids) and pulmonary hypertension (systolic pulmonary arterial pressures ≥ 35 mmHg estimated by Doppler echocardiography).
Fetal adverse outcomes were defined as having one or more of the following: 1) low birth weight (a live born weight less than 2500 g), 2) premature birth (live birth before 37 weeks of gestation), 3) fetal growth restriction (FGR) (with birth weight below the 10th percentile of the Chinese population according to gestational week at delivery and fetal gender), 4) fetal distress (fetus hypoxia and acidosis which could endanger the health of the fetus), 5) neonatal asphyxia (the combination of systemic hypoxemia, hypercapnia, and metabolic acidosis that may occur before and during birth and the neonatal period), 6) congenital heart disease, 7) others: fetal death (intrauterine fetal demise after 20 weeks of gestation unexplained by chromosomal abnormalities, anatomic malformation, or congenital infection), neonatal death (the death of a live infant within 28 days after birth) and congenital malformation.
Normal values for laboratory tests were as follows: white blood cells (WBC) 4–10 × 109/l, hemoglobin ≥ 110 g/l (female), platelets 125–350 × 109/l, complement C3 0.8–1.6 g/l, C4 0.2–0.4 g/l, erythrocyte sedimentation rate (ESR) ≤ 20 mm/h, C-reactive protein (CRP) ≤ 8 mg/dl, serum creatinine 44–106 µmol/l.
Outcomes of offspring of SLE patients were defined by referring to previous literature, including stunting [15], underweight [15], anemia [16], learning disorders [17], sensory integration dysfunction [18], eczema [19], dental caries [20], allergic rhinitis or allergic asthma [21], congenital heart disease [22] and respiratory tract infection in infancy [23]. Data from a number of large census studies on children’s long-term outcomes [15, 16, 24–28] and other reported studies on long-term outcomes in offspring of SLE patients [29–32] were applied as normal controls and disease controls respectively.
Statistical analysis
Data were analyzed using SPSS 23.0 software or GraphPad Prism 7.0. Values were presented as mean with standard deviation (SD) for continuous variables and number (percent) for categorical variables. Intergroup comparisons were performed using the χ2 test. To ascertain the independent effect of various parameters on pregnancy outcomes, univariate analysis using the logistic regression analysis model was conducted. Variables significant (p < 0.05) in univariate analysis were then included in the multivariate model, and results were reported as odds ratios (OR) with 95% confidence intervals (CI). A p-value < 0.05 was considered significant.
Results
Characteristics of the cohort
In total, 198 deliveries of 194 SLE patients were included in the analysis. Renal activity was the most common manifestation, followed by hematological involvement. Based on the SLEDAI-2K score, 141 (71.2%) patients had mild activity, while 39 (19.7%) and 18 (9.1%) had moderate and severe disease activity before their deliveries. A vast majority of patients received low dose corticosteroids (91.1%) and hydroxychloroquine (67.5%) (Table I).
Table I
Characteristics of patients
Major adverse perinatal outcomes in SLE patients
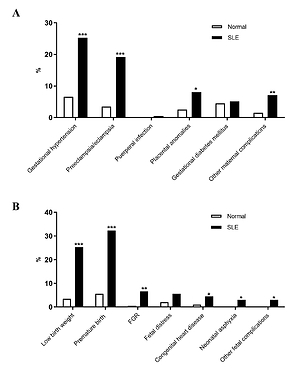
In the SLE group, 74 (37.4%) and 90 (45.5%) deliveries were recorded with at least one episode of maternal and fetal adverse outcomes, respectively. Compared with normal subjects, SLE patients displayed higher rates of gestational hypertension (p < 0.001), preeclampsia/eclampsia (p < 0.001) and placental anomalies (p < 0.05) (Figure 1 A), low birth weight (p < 0.001), premature birth (p < 0.001), FGR (p < 0.01), congenital heart disease (p < 0.05) and neonatal asphyxia (p < 0.05) (Figure 1 B).
Figure 1
Maternal and fetal adverse outcomes between normal women and women with systemic lupus erythematosus (SLE). Women with SLE had higher risk of gestational hypertension (p < 0.001), preeclampsia/eclampsia (p < 0.001) and placental anomalies (p < 0.05) than normal women. Compared to normal women, women with SLE had higher incidence of low birth weight (p < 0.001), premature birth (p < 0.001), fetal growth restriction (FGR) (p < 0.01), congenital heart disease (p < 0.05) and neonatal asphyxia (p < 0.05). Placental anomalies included placental abruption, placenta previa and placental adherence. Other maternal complications included pulmonary hypertension and intrahepatic cholestasis. Other fetal complications included fetal death, neonatal death and congenital malformation. *p < 0.05, **p < 0.01, ***p < 0.001
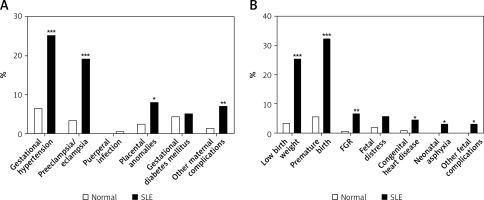
Then, the variations in adverse outcomes across disease activity states were compared. Patients with moderate and severe disease activity (active group) had higher rates of gestational hypertension (p < 0.001) and preeclampsia/eclampsia (p < 0.001) than those with mild disease activity (inactive group) (Figure 2 A). In terms of fetal adverse outcomes, the rates of low birth weight (p < 0.001), premature birth (p < 0.001) and FGR (p < 0.01) were higher in the active group than the inactive group (Figure 2 B).
Figure 2
Maternal and fetal adverse outcomes between women with systemic lupus erythematosus (SLE) with and without active disease. A – Women with active SLE had higher risk of gestational hypertension (p < 0.001) and preeclampsia/eclampsia (p < 0.001) than women with inactive SLE. B – The incidence rates of low birth weight (p < 0.001), premature birth (p < 0.001) and FGR (p < 0.01) were higher in women with active SLE than those with inactive SLE. Placental anomalies included placental abruption, placenta previa and placental adherence. Other maternal complications included pulmonary hypertension and intrahepatic cholestasis. Other fetal complications included fetal death, neonatal death and congenital malformation. FGR – fetalgrowth restriction. *p < 0.05, **p < 0.01, ***p < 0.001
Association of specific organ activity with maternal adverse outcomes
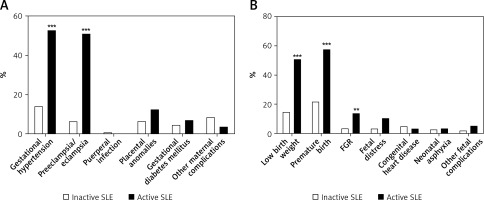
To find out what organ activity contributed to increased maternal adverse outcomes, SLEDAI-2k sub-items were categorized and analyzed by univariate logistic regression. Gestational hypertension was associated with renal activity (OR = 4.04, p = 0.001), serositis (OR = 3.90, p < 0.05) and hematologic activity (OR = 3.85, p < 0.01). Preeclampsia/eclampsia was linked to renal activity (OR = 9.57, p < 0.001), serositis (OR = 3.89, p < 0.05), low complement (OR = 4.26, p < 0.05), increased DNA binding (OR = 2.62, p < 0.05) and hematologic activity (OR = 4.05, p = 0.001). Next, multivariate logistic analysis was performed to find out the independent risk factors. Renal activity (OR = 4.43, p < 0.001) and hematologic activity (OR = 3.07, p < 0.05) were still associated with gestational hypertension (Figure 3 A), while renal activity (OR = 9.14, p < 0.001) and low complement (OR = 3.15, p < 0.05) were independently linked to preeclampsia/eclampsia (Figure 3 B).
Figure 3
Key factors for special maternal and fetal adverse outcomes in women with systemic lupus erythematosus (SLE) by multivariate logistic analysis. A – Renal activity (p < 0.001) and hematologic activity (p < 0.05) were key factors for gestational hypertension. B – Renal activity (p < 0.001) and low complement (p < 0.05) were key factors for preeclampsia/eclampsia. C – Renal activity (p < 0.05), mucocutaneous activity (p < 0.05) and serositis (p < 0.05) were key factors for low birth weight. D – The key factors for premature birth were renal activity (p < 0.001) and mucocutaneous activity (p < 0.01)

Association of specific organ activity with fetal adverse outcomes
The univariate logistic regression analysis revealed that low birth weight was linked to renal activity (OR = 2.14, p < 0.05), mucocutaneous activity (OR = 3.58, p < 0.01), serositis (OR = 5.86, p < 0.01) and low complement (OR = 3.48, p < 0.05), while premature birth was associated with renal activity (OR = 3.42, p = 0.001), mucocutaneous activity (OR = 4.25, p = 0.001) and serositis (OR = 3.99, p < 0.05), and FGR was related to mucocutaneous activity (OR = 3.67, p < 0.05). Among these, renal activity (OR = 2.24, p < 0.05), mucocutaneous activity (OR = 3.26, p < 0.05) and serositis (OR = 4.32, p < 0.05) remained significant for low birth weight in multivariate logistic analysis (Figure 3 C); so did renal activity (OR = 4.20, p < 0.001) and mucocutaneous activity (OR = 4.07, p < 0.01) for premature birth (Figure 3 D).
Follow-up of offspring of SLE patients
Among all offspring of SLE patients, one died at birth, one died at the age of 5 months and 54 were lost to contact. The remaining 142 children were followed up for 4.8 (minimum 2.2 to maximum 9.6) years. As shown in Table II, 4.2% suffered from congenital heart diseases, including one congenital heart block, one ventricular septal defect, 2 cases of patent foramen ovale and 3 cases of atrial septal defect, which were high compared with the data of Chinese children in the general population. Meanwhile, offspring of SLE patients also had elevated frequency of eczema (35.2%). In total, 51 (35.9%) children experienced respiratory tract infection 3 or more times per year and 13 (9.2%) children received intravenous transfusion treatment 3 or more times per year due to severe respiratory tract infection during the infantile period.
Table II
Characteristics of offspring of systemic lupus erythematosus (SLE) patients
Association of perinatal disease activity with growth of offspring of SLE patients
In order to study the influence of perinatal disease activity on long-term outcomes of offspring of SLE patients, the rates of long-term events in offspring of SLE patients were compared across disease activity states. To our surprise, there were no differences in the rates of stunting, underweight, anemia, learning disorders, sensory integration dysfunction, eczema, dental caries, allergic rhinitis/allergic asthma, congenital heart disease and respiratory tract infection in infancy between offspring of SLE patients with active disease and those of SLE patients without active disease (Figure 4). However, the data showed that offspring of SLE patients with eczema had higher frequency of anti-Ro60 antibody than those without (40.0% vs. 16.7%, p < 0.05), while offspring of SLE patients with repeated respiratory tract infection had lower frequency of anti-Ro52 antibody (4.3% vs. 27.3%, p < 0.05) but higher frequency of immunosuppressant use (17.6% vs. 5.7%, p < 0.05) (data not shown).
Discussion
This study analyzed the perinatal characteristics of SLE patients in a single center and confirmed that women with SLE had higher rates of adverse prenatal outcomes than normal subjects. Renal activity was the most important organ activity of women with SLE in predicting a variety of adverse pregnancy outcomes, including gestational hypertension, preeclampsia/eclampsia, low birth weight and premature birth. Symptomatically, proteinuria and thrombocytopenia were of particular concern because of their strong association with poor outcomes. However, it was demonstrated for the first time that most lupus offspring grew well regardless of maternal perinatal disease activity, although they had high rates of eczema and repeated respiratory tract infections in infancy.
So far, only a few studies have discussed the outcomes of offspring of SLE patients and the results are controversial, due to the small number of studies, different evaluation methods and research designs [30, 33]. Some studies suggested that maternal SLE was associated with learning disorders, autism spectrum disorders, attention deficit and probably problems in offspring, but they were assigned a low or moderate level [30]. In this cohort, most offspring of SLE patients grew well, irrespective of perinatal disease activity. The percentage of learning disorders was 2.8%, lower than that (21.4–26.0%) observed in overseas research, which could be attributed to different definition and assessment tools of learning disorders and subjects’ age among studies [17, 34].
The growth of children born to women with SLE is worthy of attention. However, relevant reports are rare and there is no consensus in the findings. This study identified a link between lupus disease activity and adverse pregnancy events, but no association between long-term growth of offspring of SLE patients and lupus disease activity. Several studies focusing on neurologic and cognitive development have produced similar results. A national study confirmed the association between SLE and preterm birth, but there was no difference in neurological disease between children of women with or without SLE [35]. Not only SLE, but also hydroxychloroquine and/or immunosuppressants were found to have no significant deleterious effects on the neurocognitive development of children [36].
The reason for the lack of significant difference between healthy newborns and neonates born to mothers with SLE is currently unknown. Although some fetuses of SLE patients developed growth retardation, this difference was not significant after birth, suggesting that the postnatal environment may be more important for the growth of offspring of lupus patients. In addition, some adverse manifestations of offspring of SLE patients, such as respiratory tract infection during infancy and eczema, may be caused by specific maternal autoantibody phenotype and immunosuppressive therapy. For example, positive anti-SSA antibody is more likely to be seen in SLE patients whose offspring develop eczema (data not shown). There have been a few reports of eczema complicated by SLE, which may also be associated with anti-SSA [37].
There are some limitations of this study. Firstly, this retrospective investigation depended on the analysis of medical records, so some gaps remained despite efforts to maximize data collection. Secondly, there was a center bias. As a provincial tertiary hospital, more pregnant women with SLE with severe activity and complex complications were enrolled in our hospital. Thirdly, the small rates of neurological involvement and vasculitis in this cohort make it difficult to assess the role of these factors.
In conclusion, perinatal disease activity has a great impact on mothers with SLE and their fetuses, and renal activity is the most critical aspect in prediction of various adverse outcomes. Careful monitoring and control of perinatal disease activity, especially renal activity, are necessary for a successful pregnancy. However, growth of offspring of SLE patients seems not to be affected by perinatal disease activity.