Introduction
Osteoarthritis (OA) is a highly prevalent and disabling disease that affects more than 7% of the world’s population (528 million people), with even higher prevalence in developed countries where the population is highly aged and obesity rates are higher, such as in the United States (14%) [1]. The knee is the most commonly involved joint in osteoarthritis, which accounts for 87% of OA and is the leading cause of functional limitation and pain in adults, affecting more than 250 million people worldwide [2–4]. A 10-year survey in China showed that the 10-year average age-standardized prevalence of knee osteoarthritis (KOA) was 4.6% per 1000 person-years, with a 10-year incidence rate of 25.2, and the prevalence of KOA tended to increase with age, with the study finding a spike in KOA prevalence after age 55 years, with an average prevalence of 13.2% in that age group [4]. Among patients with KOA, 36.8% to 60.7% have different degrees of pain, 52% have combined insomnia (which is 3 times the prevalence of insomnia in the general population), 17% of them have depression, and direct medical costs of patients with both KOA and depression are more than 30% higher than those with only KOA: in the UK, France, and the US, from the annual disability benefits and labour force of KOA patients, the cost of loss, etc. is about $3.4 to $13.2 billion [5–7]. Dragan Primorac’s study showed that in this population aged 60 years or older, the prevalence of OA is about 13% for women and 10% for men, and KOA has become one of the leading causes of disability in the elderly [8]. In summary, KOA brings a huge burden of disease and economic loss to patients, the government, and society [9–11].
The main treatments for KOA include medication, physical therapy, and surgery, the medication of which has side effects, and surgery is only applicable to patients with end-stage KOA; therefore, physical therapy is currently receiving more and more attention, and mind-body therapy is one of the physical therapies [12, 13]. In 2021, an Italian multidisciplinary best practice on the non-surgical treatment of KOA stated that mind-body therapy could be considered as a treatment for patients with KOA [14]. Aerobic exercise and mind-body therapy are thought to be the greatest treatments for pain and function for KOA patients, based on Siew-Li Goh’s study [15]. According to Romy’s research, yoga can help KOA sufferers feel less stiff and less discomfort, and perform better [16]. According to Zhi-peng Zeng’s research, Baduanjin exercises can help KOA sufferers feel less pain and be more active [17]. A network meta-analysis of the efficacy of nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, and exercise therapy for KOA showed that exercise therapy could be the best option for pain in patients with KOA, followed by NSAIDs and opioids, but the results of the study also showed little difference between the 3 rankings [18]. Although mind-body therapies are an important part of the management of KOA, and there is a growing body of research confirming the effectiveness of mind-body therapies for KOA, there is still some controversy surrounding the treatment of KOA with mind-body therapies. Kolasinski’s study showed that clinical trials involving mind-body therapies were often designated as low-quality evidence in the GRADE analysis because blinded implementation is usually poor [19]. Secondly, there are many types of mind-body therapies involved, and there is not enough evidence to show that one type of exercise is better than another. Network meta-analysis is a statistical analysis method that enables indirect comparisons, and it has been used to evaluate and measure the effectiveness and safety of multiple interventions in similar subjects in the absence of directly comparable original studies, and to support the ranking of interventions according to an outcome indicator, which can provide a more focused and reliable basis for clinical research [20]. Because of this, the current study used a Network Meta-analysis to systematically assess the effects of various mind-body therapies on interventions for patients with KOA to supply healthcare professionals with an evidence-based basis on which to develop the best exercise regimens.
Material and methods
Protocol and registration
The study was conducted in compliance with the PRISMA statement [21]. Our study has been previously published in INPLASY (registration number: 202270084).
Search strategy
Our research is based on the PICOS tool to develop a search strategy: (P) Population: Patients aged ≥ 18 years with a diagnosis of KOA according to the American College of Rheumatology (ACR) [22] clinical criteria for KOA, (I) Intervention: Various types of mind-body therapies, including Baduanjin exercises, retro walking, forward walking, Pilates, Taiji, Yoga, Wuqinxi, Yijinjing, balance training, MBSR, CBT, meditation, etc, (C) Comparator: control group with only daily exercise or daily nurse or no intervention, (O) Outcomes: The WOMAC score, TUG test, or SF-36 score of the study population were used as the outcome indicators for this study, (S) Study type: RCTs. Through searching Cochrane Library, PubMed, EBSCO, Web of science, Medline, and Embase, only randomized controlled trials (RCTs) were collected to study the effects of different mind-body therapies on patients with KOA. The search period was January 2007 – May 2022. Search expressions were constructed in terms of subject terms plus free words, while tracing references for inclusion in the literature. The detailed search strategy can be found in Table I, using PubMed as an example.
Table I
Search strategy on PubMed
Inclusion criteria
Based on the criteria outlined in the PICOS principles we screened and assessed the material, and based on the outcomes we decided whether it should be included. (P) Population: Patients aged ≥ 18 years with a diagnosis of KOA according to the American College of Rheumatology (ACR) [22] clinical criteria for knee osteoarthritis, (I) Intervention: Various types of mind-body therapies, including Baduanjin exercises, retro walking, forward walking, Pilates, Taiji, yoga, Wuqinxi, Yijinjing, balance training, MBSR, CBT, meditation, etc, (C) Comparator: control group with only daily exercise or daily nurse or no intervention, (O) Outcomes: The WOMAC score, TUG test, or SF-36 score of the study population were used as the outcome indicators for this study, (S) Study type: RCTs.
Exclusion criteria
(1) Literature for which raw data were not available and data could not be extracted/combined, (2) Unpublished or duplicate publications; (3) Literature with a quality grade of C, (4) Literature not in English, (5) Related studies in the category of non-randomized controlled trials.
Study selection
Two researchers (Yanfei Ma and Ailin Hou) screened the literature alone, extracted the information, and summarized it for examination. In cases of disagreement between the 2 researchers, a third researcher (Rong Hu) was consulted to assist in judgment. Reading the literature’s titles and abstracts allowed for the first initial screening, which aimed to weed out any works that were unrelated to the subject. The next stage was to rescreen the literature using the already determined inclusion and exclusion criteria while reading the whole text. First author, year of publication, nation, study population, age, sample size, intervention, intervention duration, intervention frequency, and outcome indicators were all extracted from the collected literature using a standard form.
Based on the Cochrane Handbook version 5.1.0 tool for assessing the risk of bias in RCTs, 2 researchers (Yanfei Ma and Ailin Hou) independently assessed the risk of bias (ROB) in the final included literature. The assessment tool contained the following 7 main aspects: generation of randomized sequences, concealment of treatment assignment, blinding of participants and personnel, incomplete outcome data, selective reporting, and other sources of bias. Based on the assessment results, “low risk of bias”, “high risk of bias”, and “unclear” could be presented. If the evaluation criteria were fully satisfied, the quality of the literature was A. If the evaluation criteria were partially satisfied, the quality of the literature was B. If the evaluation criteria were not fully satisfied, the quality of the literature was C [14]. The work was eventually published in the literature at the A and B levels. If disagreement developed during the examination of the literature’s risk of bias, a third investigator (Rong Hu) was brought into the discussion to help make a decision.
Data analysis
Our study used State software (version 15.1) to conduct a network meta-analysis. In this study, the intervention was mind-body therapy, and the variables involved were all continuous variables, so they are expressed as means and standard deviations (SD) [23]. A grid of direct and indirect comparisons between the outcomes of the different interventions was produced by State software. Dots indicate interventions, with larger dots indicating more patients receiving the intervention, straight lines indicating the presence of evidence of direct comparisons between 2 interventions, and thicker lines indicating the number of studies in which the 2 interventions were compared directly. Because of the potential differences that must exist between studies, we chose a random-effects model for the analysis rather than a fixed-effects model [24]. The ranking of interventions is reported as a P score, which is an iterative simulation of the probability under the SUCRA curve, and the ranking of each intervention is determined by ranking the SUCRA values from largest to smallest [25]. The closer the P score is to 1, the higher the probability that it is the optimal solution, and the closer the P score is to 0, the lower the probability that it is the optimal solution. Although the P scores and the area under the SUCRA curve after iteration allow us to determine the ranking of the interventions, these scores should be interpreted and used with caution. To test for publication bias due to small sample effects, we performed a funnel plot analysis and determined whether our study was subject to publication bias by symmetry [26].
Results
Study identification and selection
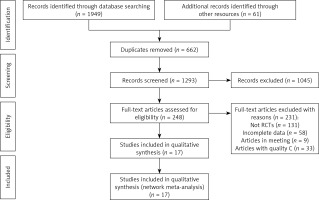
In total, the researcher obtained 1955 documents from databases and other sources. First, the researcher removed 1293 documents after removing duplicates by computer software. Second, the researcher de-duplicated 1045 documents that were not related to the topic by reading the titles and abstracts of the documents. Third, the researcher removed 231 duplicates by reading the full text and reviewing the inclusion criteria as well as the exclusion criteria. Finally, our investigation contained 17 documents (Figure 1).
Quality assessment of the included literature
Five of the 17 studies were rated as low risk, 2 as high risk, and 10 as moderate risk following independent evaluation and pooling by 2 researchers (Yanfei Ma, Ailin Hou). There were some challenges in ensuring the simultaneous blinding of patients and measurers because the intervention in this study involved mind-body therapy and the study participants needed to stick to some form of exercise for a length of time. Table II contains the relevant information.
Table II
Basic characteristics of included randomized controlled trials
| Author | Year | Country | Sample | Age, mean (SD) | Interventions | K/L | Intervention frequency | Intervention length | Outcomes | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T | C | T | C | T | C | T | C | ||||||
| Ye [27] | 2020 | China | 28 | 28 | 65.11 (6.57) | 63.61 (2.63) | Baduanjin exercises | Daily nurse | / | / | 3 times/week | 12 weeks | WOMAC |
| Alghadir [28] | 2019 | Arab | 21 | ①20 ②18 | 54.6 (45–66) | ①56.8 (46–66) ②55.3 (47–65) | Retro walking | ①Forward walking ②Daily exercise | / | / | 3 days/week | 6 weeks | WOMAC, TUG |
| Chen [29] | 2021 | China | 16 | 16 | 60.31 (7.85) | 60.94 (6.89) | Retro walking | Daily nurse | 3.38(0.619) | 3.19(0.66) | Once a week | 4 weeks | WOMAC |
| Ye [30] | 2019 | China | 25 | 25 | 64.48 (7.81) | 63.08 (3.65) | Baduanjin | Daily nurse | / | / | 3 times/week | 12-week | WOMAC |
| Saleem [31] | 2022 | Pakistan | 20 | 20 | 57.60 (6.34) | 55.65 (7.28) | Pilates | Daily exercise | / | / | 3 times/week | 8 weeks | WOMAC |
| Zhu [32] | 2016 | China | 23 | 23 | 64.61 (3.40) | 64.53 (3.43) | Taiji | Daily nurse | Grade 1 (30.43%) Grade 2 (52.17%) Grade 3 (17.40%) | Grade 1 (26.09%) Grade 2 (60.87%) Grade 3 (13.04%) | 3 times/week | 24 weeks | WOMAC |
| Brismée [33] | 2007 | USA | 22 | 19 | 70.8 (9.8) | 68.8 (8.9) | Taiji | Daily nurse | / | / | 3 times/week | 6 weeks | WOMAC |
| Lee [34] | 2009 | Korea | 29 | 15 | 70.2 (4.8) | 66.9 (6.0) | Taiji | Daily nurse | Grade 2 (48.27%) Grade 3 (44.83%) Grade 4 (6.90%) Grade 2 (53.33%) | Grade 3 (46.67%) Grade 4 (0%) | Twice a week | 8 weeks | WOMAC, SF-36 |
| Xiao [35] | 2020 | China | 49 | 49 | 70.7 (9.36) | 70.2 (10.35) | Wuqinxi | Daily exercise | / | / | Four times/week | 24 weeks | WOMAC, TUG |
| Zhang [36] | 2021 | China | 22 | 21 | 55.76 (8.37) | 53.40 (10.66) | Yijinjing | Daily exercise | / | / | Twice a week | 12 weeks | WOMAC |
| Cheung [37] | 2017 | USA | 32 | ①28 ②23 | 68.9 (7.7) | ①74.4(7.5) ②71.8(8.0) | Yoga | ①Daily exercise ②Daily nurse | / | / | 2–4 days/week | 8 weeks | WOMAC |
| Cheung [38] | 2014 | USA | 18 | 18 | 71.9 (5.33) | 71.9 (6.03) | Yoga | Daily nurse | / | / | Once a week | 8 weeks | WOMAC |
| Marais [39] | 2022 | French | 20 | 20 | 63.0 (7.4) | 56.2 (12.9) | MBSR | Daily nurse | / | / | Two-and-a-half-hour weekly | 8 weeks | WOMAC, SF-36 |
| Lee [40] | 2021 | Korea | 19 | 19 | 72.05 (5.15) | 71.89 (5.44) | Balance training | Daily exercise | / | / | Five times/week | Six weeks | WOMAC, TUG, SF-36 |
| Smith [41] | 2015 | USA | 50 | 50 | 59.2 (9.9) | 59.6 (9.1) | CBT | Daily nurse | 2.3 (1.1) | 2.4 (1.2) | 8-session (45 mins/session) | / | WOMAC |
| Kuntz [42] | 2018 | Canada | 10 | ①11 ②10 | 65.5 (5.6) | ①63.7 (8.9) ②71.1 (9.3) | Yoga | ①Daily exercise ②Daily nurse | / | / | Three 1-hour group classes/sessions each week | 12 weeks | TUG |
| Innes [43] | 2018 | USA | 11 | 11 | 58.09 (1.60) | 58.82 (2.23) | meditation | Daily Nurse | / | / | Twice/day | 8 weeks | SF-36 |
[i] MBSR – mindfulness-based stress reduction, CBT – cognitive behavioural therapy, SF-36 – Health-related Quality of Life, MHC – Mental Health Component, PHC – Physical Health Component, WOMAC – Western Ontario and McMaster Universities Osteoarthritis Index, TUG – Time up and go test, T – experimental group, C – control group, K/L – Kellgren/Lawrence.
Characteristics of the included literature
Finally, our review incorporated research from 17 randomized controlled trials with a total of 859 KOA patients. Thirteen different mind-body practices, including Baduanjin exercises, retro and forward walking, Pilates, Taiji, yoga, Wuqinxi, Yijinjing, balance training, MBSR, CBT, and meditation, are included in this study. Daily nursing or daily exercise interventions made up the control group’s interventions. Table II provides details of the included literature [27–43].
Network analysis
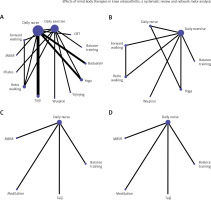
The full NMA figure is shown in Figures 2 A–D.
Figure 2
A – NMA figure for WOMAC. B – NMA figure for TUG. C – NMA figure for MHC. D – NMA figure for PHC
Western Ontario and McMaster Universities Osteoarthritis Index
As seen by the network meta-analysis, compared to the control group (Taiji), Baduanjin exercises (MD = –9.93, CL = (–16.77, –3.08)) was a better choice in terms of reducing WOMAC scores. Relative to the control group (retro walking), yoga (MD = –6.10, CL = (–11.95, –0.24)) was more effective in reducing WOMAC scores. Compared to the control group (balance training), Baduanjin exercises (MD = –10.32, CL = (–16.95, –3.68)) and yoga (MD = –6.49, CL = (–12.10, –0.88)) were more advantageous in reducing WOMAC scores. Compared to the control group (Pilates), Baduanjin exercises (MD = –12.03, CL = (–18.55, –5.51)) and yoga (MD = –8.20, CL = (–13.67, –2.72)) and balance training (MD = –1.71, CL = (–3.33, –0.09)) were superior in terms of lowering WOMAC scores. Compared with the control group (forward walking), Baduanjin exercises (MD = –12.03, CL = (–18.96, –5.09)) and yoga (MD = –8.20, CL = (–14.16, –2.23)) were more appropriate in reducing WOMAC scores. Relative to the control group (Yijinjing), Baduanjin exercises (MD = –14.38, CL = (–21.93, –6.83)) was superior to the control group in terms of reducing WOMAC scores. Compared to the control group (CBT), Baduanjin exercises (MD = –13.04, CL = (–15.94, –10.13)) and yoga (MD = –9.20, CL = (–14.94, –3.47)) and Taiji (MD = –5.77, CL = (–11.53, –0.01)) were more appropriate in reducing WOMAC scores. Relative to the control group (Daily Nurse), Baduanjin exercises (MD = –13.34, CL = (–16.13, –10.54)) and yoga (MD = –9.50, CL = (–15.18, –3.83)) and Taiji (MD = –6.07, CL = (–11.77, –0.37)) were more effective in lowering WOMAC scores. Relative to the control group (Daily Exercise), Baduanjin exercises (MD = –13.43, CL = (–19.91, –6.95)) and yoga (MD = –9.60, CL = (–15.02, –4.17)) and retro walking (MD = –3.50, CL = (–5.71, –1.29)) and balance training (MD = –3.11, CL = (–4.55, –1.67)) and Pilates (MD = –1.40, CL = (–2.14, –0.66)) were more advantageous in reducing WOMAC scores. Compared to the control group (Wuqinxi), Baduanjin exercises (MD = –7.27, CL = (–13.61, –0.92)) and yoga (MD = –10.55, CL = (–17.21, –3.88)) were superior to the control group in terms of reducing WOMAC scores. Relative to the control group (MBSR), Baduanjin exercises (MD = –21.34, CL = (–34.84, –7.83)) and yoga (MD = –17.50, CL = (–31.88, –3.13)) were better choices in terms of reducing WOMAC scores. The probability ranking of the different mind-body interventions in terms of lowering WOMAC scores was ranked first by Baduanjin exercises in the SUCRA (SUCRA: 98.3% as shown in Figure 3 A). A comparison between the 2 different interventions is shown in Table III A.
Figure 3
A – SUCRA plot for WOMAC, B – SUCRA plot for TUG, C – SUCRA plot for MHC, D – SUCRA plot for PHC

Table III
A – League table of Western Ontario and McMaster Universities Osteoarthritis Index
Timed up and go
As seen by the network meta-analysis, compared to the control group (retro walking), balance training (MD = –1.04, CL = (–1.88, –0.20)) was more advantageous in terms of reducing TUG scores. Compared to the control group (forward walking), balance training (MD = –1.34, CL = (–2.16, –0.52)) and retro walking (MD = –0.30, CL = (–0.55, –0.05)) were more effective in reducing TUG scores. Relative to the control group (yoga), balance training (MD = –1.54, CL = (–2.69, –0.39)) showed an advantage in reducing TUG scores. Compared to the control group (daily Exercise), balance training (MD = –1.44, CL = (–2.24, –0.64)) and retro walking (MD = –0.40, CL = (–0.65, –0.15)) were more effective in reducing TUG scores. To reduce TUG scores, balance training (MD = –354, CL = (–5.85, –1.23)) and retro walking (MD = –2.50, CL = (–4.68, –0.32)) and forward walking (MD = –2.20, CL = (–4.37, –0.03)) should be selected more than the control group (daily nurse). The probability ranking of the different mind-body interventions in terms of lowering TUG scores was ranked first by balance training in the SUCRA (SUCRA: 99.4%, as shown in Figure 3 B). A comparison between the 2 different interventions is shown in Table III B.
B
– League table of Timed Up and Go test
Mental Health Component (MHC) of SF-36
As seen by the network meta-analysis, compared to the control group (daily nurse), MBSR (MD = 8.90, CL = (2.33, 15.47)) was more effective in improving the MHC of SF-36. Relative to the control group (meditation), MBSR (MD = 18.70, CL = (10.08, 27.32)) and balance training (MD = 15.75, CL = (6.78, 24.71)) and daily nurse (MD = 9.80, CL = (4.22, 15.38)) were more likely to give options for improving MHC of SF-36. The probability ranking of the different mind-body interventions in terms of improving the MHC of SF-36 was ranked first by MBSR in the SUCRA (SUCRA: 87.9%, as shown in Figure 3 C). A comparison between the 2 different interventions is shown in Table III C.
C
– League table of the Mental Health Component of the 36-Item Short Form Health Survey
Physical Health Component of SF-36
As seen by the network meta-analysis, compared to the control group (daily nurse), balance training (MD = 12.24, CL = (5.99, 18.48)) was a better choice than the control group in terms of improving the PHC of SF-36. Compared with the control group (meditation), balance training (MD = 14.40, CL = (6.76, 22.03)) was more effective in improving the PHC of SF-36. Relative to the control group (MBSR), balance training (MD = 15.14, CL = (6.61, 23.66)) was a better choice than the control group in terms of improving the PHC of SF-36. The probability ranking of the different mind-body interventions in terms of improving PHC of SF-36 was ranked first by MBSR in the SUCRA (SUCRA: 90.3%, as shown in Figure 3 D). A comparison between the 2 different interventions is shown in Table III D.
D
– League table of the Physical Health Component of the 36-Item Short Form Health Survey
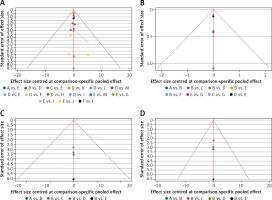
Publication bias test
We drew funnel plots for the different outcome indicators separately, and some plots show that the scattered points of each study are on both sides of the funnel plot and are roughly symmetrically distributed, suggesting that the risk of publication bias in this study is lower [44], as shown in Figures 4 A–D.
Discussion
In this study, we evaluated the effects of several mind-body interventions given to KOA patients. There were 859 KOA patients, 17 studies in total, and 13 distinct types of mind-body therapies. According to our research, balance training is a good mind-body exercise for lowering TUG scores, Baduanjin exercises may be a good option for lowering the WOMAC index, MBSR produced better results for raising the SF-36’s MPC, and balance training is one of the exercise modalities to consider for raising the SF-36’s PHC.
KOA can cause symptoms such as pain, stiffness, and loss of function, and is a high-risk factor for disability in the elderly [45]. The WOMAC is a standardized questionnaire that has been widely used to assess the physical condition of patients with KOA in 3 areas: pain, stiffness, and function [46]. Our study showed that among the 13 mind-body therapies, Baduanjin exercises are quite effective in reducing WOMAC in patients with KOA. This is similar to the findings of Zhi-peng Zeng, Fenglan Wang, and Ruojin Li, and the study demonstrated that Baduanjin is a safe and effective exercise program for intervention in KOA [17, 47,48]. In addition, Kevin Ki-Wai Ho’s study applied Baduanjin to 112 patients with KOA in the community, and after 6 months the patients had a significant reduction in WOMAC without any adverse events [46]. AN Bing-Chen found in a follow-up study of 28 patients with KOA, who consistently participated in Baduanjin exercises, that the patients showed significant improvements in all 3 aspects of WOMAC (pain, stiffness, and function) after 1 year and that for KOA patients Baduanjin exercises were a safe and viable option [49]. Jiao Liu randomized 140 patients with knee osteoarthritis into 4 groups of Taiji, Baduanjin, stationary cycling, and health education to participate in a 12-week intervention, with 108 patients eventually completing the study, and their study saw that Baduanjin exercises could alter the resting-state functional connectivity of the brain in KOA patients [50]. In addition, another of Jiao Liu’s studies found that KOA patients showed an increase in multiple resting-state functional connectivity within the brain after participating in the Baduanjin exercises [51]. Baduanjin exercises, a traditional from of Chinese exercise dating back more than 2500 years, was named Baduanjin because it contains 8 different movements [52]: “two hands hold up the heaven”, “drawing the bow to shoot the eagle”, “separating heaven and earth”, “wise owl gazes backwards”, “swaying the head and shaking the tail”, “two hands hold the feet”, “clenching the first and glaring fiercely”, and “bouncing on the toes” are the 8 movements performed [53]. Each movement of the Baduanjin exercises emphasizes the interplay between body and mind, with slow movements accompanied by deep breathing and slow muscle stretching with mental concentration; its effectiveness has been proven in patients with a variety of diseases, and it is widely accepted and recognized by the public [52, 54–56]. In practice, each movement needs to be repeated several times. Exercise training is a physical therapy that can be used as a supplement to medication or surgery. For KOA patients, adherence to exercise training can slow the degeneration of cartilage, inhibit inflammation, and slow the loss of subchondral bone and epiphyseal trabeculae [13]. Baduanjin exercises are increasingly being used as a gentle and safe mind-body therapy for patients with KOA.
Reduced muscle strength, loss of bodily function, and loss of proprioception are common in KOA patients. These modifications could be brought on by articular cartilage degeneration and mechanoreceptor dysfunction, and these impairments reduce neuromuscular control, decreasing the patient’s mobility and raising the chance of a fall [57]. The Timed Up and Go (TUG) test has been endorsed by the Centres for Disease Control and Prevention (CDC) as a tool to assess patient gait, strength, and balance, to further assess the risk of falls in older patients [58]. Balance training is necessary for patients with KOA who are at high risk of falls; it reduces the risk of falls in patients with KOA [57, 59]. Our study showed that balance training is a good mind-body exercise in reducing TUG scores. This is similar to the findings of Chun-De Liao et al. [60] and Javed et al. [61]. Takacs’s study also showed that balance training significantly improved patients’ fear of exercise [62]. There is some disagreement with the findings of Anderson et al., which may be related to the inconsistency between our study population and the study objectives [63]. The main objective of the study by Anderson et al. was to investigate the effectiveness of balance training as a preoperative intervention for total knee arthroplasty. Balance training may help patients reverse muscle atrophy, restore body function, and maintain balance performance, therefore reducing the risk of falls in patients with KOA [64, 65].
The long duration of KOA not only damages the physiological function of the patient but also increases the psychological burden and reduces the quality of life of the patient. The 36-Item Short Form Health Survey questionnaire is a commonly used tool to assess patients’ health-related quality of life. The SF-36 contains 2 different concepts, one for the physical dimension of patients, represented by the Physical Health Component (PHC), and the other for the mental dimension of patients, represented by the Mental Health Component (MHC) [66]. Our study showed that MBSR is a good mind-body exercise in increasing the MHC of SF-36. Our findings are consistent with Marais’s study [39]. In addition, Marais et al. [39] found no difference in pain relief between patients in the MBSR group and those in the usual care group at baseline and 3 months, but patients in the MBSR group had a higher degree of pain relief. At baseline and 6 months, patients in the MBSR group had better pain relief than those in the usual care group, which was statistically significant. However, in practice, there was no difference in pain medication use between the 2 groups. Mindfulness-based interventions can manage patient pain, depressed mood, and health-related anxiety and are an effective option for chronic patients. Its effectiveness has been demonstrated in patients with multiple types of chronic diseases [67]. In addition, we found that balance training is a good mind-body exercise for increasing the PHC of SF-36. This is similar to the findings of Arghavani et al. [68]. This may be related to previous studies showing that balance training can help patients reverse muscle atrophy, restore physical function, maintain balance performance, help patients reduce the risk of falls, and build confidence in life, thus further improving patients’ physical health [64, 65].
Although we wanted to ensure the rigor of our study as much as possible, there are still some limitations. First, there are several scales used to assess the functional status of the knee in KOA patients, such as the WOMAC, the Knee Injury and Osteoarthritis Outcome Score (KOOS) [69], the Knee Society Score (KSS) [70], and others. In this study, a meta-analysis was conducted using WOMAC as the outcome variable. After screening according to our literature search strategy inclusion and exclusion criteria, WOMAC was mostly used as an outcome variable in the final included literature. Therefore, we were unable to analyse and validate multiple perspectives on the outcome variable of knee functional status. Second, due to the limitations of the current number of studies, there was a different distribution of the number of trials in our analysis. We used the consistency test and inconsistency test during our software analysis, and the results may be subject to some risk of bias. Therefore, in the future, we also hope that there will be more relevant studies that will allow us to validate the trial results again on the basis of multicentre and large samples.
Overall, our study has several practical applications, most notably that patients with KOA may benefit from either Baduanjin exercises, balance training, or MBSR. Additionally, when treating KOA patients, medical personnel can include mind-body therapies as a complement to pharmaceutical treatment approaches, enhancing the therapeutic strategy and maximizing patient outcomes.
In conclusion, significant research has proven the efficacy of mind-body therapies for KOA patients, and we advise choosing Baduanjin exercises to enhance WOMAC, balance training to improve TUG, and MBSR or balance training to improve SF-36. Finally, depending on the clinical settings and unique patient characteristics, the medical team can create scientific and individualized treatment regimens for patients.