Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Section Editors
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
GENERAL SURGERY / SYSTEMATIC REVIEW/META-ANALYSIS
Effects and safety of intraoperative intermittent pneumatic compression for preventing postoperative venous thromboembolism: a meta-analysis
1
Department of Nursing, The First People’s Hospital of Lianyungang, The Affiliated Lianyungang Hospital of Xuzhou Medical University, Jiangsu, China
Submission date: 2021-08-05
Final revision date: 2021-11-09
Acceptance date: 2021-11-20
Online publication date: 2021-11-21
Corresponding author
Jianhua Li
Department of Nursing, The First People’s Hospital of Lianyungang, The Affiliated Lianyungang Hospital of Xuzhou Medical University, 182 Tongyu North Road, Haizhou District, Lianyungang, Jiangsu Province, China, Phone: 12815194604, Fax: 0024 0681 1026
Department of Nursing, The First People’s Hospital of Lianyungang, The Affiliated Lianyungang Hospital of Xuzhou Medical University, 182 Tongyu North Road, Haizhou District, Lianyungang, Jiangsu Province, China, Phone: 12815194604, Fax: 0024 0681 1026
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Intermittent pneumatic compression (IPC) has been used for venous thromboembolism (VTE) prevention. It is necessary to evaluate the effects and safety of intraoperative use of IPC devices in the prevention of VTE in surgical patients.
Material and methods:
Two authors independently searched the PubMed, Cochrane Library, MEDLINE, Embase, China National Knowledge Infrastructure (CNKI), and Wanfang databases for randomized controlled trials (RCTs) and cohort studies on the use of IPC in surgical patients up to June 10, 2021. The Cochrane Collaborations risk of bias tool and the Newcastle-Ottawa Scale (NOS) were used for quality assessment. RevMan 5.3 software was used for statistical analyses.
Results:
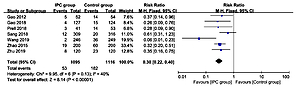
A total of 13 studies including seven RCTs and six retrospective cohort studies involving 6673 surgical patients were included; 1883 patients underwent IPC intervention. The synthesized RCT results indicated that IPC was beneficial to reduce the incidence of deep vein thrombosis (DVT) (RR = 0.30, 95% CI: 0.22–0.40, p < 0.001) and VTE (RR = 0.51, 95% CI: 0.27–0.95, p = 0.03). The synthesized results from retrospective cohort studies indicated that IPC is beneficial to reduce the incidence of DVT (RR = 0.63, 95% CI: 0.42–0.96, p = 0.03) and PE (RR = 0.34, 95% CI: 0.16–0.72, p = 0.005). No significant publication bias was found for any synthesized outcomes (all p > 0.05).
Conclusions:
IPC seems to be safe and effective in the prevention and management of intraoperative VTE. Limited by study sample size, this conclusion still needs to be further confirmed by large-sample, multi-center, high-quality clinical studies.
Intermittent pneumatic compression (IPC) has been used for venous thromboembolism (VTE) prevention. It is necessary to evaluate the effects and safety of intraoperative use of IPC devices in the prevention of VTE in surgical patients.
Material and methods:
Two authors independently searched the PubMed, Cochrane Library, MEDLINE, Embase, China National Knowledge Infrastructure (CNKI), and Wanfang databases for randomized controlled trials (RCTs) and cohort studies on the use of IPC in surgical patients up to June 10, 2021. The Cochrane Collaborations risk of bias tool and the Newcastle-Ottawa Scale (NOS) were used for quality assessment. RevMan 5.3 software was used for statistical analyses.
Results:
A total of 13 studies including seven RCTs and six retrospective cohort studies involving 6673 surgical patients were included; 1883 patients underwent IPC intervention. The synthesized RCT results indicated that IPC was beneficial to reduce the incidence of deep vein thrombosis (DVT) (RR = 0.30, 95% CI: 0.22–0.40, p < 0.001) and VTE (RR = 0.51, 95% CI: 0.27–0.95, p = 0.03). The synthesized results from retrospective cohort studies indicated that IPC is beneficial to reduce the incidence of DVT (RR = 0.63, 95% CI: 0.42–0.96, p = 0.03) and PE (RR = 0.34, 95% CI: 0.16–0.72, p = 0.005). No significant publication bias was found for any synthesized outcomes (all p > 0.05).
Conclusions:
IPC seems to be safe and effective in the prevention and management of intraoperative VTE. Limited by study sample size, this conclusion still needs to be further confirmed by large-sample, multi-center, high-quality clinical studies.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.